The incidence of melanoma has increased considerably over the last few decades. In fact, according to the World Health Organization (WHO), the number of melanoma cases worldwide has continued to rise at a rate that exceeds that of any other form of cancer.1 GLOBOCAN estimates indicate that 41,400 newly diagnosed cases of melanoma and 10,800 related deaths were reported throughout the EU in 2000.2 Corresponding numbers for the US in 2007 are 59,940 cases and 8,110 deaths.3 Survival prospects for patients with advanced melanoma have not improved in more than 30 years, with median survival times ranging from six to nine months.4,5 Overall, clinical data have not shown any one therapeutic regimen to be superior to another in the treatment of this intractable disease, and single-agent chemotherapy with dacarbazine remains the only reference standard.6,7
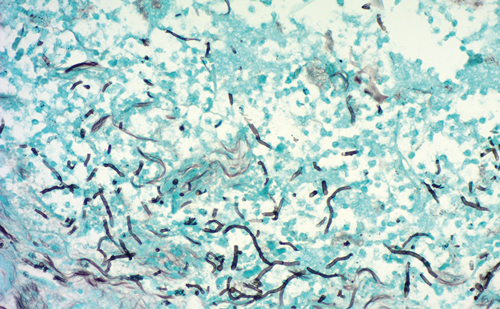
Multiple cellular pathways are activated in melanoma via specific mutations or changes in expression levels of various proteins.8 One important pathway that regulates apoptosis is mediated by Bcl-2, and this pathway represents a potential therapeutic target. Bcl-2 is an antiapoptotic protein that obstructs the mitochondrial release of cytochrome C and consequently inhibits the activation of caspase-9, a critical mediator of cell death.9 Bcl-2 expression has been reported in 90% of all cases of human melanoma.10 Aberrant expression of Bcl-2 partially explains melanoma cell survival and resistance to standard chemotherapy.9,11
Oblimersen sodium (Genasense®, Genta Inc., New Jersey, US), an 18-base phosphorothioate antisense oligonucleotide, selectively binds to the first six codons of the human bcl-2 mRNA open-reading frame, leading to RNA degradation and, in turn, suppression of Bcl-2 translation. In both clinical and pre-clinical settings, oblimersen has been shown to effectively downregulate the Bcl-2 protein and may have the potential to augment the apoptotic effects of chemotherapy in advanced melanoma.10–13
Notably, oblimersen was found to improve response rates in a dose-finding study with dacarbazine, with an associated decrease in Bcl-2 based on serial tumour biopsies.12
This article highlights recent phase III data supporting the use of oblimersen with dacarbazine in advanced melanoma and, in particular, the substantial prognostic impact of baseline serum lactate dehydrogenase (LDH) levels on overall survival (OS) observed among the study’s patient population. The strong therapeutic rationale for prospectively assessing the efficacy of this agent among patients with low baseline LDH in an ongoing oblimersen study in advanced melanoma is discussed. Current investigations seek to optimise oblimersen’s antitumour activity in patients who would most likely benefit from the addition of this agent to chemotherapy.
Study GM301
A stratified, randomised, open-label phase III trial of dacarbazine with or without oblimersen was conducted among 771 chemotherapy-naïve patients with advanced melanoma.14 Patients received either five days of oblimersen at a dose of 7mg/kg/day by continuous intravenous (IV) infusion followed by dacarbazine 1,000mg/m2 intravenously or the same dose of dacarbazine alone. An important stratification factor was baseline serum LDH level, which was recently recognised as a basis for classifying patients into the category of M1c (patients with metastasis to all other visceral sites or disant metastasis at any site associated with an elavated LDH) in the new American Joint Committee of Cancer (AJCC) staging system for melanoma.15
Based on an intent-to-treat analysis, the combination of oblimersen plus dacarbazine yielded a trend towards improvement in the primary end-point of OS at 24-month minimum follow-up (median 9.0 versus 7.8 months; p=0.077). Significant findings in favour of the combination therapy were evident for OR rate (13.5 versus 7.5%; p=0.007), durable response rate (7.3 versus 3.6%; p=0.03) and progression-free survival (PFS) (hazard ratio 0.75; p=0.0007).14,16
Safety analyses revealed that grade 3/4 neutropoenia and thrombocytopoenia were the most important adverse events.14 The incidence of grade 3/4 neutropoenia with infection was slightly increased in the oblimersen–dacarbazine group (4.3%) compared with dacarbazine alone (2.8%). The incidence of bleeding events was also increased in the oblimersen–dacarbazine group (13.7 versus 9.2%). However, these events were largely grade 1/2. In fact, the incidence of grade 3/4 bleeding events was slightly less in the oblimersen–dacarbazine group (2.2%) than in the dacarbazine alone group (3.1%). A small percentage of patients in both groups discontinued study therapy due to a treatment-related adverse event (oblimersen–dacarbazine group 6.2%, dacarbazine alone group 2.2%).14
One of the end-points in this trial was PFS, a parameter that is increasingly being assessed as a primary end-point in clinical trials in oncology, although unequivocal determination of the timing of progression is problematic.17 Various statistical approaches are employed to minimise potential biases in PFS estimation and to increase the reliability of this time-to-event end-point. In Study GM301, multiple sensitivity analyses were conducted and confirmed the robust nature of the PFS data.14 In a separate analysis, PFS data were further evaluated using a simulation model that included realistic assumptions about the actual pattern of assessment times in Study GM301.18 Results of this analysis showed that the observed treatment difference in PFS could not be explained by assessment bias.18
The Importance of Baseline Serum Lactate
Dehydrogenase – Additional Analyses of Study GM301 Elevated LDH is considered to be the most important independent negative prognostic indicator in advanced melanoma. A statistically significant interaction between treatment effect and baseline LDH was identified in Study GM301, and multivariate analyses adjusting for baseline prognostic factors confirmed this interaction.14 The therapeutic benefit of oblimersen plus dacarbazine was most evident among patients with normal LDH (i.e. baseline LDH ≤1.1 times the upper limit of normal [x ULN], as defined in the protocol). The combination therapy was statistically significantly superior to dacarbazine alone for all efficacy end-points analysed (including OS) among patients with normal LDH (see Table 1), whereas no significant differences between treatment groups were apparent among patients with elevated LDH (i.e. baseline LDH >1.1 x ULN). Notably, among patients with normal LDH, OS was significantly increased with the oblimersen–dacarbazine regimen compared with dacarbazine alone (11.4 versus 9.7 months; p=0.02).14 It appears from these analyses that not only is LDH a key stratification factor, but it can also be used to identify those patients in whom the oblimersen–dacarbazine regimen would provide the most therapeutic benefit.14 Of note, downregulating Bcl-2 may not be effective in patients with elevated baseline LDH. This is perhaps due, in part, to drug-resistance mechanisms other than Bcl-2 overexpression.14
When used in disease-staging systems and as a stratification factor, LDH is often categorised as ‘normal’ or ‘elevated’ based on intuitive or pragmatic cut-off points. Historically, the worst survival has been associated with the ‘elevated’ LDH category. In light of the findings in Study GM301, the appropriateness of the protocol-specified LDH cut-off value of 1.1 was analysed.19 Baseline LDH value was analysed as a continuous variable to determine its prognostic importance and to assess the possible interaction between treatment effect and LDH. In addition, data from another large, randomised, open-label phase III study in advanced melanoma conducted by the European Organisation for Research and Treatment of Cancer (EORTC) Melanoma Group (EORTC Study 18951)20 were similarly and independently analysed. The two studies had similar eligibility criteria.
Five LDH categories were derived based on previously used or reported cut-off points.19 In both studies, more patients had a baseline LDH value close to the ULN (i.e. within the range of 0.8–1.1 x ULN) than in the general population.21 This observation suggests the existence of biological differences among patients with advanced melanoma and an increase in the true normal baseline LDH in this setting, which may signal early aggressive disease.21
In the analysis of Study GM301, survival in advanced melanoma was predicted by LDH category over a wide range of median survival values and in a highly ordered manner (see Figure 1).21 Pre-treatment LDH value was of strong and incremental prognostic importance (overall p<0.0001). Minor variations in baseline LDH around the ULN had a substantial prognostic impact on survival in advanced melanoma, and survival was substantially worse as baseline LDH increased, regardless of whether or not the LDH value remained within the normal reference range.19,21
Analysis of EORTC Study 18951 corroborated these findings (see Figure 2).19,21 In Study GM301, a continuous and monotonic relationship was observed between treatment outcome and LDH (see Table 2).21 Maximum benefit from oblimersen plus dacarbazine was achieved in the subgroup of patients with LDH ≤0.8 x ULN (the lowest LDH category analysed) across all efficacy end-points, including OS, reflecting a more favourable disease course and biology.19,21
Among patients with a baseline LDH of ≤0.8 x ULN, median OS was 12.3 months with the oblimersen–dacarbazine regimen versus 9.9 months with dacarbazine alone (p=0.0009).21 The two-year survival rate among patients with baseline LDH ≤0.8 x ULN was 27% (95% confidence interval [CI] 20.6–34.8) with oblimersen plus dacarbazine and 12% (95% CI 7.3–19.0) with dacarbazine alone.21 The Kaplan-Meier curves separated from the start, suggesting that this population was more homogenous with respect to treatment effect than patients with LDH ≤1.1 x ULN (data not shown).
The Randomized, Double-blind, Placebo-controlled Trial of Genasense® plus Dacarbazine versus Dacarbazine Alone In Advanced Melanoma
In view of the above retrospective analyses, the Randomized Double-Blind, Placebo-controlled Trial of Genasense® Plus Dacarbazine versus Dacarbazine Alone In Advanced Melanoma (AGENDA) Trial (study GM307) was initiated to prospectively assess the efficacy of the same regimen of oblimersen plus dacarbazine as administered in study GM301 in chemotherapy-naïve patients with advanced melanoma and low LDH.22 Primary efficacy analyses will assess oblimersen’s effect on PFS and OS. In this ongoing double-blind phase III study, eligible patients are randomised to treatment with oblimersen plus dacarbazine or placebo plus dacarbazine at dosages identical to those in study GM301. However, unlike Study GM301, enrolment is limited to patients most likely to benefit from the addition of oblimersen (those with baseline LDH ≤0.8 x ULN). As the timing of outcome assessments may affect estimation of PFS and other time-to-event end-points, uniform evaluation schedules between treatment groups were selected to minimise the chance of biased results.
Additional Research
Pre-clinically, intra-tumoral uptake and retention of oblimersen is enhanced with administration by short IV infusion. A dose-escalation study of the safety and pharmacokinetics of oblimersen administered as a weekly two-hour infusion for three weeks is ongoing in patients with advanced solid tumours.23 Oblimersen has been safely administered in this manner at weekly doses of up to 1,000mg. Although not considered, dose-limiting, fever, chills and slight decreases in blood pressure occurred at the 1,000mg dose level (particularly with the first infusion).23 Prophylactic administration of corticosteroids prior to oblimersen and administration of oblimersen as a twice-weekly short IV infusion are being studied. Pre-clinical models demonstrate a synergistic effect with a combination of oblimersen, temozolomide and an albumin-bound formulation of paclitaxel, warranting further exploration. A phase I safety, pharmacokinetic and pharmacodynamic study of this combination is ongoing in chemotherapy-naïve patients with advanced melanoma and normal LDH.24
Based on preliminary results for six patients, Grade 3–4 adverse events were limited to neutropoenia and thrombocytopoenia, which each occurred in one patient. Decreases in Bcl-2 levels were apparent.24
Summary
Advances in our understanding of melanoma biology and continued oblimersen research may lead to enhanced therapeutic approaches with this agent. In the GM301 study,14 oblimersen combined with dacarbazine compared with dacarbazine alone yielded a significantly better result for OS among patients who had baseline LDH categorised as normal (≤1.1 x ULN).Recent analyses of clinical data demonstrate that small variations in LDH below the ULN have a considerable prognostic effect on survival in advanced melanoma. The addition of oblimersen to standard dacarbazine therapy is currently being investigated in the AGENDA trial among patients with low LDH (≤0.8 x ULN) and may prove to be advantageous in improving survival in this population. ■
Current Status of Oblimersen (Bcl-2 Antisense) Therapy for Advanced Melanoma
Article:
References
- Lens MB, Dawes M, Global perspectives of contemporary epidemiological trends of cutaneous malignant melanoma, Br J Dermatol, 2004;150:179–85.
- Incidence and mortality in the European Union. https://info.cancerresearchuk.org/cancerstats/geographic/canceri neu/incidence and mortality, 2007.
- Jemal A, Siegel R, Ward E, et al., Cancer statistics, 2007, CA Cancer J Clin, 2007;57:43–66.
- Serrone L, Zeuli M, Sega FM, et al., Dacarbazine-based chemotherapy for metastatic melanoma: Thirty-year experience overview, J Exp Clin Cancer Res, 2000;19:21–34.
- Atkins MB, Cytokine-based therapy and biochemotherapy for advanced melanoma, Clin Cancer Res, 2006;12:2353–58s.
- Eggermont AMM, Reaching first-base in the treatment of metastatic melanoma, J Clin Oncol, 2006;24:4673–4.
- Flaherty KT, Chemotherapy and targeted therapy combinations in advanced melanoma, Clin Cancer Res, 2006;12:2366–70s.
- Sosman JA, Puzanov I, Molecular targets in melanoma from angiogenesis to apoptosis, Clin Cancer Res, 2006;12: 2376s–83s.
- Soengas MS, Lowe SW, Apoptosis and melanoma chemoresistance, Oncogene, 2003;22;3138–51.
- Jansen B, Schlagbauer-Wadl H, Brown BD, et al., Bcl-2 antisense therapy chemosensitises human melanoma in SCID mice, Nat Med, 1998;4:232–4.
- Klasa RJ, Gillum AM, Klem RE, Frankel ST, Oblimersen Bcl-2 antisense: Facilitating apoptosis in anticancer treatment, Antisense Nucleic Acid Drug Dev, 2002;12:193–213.
- Jansen B, Wacheck V, Heere-Ress E, et al., Chemosensitisation of malignant melanoma by BCL2 antisense therapy, Lancet, 2000;356:1728–33.
- Jansen B, Wacheck V, Heere-Reese E, et al., Clinical, pharmacological and pharmacodynamic study of Genasense (G3139, Bcl-2 antisense oligonucleotide) and dacarbazine (DTIC) in patients with malignant melanoma, Proc Am Soc Clin Oncol, 2001;20: abstract 1426.
- Bedikian AY, Millward M, Pehamberger H, et al., Bcl-2 antisense (oblimersen sodium) plus dacarbazine in patients with advanced melanoma: The Oblimersen Melanoma Study Group, J Clin Oncol, 2006;24:4738–45.
- Balch CM, Buzaid AC, Soong S-J, et al., Final version of the American Joint Committee on Cancer staging system for cutaneous melanoma, J Clin Oncol, 2001;19:3635–48.
- Kay R, Gilles E, Wu J, Agarwala SS, Progression-free survival (PFS) with an oblimersen-dacarbazine (OBL-DTIC) regimen in advanced melanoma: PFS difference is not explained by assessment asymmetry, 4th Int. Melanoma Congress, 2007.
- Panageas KS, Ben-Porat L, Dickler MN, et al., When you look matters: The effect of assessment schedule on progression-free survival, J Natl Cancer Inst, 2007;99:428–32.
- Gilles E, Kay R, Wu J, Agarwala SS, Progression-free survival (PFS) with an oblimersen-dacarbazine (OBL-DTIC) regimen in advanced melanoma: PFS dierence [sic] is not explained by assessment asymmetry, Proc Int Melanoma Congress, 2007;20:540, abstract T-33.
- Keilholz U, Suciu S, Bedikian AY, et al., LDH is a prognostic factor in stage IV melanoma patients (pts) but is a predictive factor only for bcl2 antisense treatment efficacy: Re-analysis of GM301 and EORTC 18951 randomised trials, Proc Am Soc Clin Oncol, 2007;25:485s, abstract 8552.
- Keilholz U, Punt CJA, Gore M, et al., Dacarbazine, cisplatin and interferon-alfa-2b with or without interleukin-2 in metastatic melanoma: A randomised Phase III trial (18951) of the European Organisation for Research and Treatment of Cancer Melanoma Group, J Clin Oncol, 2005;23:6747–55.
- Keilholz U, Suciu S, Bedikian AY, et al., LDH is a prognostic factor in stage IV melanoma patients (pts) but is a predictive factor only for bcl2 antisense treatment efficacy: Re-analysis of GM301 and EORTC 18951 randomised trials, 43rd Annual Meeting of the Am Soc Clin Oncol (ASCO); 2007.
- Bedikian AY, Agarwala SS, Gilles E, et al., The AGENDA study: A randomised, double-blind study of Genasense plus dacarbazine (DTIC) in chemotherapy-naïve patients with advanced melanoma and low LDH, Proc Int Melanoma Congress, 2007;20:538, abstract T-26.
- Tolcher A, Julian T, Qureshi A, Oblimersen (OBL; Genasense(r)), a phosphorothioate (PS) Bcl-2 antisense oliogonucleotide (ASO), can be safely administered by bolus subcutaneous (SC) injection and brief IV infusion, Proc Am Soc Hematol, 2007;110:254–5B.
- Pavlick A, Volm M, Ryan T, et al., A phase I study of the triple combination of oblimersen (OBL), temozolomide (TMZ) and Abraxane (ABX) in patients with advanced melanoma and normal LDH, Proc Int Melanoma Congress, 2007;20:542.