Despite the addition of tumour-site-specific planning margins to target volumes defined on conventional CT scans, inadequate coverage of lung tumours and/or excessive irradiation of normal tissues are commonly observed.2–4 As such, individualised or ‘patient-specific’ planning margins are recommended instead of standard or ‘population-based’ margins.5,6
Different approaches have been used to determine individualised margins, but 4-D CT (4DCT) scans, or respiration-correlated CT scans, have been the focus of most interest. Since the first reports on the use of 4DCT in radiotherapy planning in 2003,7,8 aspects of the technique have rapidly evolved and many major manufacturers specifically offer 4DCT imaging as an option in imaging for radiotherapy planning.
During 4DCT acquisition, images are acquired in all phases of the respiratory cycle while simultaneously recording respiration, followed by a retrospective sorting process that correlates CT images with the phase of respiration.
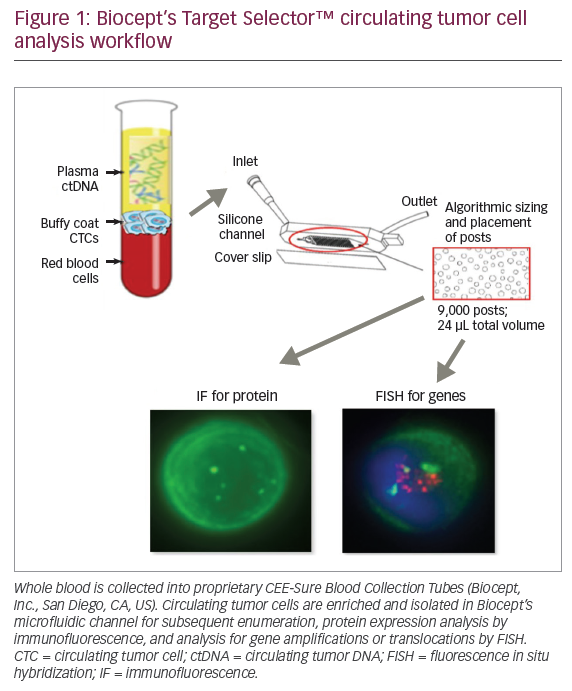
Up to 10 respiration-correlated 3-D data sets are typically derived from a single 4-D data set. Each of the resulting respiration-correlated 3-D data sets represents the patient’s anatomy during a single respiratory phase. 4DCT images can be viewed on a 4-D workstation in the form of movie loops in any selected plane (see Figure 1), or can be visualised using a colour intensity projection (CIP), which incorporates the motion information of selected component 4DCT data sets for each slice into a single composite colour image.9
Current Status in Implementing 4DCT
4DCT studies provide an insight to the possible intra-fractional motion of intrathoracic and upper abdominal organs and tumours, and some key aspects are highlighted below. Use of 4 DCT for Defining Reproducible Target Volumes in Lung Cancer
A reproducible respiratory pattern is required in order to acquire optimal 4DCT data sets, as a respiratory pattern that is not sufficiently reproducible results in missing images at a specific respiratory phase for some table indices.10
However, a majority of patients with lung cancer have impaired pulmonary function. If respiratory coaching is used to optimise image acquisition, and to avoid ‘gaps’ in resorted 4DCT volumes, it implies that such coaching should also be used during treatment delivery. The latter will result in a more labour-intensive procedure.
It is reassuring that two recent studies in patients undergoing 4DCT without respiratory coaching found that reproducible target volumes can be derived for non-gated radiotherapy. In the first study, adequacy of coverage of the target volume was assessed in 26 patients with peripheral lung cancer who underwent two successive 4DCT scans at a single session.11
A dosimetric analysis revealed that the planning target volume (PTV) derived from a single uncoached 4DCT achieved similar dosimetric coverage to that achieved using two consecutive 4DCT scans. Analysis of repeat 4DCT target volumes in 59 consecutive patients who underwent radiotherapy planning for stereotactic radiotherapy found that treatment based upon a PTV derived from only the initial 4DCT would not have led to under dosage to the tumour in nearly all patients.12
Implementing Respiration-gated Radiotherapy (RGRT) for Lung Cancer
By limiting treatment delivery to a pre-defined phase of respiration, RGRT permits the irradiation of smaller target volumes. However, an evaluation of 4DCT scans is required in order to individually assess the potential benefits of this approach.5,13
For patients with stage I non-small cell lung cancer (NSCLC), the potential benefits of RGRT were shown to correlate with the extent of tumour mobility, which was seen when the 3-D mobility vector was ?1cm.6
Images can be viewed in any plane and motion evaluated using movie loops and measurement tools.
However, the same analysis revealed that if a threshold reduction in PTV of at least 50% is required, only 15% of patients with stage I NSCLC would benefit from RGRT. In view of the limited toxicity observed with stereotactic radiotherapy for stage I NSCLC,14 the benefits of RGRT for this indication are unclear.
A similar analysis in stage III NSCLC patients revealed that the smaller gated treatment volumes at end-expiration reduced lung toxicity parameters such as the percentage of lung volume that received a dose of 20Gy or more (V20) and mean lung dose by, respectively, 7% and 4.9%.13 4DCT data also allowed for the average residual 3-D tumour mobility within the gating window of 4.0 ± 3.5 mm to be accurately established.
Characterising Motion of Normal Organs for ‘Conformal Avoidance’
An analysis of abdominal 4DCT scans from 54 patients found predominantly cranio-caudal renal motion, with a mean of 9.8mm for the left kidney and 9.0mm for the right.15 Large inter-patient variations were observed, ranging from 2.5mm to 30mm (left) and from 2.5mm to 20mm (right), and mobility of one kidney did not predict for mobility of the contralateral organ.
A comparable study revealed mobility of the distal oesophagus, the magnitude of which could be significant during high-dose stereotactic radiotherapy to paraspinal and paramediastinal tumours.16 This analysis recommended location-specific oesophageal mobility margins of 5mm proximally for both mediolateral and dorso-ventral directions, 7mm and 6mm, respectively, in the mid-oesophagus, and 9mm and 8mm, respectively, in the distal oesophagus.
Evaluation Image-guided Radiotherapy Approaches for Abdominal Tumours
As both the pancreas and adjacent organs exhibit respiration-induced motion, a 4DCT planning study was performed to examine a possible reduction in renal doses by using RGRT and intensity-modulated radiotherapy (IMRT).17 IMRT alone was shown to achieve a significant reduction in renal doses, with a reduction in left kidney of 42.2% and 55.4% for the right kidney. Rather surprisingly, RGRT did not significantly reduce renal doses, either with or without IMRT.
A similar analysis of standard fields recommended for gastric radiotherapy in a previous study revealed that standard fields did fully cover the PTV in any of five patients.18 Conventional planning using 4DCT information to optimise target coverage would have resulted in a mean dose of 19.9Gy to the left renal volume and 29.0Gy to the right renal volume.Again, RGRT would have resulted in clinically insignificant dose reductions in comparison with non-gated radiotherapy, a finding accounted for by parallel movements of the stomach and kidneys during quiet respiration.
Nevertheless, the gated PTVs were up to 11% smaller, which could decrease the volume of irradiated bowel.
These studies have highlighted the need to evaluate new techniques for combined modality treatments using 4-D imaging. A failure to do so could risk inferior tumour control when implementing ‘modern’ techniques.19
Impediments to the Clinical Use of 4 DCT
Hardware issues of 4DCT acquisition have largely been resolved. However, limitations in software tools to analyse the large volume of generated data in each patient, as well as the unavailability of 4-D radio-therapy planning software, remains an impediment for clinical use of 4DCT data. A few key points are highlighted below.
Planning Tools for Evaluating 4DCT Scans
Most current radiotherapy planning systems still do not allow for the import of all 4-D information. Despite this, efficient clinical use of 4DCT data sets in lung cancer has been made possible using the post-processing tool of maximum-intensity projection20 and colour intensity projection.9 Such approaches allow for a rapid evaluation of motion for RGRT and permit contours to be generated in a matter of minutes.
4-D Radiotherapy Planning Systems
4DRT has been defined as the “the explicit inclusion of the temporal changes in anatomy during the imaging, planning and delivery of radiotherapy”.1 No commercial 4-D planning systems are currently available; tools such as deformation registration are essential in order to reduce the workload and enable a true estimate of the radiation dose to sites affected by motion to be determined.
Lack of Tools for Verifying 4-D Radiotherapy
Changes in tumour position or size can arise during treatment, and volumetric imaging at the treatment unit is desirable, particularly when interventions for motion management such as RGRT have been implemented. Even for tumours that are visible on fluoroscopy, a comparison of simulated conventional fluoroscopy using the same data set used for 4DCT revealed that clinicians consistently overestimated the mobility of tumours when using fluoroscopy.21 This suggests that fluoroscopy is unsuitable for verifying target volumes during high-dose stereotactic radiotherapy. Volumetric cone-beam CT (CB-CT) scans that are mounted on the linear accelerator have entered clinical use.22 The slow image acquisition using CB-CT results in a ‘slow’ CT image that is blurred, and the development of gated CB-CT acquisition is awaited in order to allow for evaluation of RGRT.
Conclusion
The clinical use of 4DCT data is of crucial importance for optimal IGRT for tumours in the thorax and upper abdomen. However, major impediments to the clinical implementation of 4-D radiotherapy are the lack of 4-D planning software, and a lack of software tools that allow for online verification of IGRT.