Unfortunately, only a small proportion – between 10 and 15% – of patients with liver metastases only are primary candidates for potentially curative liver resection, since surgery is limited to those with a good performance status, and those who fall within ‘limited disease criteria’ (generally four or fewer tumors in one lobe of <4cm each, not involving major vascular structures). Of those who do have a complete surgical resection undertaken with curative intent, the five-year survival rate is 30–40%, with at least two-thirds of patients developing recurrent liver metastases within two years after surgery.4 The majority of patients with liver metastases are initially not candidates for liver resection and are managed with systemic chemotherapy; there have been major palliative advances in this field over the last 10 years. Until the mid-1990s the only available drug—which had limited activity in metastatic colorectal cancer—was fluorouracil (5FU). The last decade has seen a rapid evolution of systemic chemotherapies for metastatic colorectal cancer with the development of new cytotoxic agents such as oxaliplatin and irinotecan; oral analogs (Capecitabine; Xeloda® and UFT-tegafur); and targeted biologicals such as bevacizumab (a monoclonal antibody against vascular endothelial growth factor) and cetuximab and panitumumab (monoclonal antibodies against the epidermal growth factor receptor type-1).
Combined with 5FU plus leucovorin (LV), irinotecan-based (FOLFIRI) and oxaliplatin-based (FOLFOX) regimens have evolved as standard first- and second-line treatments for metastatic colorectal cancer (see Table 1). More recently, phase II/III clinical trials have shown that the addition of bevacizumab increases the activity of 5FU/LV, irinotecan combinations,5 and oxaliplatin-based (FOLFOX) regimens.6 Recent trials (XELOXA/NO16966 and CRYSTAL) have suggested that biologicals may not provide the level of added benefit that was originally hoped for.7
These important new advances in biologic and cytotoxic agents have resulted in a significant prolonging of median survival time from approximately six months with 5FU-containing chemotherapy regimens8 to an excess of 20 months in some studies.5,9,10 Yet, despite these valuable gains, metastatic colorectal cancer is almost always fatal, with up to 90% of patients dying of liver failure caused by local effects of hepatic tumors. In high-risk patients with non-resectable and chemo-refractive liver tumors, therapies should be considered palliative, with the primary aim of treatment being to achieve a maximum reduction in tumor cell burden and improvements in progressionfree survival and quality of life, as well as improving overall survival. External-beam radiation therapy (EBRT) is a cornerstone of curative and palliative therapy in nearly all malignancies, but has not been applied with much success to hepatic disease due to the low tolerance of the organ to radiation compared with tumor. Significant technological advances in radiation treatment planning and delivery—which may benefit an increasing number of patients with liver metastases—have led to improved tumordirected radiotherapy approaches, such as:
• 3-D radiotherapy;
• intensity-modulated radiotherapy; and
• stereotactic radiotherapy.
However, the key limitation of this treatment is the tolerance of normal liver parenchyma to radiation. The maximum acceptable dose to the whole liver is 35Gy, which is far below the required dose to destroy adenocarcinoma metastases, estimated at 70Gy or above (for monotherapy) or at 50Gy or above when concurrent chemotherapy is given. An alternative approach is the implantation of radiation sources into the tumor (brachytherapy).
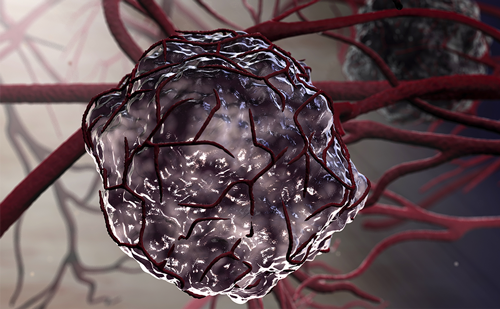
One form of brachytherapy is radioembolization, or selective internal radiation therapy (SIRT), which has been successfully utilized for the treatment of liver metastases and primary liver tumors. This procedure delivers radiation particles intravascularly, and takes advantage of the differential blood supply to tumors and normal parenchyma in order to ensure tumor-directed therapy. Eighty percent of the blood supply to the liver is via the portal vein, whereas almost all of the blood supply to the tumors is via the hepatic artery. By using the hepatic artery to inject embolic particles, multiple sites of disease within the liver can be selectively irradiated in a single procedure. The radiation is delivered by SIR-Spheres® (Sirtex Medical, Australia), which are biocompatible microspheres containing the pure beta-emitter radionuclide yttrium-90, which decays to stable zirconium-90 with an average half-life of 2.67 days (64.2 hours). The microspheres, with a mean diameter of 32μm, lodge within malignant microvasculature where they deliver high localized doses of ionizing radiation (100–3,000Gy) to tumors and the neovascular supply of the tumor while delivering safe levels to the normal tissue (mean penetration of radiation into tissues is 2.4mm).11 Notably, the size of the microspheres means that they cannot pass into the capillary bed.
This loco-regional approach has been used for many years to deliver chemoembolization to hepatic malignancies, but such treatments have not provided any evidence of survival benefits in metastatic colorectal cancer (mCRC). In contrast, there is a growing body of evidence demonstrating the efficacy of radioembolization using SIR-Spheres in improving the treatmentrelated response, time to disease progression, and survival either in combination with systemic chemotherapy compared with chemotherapy alone12,13 or as a monotherapy.14 The evidence shows that responders appreciate a longer survival with little, if any, detrimental impact of treatment on quality of life.
The Clinical Evidence for Radioembolization with SIR-Spheres In parallel with the evolution of systemic chemotherapy, a series of randomized, controlled trials has been conducted combining SIR-Spheres initially with hepatic artery chemotherapy then systemic chemotherapy, as well as in single-arm dose-escalation studies. A summary of the results from these trials is outlined in Table 2.
In one of the early trials, SIR-Spheres were evaluated as a first-line treatment in patients with non-resectable liver-only colon cancer metastases.12 Combined with hepatic artery chemotherapy with floxuridine, patients treated with SIR-Spheres showed a significant reduction in tumor volume (p=0.03) and increase in time to progression (15.9 versus 9.7 months; p=0.001) compared with those receiving hepatic artery chemotherapy alone (see Table 2). The one-, two, three-, and five-year survival for patients receiving SIR-Spheres was 72%, 39%, 17%, and 3.5%, respectively, compared with 68%, 29%, 6.5%, and 0%, respectively, for hepatic artery chemoembolization alone. However, the study was halted prematurely and not powered adequately to show survival advantage.12 Nevertheless, the study was important in demonstrating the efficacy and tolerability of SIR-Spheres, and cox regression analysis suggested a benefit for patients treated with SIR-Spheres surviving beyond 15 months (p=0.06). Moreover, the addition of SIR-Spheres microspheres to hepatic artery chemotherapy was found to have no major adverse impact on quality of life, with both treatment groups demonstrating some improvement in quality of life. It is apparent from clinical reports that one of the principle determinants of survival after radioembolization is the presence or subsequent development of clinically relevant extrahepatic disease. The experience of investigators indicates that median survival times are reduced in patients who either have significant extrahepatic disease prior to treatment or who develop such disease within six months of radioembolization compared with those who did not (8.3 versus 12.6 months; p<0.001).14 These results suggest that localized treatment with SIR-Spheres should be combined with systemic chemotherapy in order to achieve the maximum survival benefit.
Subsequently, a randomized, controlled trial combining SIR-Spheres with 5FU/LV systemic chemotherapy was conducted in 21 patients with previously untreated advanced colorectal liver metastases, with or without extrahepatic metastases.13 The study found that the addition of a single administration of SIR-Spheres to a regimen of 5FU/LV chemotherapy significantly increased both time to disease progression (18.6 versus 3.6 months; p<0.0005) and median survival by more than 16 months (29.4 versus 12.8 months; p=0.02) compared with system chemotherapy alone (see Figure 1).12
SIR-Spheres for the first- and second-line treatment or salvage therapy of metastatic colorectal cancer. *p = 0.06 ; **p ≤0.05; ***p ≤0.001; ****p = 0.0001 SIR-Spheres versus active control. a Patients with liver-only disease; HAC = hepatic artery infusion; 5FU = fluorouracil; LV = leucovorin.
Adoption of radioembolization in most clinics started conservatively as salvage therapy. A retrospective analysis was conducted in 208 patients with unresectable liver-predominant metastases from colorectal cancer that were refractory to oxaliplatin-based (FOLFOX) regimens, irinotecan-based (FOLFIRI) regimens, or third-line chemotherapy and were not eligible for liver-directed therapy (including radiofrequency ablation (RFA), transarterial chemo-embolization (TACE), resection, intensity-modulated radiotherapy (IMRT), and stereotactic radiotherapy). After a single dose of SIR-Spheres, patients were followed up for a median of 13 months (range 1–42 months). In total, positron emission tomography (PET) scans showed response in 176 of 208 patients (85%). The study showed a significant survival benefit in the majority of patients responding to SIR-Spheres (see Figure 2). Researchers found that if patients did not experience a measurable response (carcinoembryonic antigen (CEA), PET, or computed tomography (CT) scan) by six weeks after treatment, their survival was short (median 4.5 months) compared with responders, who achieved an appreciably longer survival (median 10.5 months; p=0.0001).13
Although the early randomized, controlled trials involved regimens that are now considered outdated and were inadequately sized to show a convincing survival benefit, the potential was sufficient to encourage further assessment of the safety and tolerability and dosing of SIR-Spheres combined with modern agents. Phase I studies of SIR-Spheres + FOLFOX and SIR-Spheres + irinotecan have shown impressive response rates and progression-free survival.16–19 Sharma and colleagues treated newly diagnosed patients with FOLFOX4 and one application of SIR-Spheres during the first week of chemotherapy. A partial response by CT scan using Response Evaluation Criteria in Solid Tumors (RECIST) criteria was confirmed in 18 of 20 patients (90%), with stable disease in the remaining patients and no progressive disease.16 After 12 cycles of chemotherapy, three patients were down-staged and two of these patients were surgically resected. Time to progression was 9.3 months (range 3.9–30.7 months) in the whole patient group and 14.2 months (range 6.4–24.9 months) in a subset of seven patients with no extrahepatic metastases at study entry.16 Although the patient numbers are small, these results compare favorably with trial data for FOLFOX4 chemotherapy alone in this patient group.20,21 In fact, the clinical outcomes of radioembolization in combination with first-line chemotherapy regimens compare favorably with those from current chemotherapy regimens with or without the addition of new biological agents (see Figures 4 and 5). Van Hazel and Goldstein also tested the efficacy and safety of SIR-Spheres plus second-line chemotherapy with irinotecan.17–19 Over a third of the 25 patients included in the study had failed up to three previous lines of chemotherapy and 60% of patients had failed prior oxaliplatin treatment. The study showed that a single dose of SIR-Spheres in combination with irinotecan was associated with an acceptable toxicity profile.17 An overall response was achieved in 48% of patients and disease control in 87%. Median time to progressive disease was 9.2 months in the liver and 6.0 months at any site including the liver. Median overall survival was 12.2 months (range 2.8–42.3 months).19 Again, these results compare favorably with studies on irinotecan alone in second-line therapy.22–24
Radioembolization in the Continuum of Care
In summary, the evidence indicates a clear synergy between radioembolization with SIR-Spheres and systemic chemotherapy, extending survival and progression-free survival and improving response rates as a firstand second-line therapy, or as a salvage monotherapy in patients with chemorefractory disease. Furthermore, radioembolization with SIR-Spheres appears to be well tolerated and maintains quality of life in patients with unresectable tumors.12 The relative ease of administration means that treatment can be delivered on an outpatient basis, or involving one night’s hospitalization in the majority of patients.
SIR-Spheres used in conjunction with modern systemic chemotherapies are appropriate both to avoid extrahepatic progression and to prolong the local effects of radioembolization. While the evidence supports the potential of radioembolization using SIR-Spheres to provide substantial clinical benefit for patients with liver-predominant colorectal metastases at various points in the continuum of care—from first-line setting through to salvage therapy—the benefits in reducing tumor burden appear to be greatest early on when the liver vasculature is also less compromised. Moreover, because the liver is the major initial site of metastases,25 improved early responses at this site may improve overall survival. With the availability of more effective systemic chemotherapies, strategies are now being developed to resect what in the near past was regarded as ‘unresectable’ disease. The evidence indicates that this may well be a realistic goal in up to 25% of patients with metastases confined to the liver who are treated with chemotherapy alone. For these patients, the curative potential of treatment compared with classical palliative end-points of response or progression-free survival becomes a real possibility. In a retrospective analysis of published studies, Folprecht and colleagues26 found a significant correlation between response rates and the resection rate in studies with patients with isolated liver metastases (p=0.002). It is increasingly likely that radioembolization will be adopted to augment the regional response of systemic chemotherapies in the liver and increase the number of patients who are candidates for colorectal liver metastases resection. Application of an innovative multidisciplinary approach that integrates advanced surgical techniques with new drug treatments and therapeutic approaches (such as radioembolization and local ablative therapy) will allow the benefits of curative hepatic resection to be extended to a broader group of patients. However, the optimal management of patients with colorectal liver metastases can be provided only by close co-operation with various specialists (comprising a liver surgeon, oncologist, hepatologist, interventional radiologist, nuclear medicine physician, and histopathologist) who have an in-depth understanding of the latest diagnostic and therapeutic options.
Radioembolization ‘Comes of Age’
An international clinical program is now ongoing evaluating radioembolization using SIR-Spheres in phase II/III studies in combination with the newest and most effective chemotherapy agents for colorectal cancer (such as FOLFOX) in the SIRFLOX study and biologicals such as bevacizumab (concurrently administered with either FOLFOX6 or FOLFIRI) in the FAST study, and cetuximab combined with irinotecan in another phase II/III study. Finally, there is increasing evidence that the role of radioembolization is not limited to colorectal liver metastases, since significant clinical benefits have also been reported in liver metastases from breast cancer,27 neuroendocrine tumors,28–30 and other cancers,31–34 as well as in primary liver cancers such as hepatocellular carcinoma35–39 and nodular cholangiocarcinoma.40 Research into these other indications is also ongoing.