There is a large body of accumulated evidence that renal cell carcinoma (RCC) is an immunogenic tumour. Spontaneous and complete regressions of RCC metastases have been reported to occur, albeit in very rare cases.1,2 A few studies have reported profuse infiltration of RCC tumours by mononuclear cells,3,4 which may be immune-mediated or caused by non-specific inflammatory responses. However, in some patients tumour-specific T-cell lines and clones have been expanded from tumours.5–7
Therefore, as RCC is almost completely refractory to conventional treatments such as chemotherapy and radiation, early therapeutic strategies concentrated on immunotherapy.1,2,8 Before the approval of tyrosine kinase inhibitors (TKIs), cytokine therapy with interferon-α (IFN-α) and/or interleukin-2 (IL-2) was considered the standard treatment of metastatic RCC. However, durable and complete response rates were relatively rare, and clinical response rates reached no more than 20%.1,2,9–12 Other immunotherapeutic strategies, such as vaccination, resulted in promising immunological responses in patients with advanced RCC, but clinical efficacy remained low.13
A number of studies have shown that the cytokine profile observed both intratumorally and in the peripheral blood of patients with active disease is most consistent with a type 2 bias,5,14–16 and high levels of infiltrating T cells within RCC tumours were paradoxically associated with diminished cancer-specific survival.3,4 T-cell infiltrates within and surrounding tumour lesions were frequently composed of dysfunctional lymphocytes that had been rendered incapable of effectively mediating tumour regression and were more susceptible to cell death upon activation.16–19 On the molecular level, alterations in the expression and activity of intracellular signalling elements have been reported in RCC patients, including a decreased expression of the T-cell receptor (TCR) ζ chain (CD3ζ) and reduced tyrosine kinase activity,20–22 as well as defective activation of the transcription factor nuclear factor kappa B (NFκB).23–25 These data suggest that RCC frequently undermines spontaneous or immunotherapy-induced effector cell function.
The strategies RCC develops to evade antitumour immunity are frequent and quite diverse, suggesting the crucial importance of immune escape for tumour progression. Besides loss of tumour antigen expression, downregulation or even loss of molecules involved in antigen processing and/or presentation is a common immune escape mechanism in RCC leading to the failure of fully competent T cells to mount a productive immune response, a phenomenon also called T-cell ignorance26–28 (see Table 1). Moreover, tumours can express anti-apoptotic molecules, leading to resistance to killing by T cells or natural killer (NK) cells.29
Another strategy by which RCC escapes the immune system is the induction of tolerance by manipulating the function and proliferation of immune effector cells. This immunomodulation or tuning of the immune response can occur by a variety of mechanisms. In the following sections we will provide an overview of the most common mechanisms that mediate immune tolerance in RCC.
Active Suppression of Immune Effector Cells by Inhibitory Molecules Expressed by the Tumour
Co-stimulatory Molecules Inhibiting T-cell Responses
RCC cells constitutively express immunosuppressive co-stimulatory glycoproteins of the B7 family on their cell surface at a high frequency.30 The best analysed molecule is B7-H1 (programmed death ligand 1, PD-L1).30,31 The interaction of B7-H1 with its receptor PD1 on T cells is able to induce apoptosis in activated T cells or to impair cytokine production and cytotoxicity of activated antitumour T cells.31–33 In vivo monoclonal antibody-mediated blockade of B7-H1 has been shown to potentiate antitumour responses and to promote in vivo tumour regression in several murine cancer models.31,33–35 In RCC, aberrant B7-H1 expression was found not only in primary and metastatic tumour tissue but also on tumour-infiltrating mononuclear cells,36 and correlated with aggressive pathological features,36 increased disease progression, cancer-specific death and overall mortality.37 Therefore, B7-H1 is suggested as an independent predictor of prognosis.37,38 According to these results, PD1 expression on tumour-infiltrating lymphocytes (TILs) was associated with poor outcome in RCC patients.39 Furthermore, expression of B7-H4 (B7x, B7S1) or B7-H3 in RCC tissue was associated with adverse clinical and pathological features and was found to be an independent risk factor for RCC-associated death.40,41 Interestingly, in contrast to B7-H1, B7-H4 and B7-H3 are preferentially expressed in the tumour vascular endothelium. Moreover, elevated B7-H4 serum levels could be detected in RCC patients, correlating with advanced tumour stage.42 Although the receptor for B7-H4 has yet to be identified, in vitro studies suggested that B7-H4 may deliver an inhibitory signal to T cells, thereby abrogating CD4+ and CD8+ T-cell proliferation, cell-cycle progression and IL-2 production.2–4
Human Leukocyte Antigen-G
In contrast to classic human leukocyte antigen (HLA) class I antigens, HLA-G is characterised by a limited polymorphism and a physiological expression mainly restricted to the placenta, thymus, pancreatic islets, erythroid and endothelial cell precursors and immune-privileged tissues such as the eye and testes.43,44 There are at least seven alternatively spliced messenger RNA (mRNA) transcripts that encode for membrane-bound HLA-G (HLA-G1–4) and soluble HLA-G (HLA-G5–7).44 By binding inhibitory receptors such as immunoglobulinlike transcript 2 (ILT2), ILT4 and killer-cell immunoglobulin-like receptor two domains long cytoplasmic tail 4 (KIR2DL4), HLA-G prevents lysis by NK cells and T cells and promotes a T-helper cell type 2 (Th2) response.44,45 Moreover, HLA-G can transfer from cell to cell by trogocytosis, and cells that have acquired membrane-bound HLA-G1 by this mechanism act as regulatory cells – although for a limited amount of time. However, HLA-G may also have a long-term inhibitory function through HLA-G+ regulatory cells.44 In comparison with other tumour entities, the expression of HLA-G is relatively high in RCC. On the mRNA and protein level it was found in 45–60% of cases, independent of grading and stage of tumour, but its expression was subtype-specific, as it was mainly found in clear cell RCC but not in papillary RCC.46–49 HLA-G is induced by stress, hypoxia, IL-10, glucocorticoids, IFN, granulocyte–macrophage colony-stimulating factor (GM-CSF), gangliosides and the leukaemic inhibitory factor.43 Additionally, epigenetic mechanisms have been shown to play an important role in HLA-G regulation.50,51
Apoptosis-associated Ligands
Destruction of immune effector cells, by either directly inducing T-cell apoptosis or sensitising T-lymphocytes to activation-induced cell death, represents one potential mechanism to account for the observed defects in the clonal expansion and cytotoxic function of RCC-reactive T cells.17,52,53 Gene expression studies have shown an upregulation of several immune-regulatory molecules that are capable of inducing apoptosis;54 however, only a few genes, such as FasL and CD70, have been shown to be relevant for RCC immune escape.17,55 Overexpression of CD70 promotes lymphocyte apoptosis through its interaction with its CD27 receptor and the intracellular receptor-binding protein SIVA.55
Overexpression of FasL has been confirmed in many studies. Uzzo et al. were the first group to provide functional evidence17 for tumourinduced apoptosis of T cells via the expression of FasL. In concordance, increased Fas R expression was found in TILs of RCC.17,56 Moreover, FasL expression has been reported to be negatively correlated with prognosis in various cancers, and in some, but not all, studies of RCC.57–60
Active Suppression of Immune Effector Cells by Soluble Factors
Cytokines and Growth Factors
It has been shown that soluble products derived from RCC inhibit the proliferative capacity of T cells infiltrating human tumours, due to a downregulation of Janus kinase 3 (Jak 3), p56 (Lck), p59 (Fyn) and Zap 70.20,22,61 RCC is known to produce various cytokines, such as tumour necrosis factor alpha (TNF-α), transforming growth factor beta (TGF-β), IL-1β, IL-6 and IL-10, and growth factors, such as vascular endothelial growth factor (VEGF) or GM-CSF,15,18,62,63 that promote not only tumour growth but also immunosuppression by different mechanisms, such as induction of T- and NK-cell apoptosis, blocking of lymphocyte homing and activation and impairment of macrophage and dendritic cell (DC) function and maturation (see Figure 1 and Table 2).64–68 These immunosuppressive cytokines may also be secreted by the tumour microenvironment, composed of immune, stroma and vascular cells.14,15,69
NFκB has been identified as an upstream regulator responsible for the increased expression of various immunosuppressive factors including cytokines and growth factors.70,71 Moreover, cytokines and growth factors that impair host anti-tumour immune responses have been shown to activate signal transducer and activator of transcription (STAT) 3 in both tumour cells and immune cells, such as lymphocytes and antigen-presenting cells (APCs), blocking their normal function by inhibiting expression of Th-1 immunostimulatory molecules and promoting production of immunosuppressive factors.72–75
As STAT3 is a point of convergence for numerous tyrosine kinases, including VEGF receptor (VEGFR), platelet-derived growth factor receptor (PDGFR), endothelial growth factor receptor (EGFR) and Src, it is constitutively activated in diverse cancer cell types, including RCC,75,76 and prevents recruitment of lymphocytes to areas of tumour invasion by reducing expression of chemokines such as IP-10 and regulated upon activation, normal T cell expressed and presumably secreted (RANTES).74,75 Therefore, targeting these transcription factors may be an attractive therapeutic strategy, as it offers the possibility not only to block tumour cell survival and proliferation but also to restore the antitumour immune responses.73,75
Moreover, the mutation of the von Hippel–Lindau tumour suppressor gene (VHL) in RCC results in permanent activation of hypoxiainducible factor-1 alpha, causing upregulation of several growth factors such as PDGF, GM-SCF, VEGF and EGF, as well as TGF-α.77,78 VEGF not only plays a crucial role in angiogenesis, but also exerts immunosuppressive effects by inhibiting DC maturation in vivo.79,80 An inverse correlation between the density of DC and the expression of VEGF has been demonstrated within tumour tissue and the peripheral blood of cancer patients.11,12 The elevated level of circulating VEGF in cancer patients was also closely correlated with an increased number of immature myeloid cells in peripheral blood. Moreover, a recent study suggests a direct effect of VEGF on T cells with VEGF-induced chemotaxis of VEGFR1+ T-cells, increased IL-10 and decreased IFN-γ production.81 A correlation between elevated serum levels of VEGF and patient survival has been evidenced by some authors,82–84 but seemed not to be an independent prognostic factor for survival.85
Another key regulator molecule is cyclo-oxygenase-2 (COX-2), an enzyme involved in the formation of prostaglandin E2 (PGE2) from arachidonic acid. It is expressed in the majority of RCC tumours.86,87 Besides promoting tumour growth, angiogenesis and expression of anti-apoptotic molecules, COX-2 exerts immunosuppressive effects by activation of IL-6 and STAT3.88 Moreover, COX-2-derived prostaglandins have been shown to induce arginase I expression in myeloid-derived suppressor cells, which leads to depletion of arginine and thereby to T-cell dysfunction.89 Patients with maximal COX2 tumour staining might benefit form COX-2 inhibition.90
Gangliosides
Aberrant and elevated expression of gangliosides such as Gm2, Gm1 and Gd1a has been demonstrated on the surface of renal tumour cell lines and tissue.91–94 Gangliosides have been implicated in tumour progression by promoting angiogenesis and regulating cell migration and motility.94 Furthermore, gangliosides have also been found to inhibit multiple steps in the cellular immune response, including antigen processing and presentation, T-cell proliferation and – depending on ganglioside components – production of type 1 and type 2 cytokines. Moreover, RCC-secreted gangliosides were found to be involved in tumour-induced apoptosis of T cells: they could directly activate the intrinsic apoptotic pathway in a death-receptor-independent fashion by stimulating reactive oxygen species production, cytochrome C release and caspase-9 activation.95,96 With TNF-α they synergistically activate the receptor-dependent apoptotic pathway in lymphocytes.95 Moreover, gangliosides have been shown to suppress NFκB binding activity in T cells by impaired nuclear accumulation of RelA.97 Due to their important role in promoting T-cell dysfunction, gangliosides, including GM2, have been targeted by monoclonal antibodies (mAb) or vaccines to induce anti-GM2 antibodies.94
Induction of Immunosuppressive Cells
In addition to these active mechanisms described above, RCC also indirectly mediates immunosuppression by inducing cells with immunosuppressive properties, specifically regulatory T cells and dysfunctional APCs, which suppress the host antitumour responses both locally at the tumour site and systemically.
Regulatory T Cells
Natural and inducible T regulatory (Treg) cells are subsets of T lymphocytes able to suppress immune responses by direct interaction with other immune cells or through cytokines like IL-10 or TGF-β. They are characterised by expression of CD4, high-level expression of CD25, expression of glucocorticoid-induced TNF receptor (GITR), cytotoxic lymphocyte antigen-4 (CTLA-4) and the forkhead box P3 transcription factor FOXP3.98 As in a variety of other malignancies, increased frequencies of peritumoral or circulating Tregs have also been observed in RCC patients with either localised or advanced disease.99–102 They may be induced from CD4+ CD25– T cells or expanded from pre-existing Tregs by cytokines such as IL-10 and TGF-β that are produced by the tumour or tumour-associated myelomonocytic cells.98 Both increased peripheral circulating Tregs and peritumoral Tregs have been reported to be associated with worse prognosis in RCC.101–103 Moreover, a decrease in peripheral Treg cell frequencies may be correlated with clinical response to IL-2 immunotherapy;99,101 however, the effect of IL-2 on expansion and function of Tregs is controversially discussed.102,104,105
Several attempts have been undertaken to eliminate or to functionally inhibit Tregs to boost the efficacy of immunotherapy protocols.106 Danull et al. showed that elimination of Tregs by a diphtheria-toxinlabelled anti-IL-2-receptor antibody (IL-2 diphtheria toxin conjugate DAB389IL-2, denileukin diftitox, ONTAK) before vaccination with mRNA-transfected DC strongly enhanced induction of vaccinereactive T-cell responses without inducing toxicity on other cellular subsets with intermediate or low expression of CD25.100 By contrast, application of cyclophosphamide, known to downregulate Treg frequency and activity, could not enhance clinical or immunological efficacy of an allogenic DC vaccine.107
Tumour-associated Myelomonocytic Cells
Growing tumours inhibit the immune system by directly interfering with the differentiation, function and activation of APCs, such as DCs, monocytes or macrophages.108,109 Tumour-associated macrophages (TAMs), which represent the major inflammatory component of the stroma of many tumours, are characterised by the M2 phenotype and favour tumour progression not only by promoting tumour cell proliferation, angiogenesis, matrix remodelling and tumour migration, but also by suppression of adaptive immunity.108 Tumour-derived factors have been shown to induce the expression of TGF-β as well as IL-10, PGE2 and TNF-α,110 which downregulate the expression of cellsurface molecules involved in antigen presentation as well as their endocytic capacity.69
Moreover, by secretion of VEGF, GM-CSF, TGF-β, IL-10, IL-6 or PGE2, RCC arrests differentiation of APCs from its myeloid progenitors and triggers accumulation of myeloid-derived suppressor cells (MDSCs), a heterogeneous population of monocytes/macrophages, granulocytes and DCs at different stages of differentiation.109,111 They are negative for CD14, CD80, CD86 and major histocompatibility complex class II (MHCII) and express high levels of VEGFR164,111,112 and CD11b as a common marker, but may vary in their maturation markers, depending on the combination of factors produced by the tumour. As TAMs they promote angiogenesis and the development of Tregs, and their accumulation is associated with progressive tumour growth.108,109 They are suggested to engage an active cross-talk with TAMs to promote a generalised skewing of CD4 and CD8 T-cell immunity towards a type 2 response.
MDSCs isolated from RCC patients, but not from healthy donors, were capable of suppressing antigen-specific T-cell responses in vitro through the secretion of reactive oxygen species and nitric oxide upon interaction with cytotoxic T lymphocytes (CTL), which was reversible in vitro by exposing cells to the reactive oxygen species inhibitors. All-trans-retinoic acid (ATRA) was capable of abrogating MDSC-mediated immunosuppression and improving T-cell function by direct differentiation into APC precursors.111
Moreover, MDSCs have been shown to inhibit the T-cell response by depletion of arginine, mainly due to secretion of arginase I, which leads to distinct molecular changes in T-cells: a decrease in the expression of T-cell CD3ζ chain and impairment of T-cell signal transduction; and the inhibition of the cell cycle in the G0 phase.113 In RCC patients, increased numbers of MDSCs in the peripheral blood correlated with increased arginase activity in peripheral blood mononuclear cells (PBMCs), low L-arginine and high ornithine levels in plasma and a profound T-cell dysfunction and decrease in T-cell proliferation.112–114 In vitro depletion of MDSCs from the peripheral blood samples re-established T-cell proliferation and function.113,114 As high levels of VEGF have been shown to be associated with an increase in MDSCs in cancer patients,115,116 treatment with the anti- VEGF antibody bevacizumab could lead to a decrease in MDSC frequency, as shown in various murine tumour models.79,117 However, in contrast to the observation in mice, treatment of advanced RCC patients with bevacizumab did not reduce the accumulation of MDSC in peripheral blood.113
Therapeutic Perspectives in the Era of Targeted Therapies
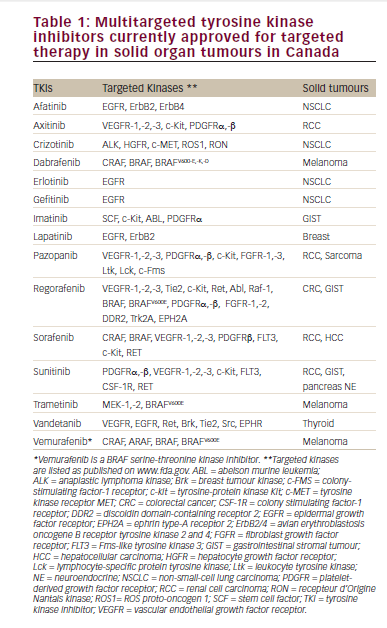
In recent years the development of new agents developed for targeting mTor or angiogenetic tyrosine kinases has substantially improved prognosis for patients with metastatic RCC.118 Nevertheless, immunotherapy is expected to experience a revival in the treatment of RCC: the growing knowledge concerning the molecular mechanisms that allow RCC to escape immune attack offers new therapeutic options, also in terms of the new targeted therapies. Furthermore, there are distinct immunological effects of targeted therapies, which have been only partially elucidated. Inhibitors of small molecules might enhance the immunogenicity of tumour cells by different mechanisms: making them more susceptible to killing by immune cells and by reversing the immune dysbalance induced by the tumour through direct action on immune cells or tumour cells (see Figure 2), or indirectly through reducing tumour burden.119–122 Therefore, sequencing or combining targeted therapies with immunotherapeutic strategies – including both mechanisms of immune activation and disruption of immunosuppressive pathways – may represent an attractive therapeutic concept. The efficacy of a standard immunotherapy combined with some anti-angiogenic agents123–125 or sorafenib126,127 has been investigated in clinical studies for RCC, and several studies combining small-molecule inhibitors with vaccination, cytokine therapy or immunoregulatory molecules are currently ongoing (www.clinicaltrials.gov). In contrast to the well-tolerated combinatorial approaches with IFN-α, caution is needed regarding sequential therapy with IL-2. A recent retrospective analysis of the safety and efficacy of high-dose IL-2 therapy after failure of prior VEGF targeted therapy in patients with metastatic RCC revealed a high incidence of severe cardiovascular complications after prior therapy with tyrosine kinase inhibitors.128 Although confirmation by larger studies is necessary, this analysis and the known cardiovascular side effects of these agents suggest that patients should be carefully selected for this sequential treatment regimen by extensive cardiovascular screening. However, as a variety of mechanisms are responsible for tumour-related immune tolerance and suppression, it is very likely that only combination therapy blocking different mechanisms may lead to success. One attractive strategy might be targeting NFκB and/or STAT3 as they are responsible for various immunosuppressive mechanisms and additionally are important for tumour cell survival and proliferation. ■