touchEXPERT OPINIONS Appropriate use of opioids to address cancer-related pain
Three pain specialists consider the use of opioids for the management of cancer-related pain.
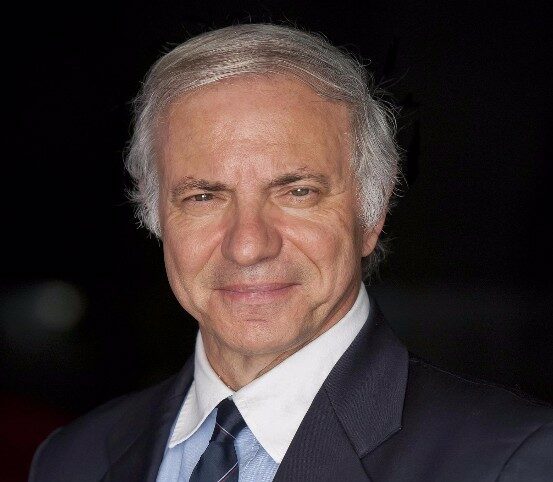
Prof. Sebastiano Mercadante outlines the pathophysiology of cancer-related pain and how it can be assessed in clinical practice. He also considers current guidelines for its management, including the role of opioids.
1/3 Next InterviewIn this interview, Prof. Mercadante answers the following questions:
- What are the key chronic pain syndromes that can result from cancer?
- How do you screen patients for pain resulting from malignancy or cancer treatments?
- How should current guidelines for the management of cancer-related pain be applied in practice?
- What are the principles of opioid titration for the management of cancer-related pain?
- What are the principles of opioid switching and dose conversion for the treatment of cancer-related pain?
Prof. Sebastiano Mercadante is director of pain and supportive care, hospice and anesthetics at La Maddalena Cancer Center in Palermo, Italy. He is also a professor of anesthesiology, intensive care and pain therapy. read more
Prof. Mercadante is also an adjunct professor of palliative medicine at the University of Texas, Houston, TX, USA, and a member of the national ministerial commission for pain and palliative care.
Prof. Mercadante is associate editor, editorial board member and/or referee for over 30 international peer-reviewed journals in the field of pain, symptom management and anaesthesiology. He has over 500 papers published in international, peer-reviewed journals, and has given over 600 lectures at national and international congresses.
Prof. Mercadante has received multiple awards, including the John Mendelson MD Award from the University of Texas MD Anderson Cancer Center for extraordinary contribution in palliative care.
Prof. Sebastiano Mercadante discloses: Advisory board/consultancy fees from Kyowa Kyrin and Molteni.
Prof. Marie Fallon summarizes the possible adverse effects of opioids and considers strategies to manage them, including adjustments to the opioid treatment and therapeutic options.
2/3 Next InterviewIn this interview, Prof. Fallon answers the following questions:
- What adverse effects may be associated with the use of opioids for cancer-related pain?
- What is best practice for assessing a patient’s risk of opioid-induced side effects?
- When should opioid adjustments be considered in patients with cancer in order to manage side effects?
- What therapeutic options can be considered to manage opioid-induced side effects?
- Which newer analgesic approaches may have fewer side effects than opioids?
Prof. Marie Fallon is chair of palliative medicine at the University of Edinburgh, Edinburgh, UK. She leads the largest portfolio of multicentre clinical trials in palliative care in the UK, specializing in symptoms such as cancer cachexia and cancer pain control. read more
Prof. Fallon is joint editor of the Oxford Textbook of Palliative Medicine (4th, 5th and 6th editions), and has served as editor of the ABC of Palliative Care (two editions), the ABC of Pain and the Textbook of Cancer Pain. She also sits on the editorial board of BMJ Supportive and Palliative Care.
Prof. Fallon is a co-director of the European Palliative Care Research Centre, Oslo, Norway. She is on the scientific committees for several international conferences, including the European Association for Palliative Care (EAPC), the European Palliative Care Research Collaborative (EPCRC), the Cachexia Society and the European Society for Medical Oncology (ESMO).
Prof. Marie Fallon discloses: Advisory board/consultancy fees from Fitabeo Therapeutics, Huddersfield Pharmacy Specials and Pfizer/Lilly.
Prof. Frank Elsner outlines strategies to ensure the safe use of opioids in patients with cancer-related pain, including guidance on assessing patients prior to therapy initiation and monitoring patients on treatment.
3/3 Leave FeedbackIn this interview, Prof. Elsner answers the following questions:
- What are the key points for clinicians regarding the safe use of opioids?
- What universal precautions can be taken to minimize the possible adverse consequences of opioid use?
- How should patients at risk of opioid use disorder be identified?
- What is best practice regarding monitoring patients for potential opioid dose reduction or discontinuation?
Prof. Frank Elsner is vice chair and assistant medical director of the Department of Palliative Medicine at the University Hospital of RWTH Aachen University, Aachen, Germany. read more
Prof. Elsner is chair of the steering group on Medical Education and Training for the European Association for Palliative Care (EAPC). He participates in multiple international research collaborations, including with the Marie Curie Palliative Care Institute, the University of Navarra and Peking University.
Prof. Elsner has contributed over 170 publications in this field, including original articles, reviews/editorials and book chapters.
Prof. Frank Elsner discloses: Lecture/advisory board fees from Ethypharm, Grünenthal, Hexal, Menarini – Berlin Chemie and TEVA.
Overview & Learning Objectives
Overview
In this activity, three pain experts share their perspectives on the use of opioids in cancer-related pain, including assessment and management of cancer-related pain, considerations for a patient receiving treatment with an opioid and the prevention of opioid misuse.
Learning Objectives
After watching this activity, participants should be better able to:
- Appraise current best practice for the management of cancer-related pain
- Apply active management of the side effects of opioids in patients with cancer-related pain
- Discuss how to prevent potential risks and abuse of opioids in patients with cancer-related pain

Register to touchONCOLOGY for FREE
- Peer-reviewed journals and expert opinions
- Interactive CME and e-learning modules
- Video conference highlights