Resection of all or part of the bony pelvis, commonly referred to as internal hemipelvectomy, is a common treatment for various localized primary tumors, and is also rarely used for metastatic lesions in this region.1,2 The generally accepted oncologic principle of obtaining a wide margin is followed to ensure adequate tumor resection and to optimize local control. While the principles of resection are not debated, musculoskeletal oncologists differ in opinion regarding the most durable and functional method of reconstruction. Primary musculoskeletal tumors involving the pelvis are rare, so there is a paucity of literature from which to draw definitive conclusions regarding the most efficacious reconstruction method in these complex cases. Furthermore, reported functional data typically relies on largely subjective criteria, such as the Musculoskeletal Tumor Society functional score.
The purpose of this article is to review the indications for internal hemipelvectomy and to examine the risks and benefits of the available reconstruction methods.
Indications
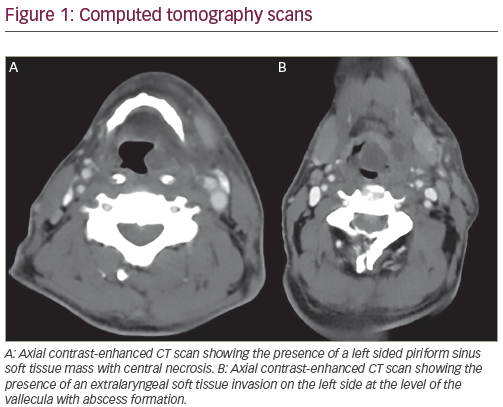
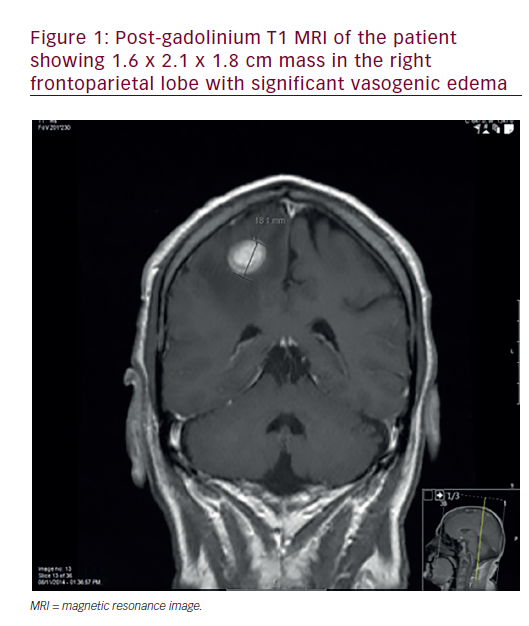
Patient evaluation begins with a focused history and physical examination. This is typically followed by radiographic evaluation of the tumor along with appropriate staging studies. Plain radiographs are often deceptively normal in cases of pelvic malignancy (see Figure 1). Computed tomography (CT) scans and magnetic resonance imaging (MRI) are used liberally to define the characteristics and local extent of the tumor. Biopsy is typically performed under CT or ultrasound guidance by a qualified radiologist and should be carried out with the guidance of the orthopaedic oncologist who will perform the definitive resection.3
Tumor resection should proceed according to the generally accepted oncologic principle of obtaining a wide margin of normal tissue. This may not be possible if the tumor encases the pelvic viscera or vital neurovascular structures or extends widely into the sacrum. Relative contraindications to limb-sparing surgery include the presence of metastatic lesions distant to the primary tumor site, extensive involvement of the pelvic viscera and/or neurovascular structures, a non-functional limb, and history of a failed prior resection (e.g. local recurrence). Limb-sparing tumor resections of the pelvic girdle were classified by Enneking4 according to location. Type I resection includes the ilium from the sacroiliac joint (occasionally requiring partial sacral resection) posteriorly to the hip joint anteriorly. Type II resection includes the hip joint and peri-acetabular region. Type III resection includes the pubis. Total internal hemipelvectomy has been referred to as a type IV resection, as the entire hemipelvis is resected.5A utilitarian incision is typically employed to gain access to the hemipelvis and its surrounding soft tissues. The incision follows the course of the iliac crest laterally and posteriorly and splits into two separate limbs at the level of the anterior-superior iliac spine. Medially, the incision follows the course of the inguinal ligament. The distal limb of the incision follows the anterior border of the gluteus medius muscule. Occasionally there is a perineal extension of the ilio-inguinal limb for medially-based tumors that involve the adductor musculature.
Reconstructive Options
Instability of the pelvis and the leg-length discrepancy that results following resection of the innominate bone is thought to lead to poor ambulation and inferior patient acceptance.6–11 As a result, most authors currently advocate replacement of the resected bone using a prosthetic device or allograft, or by using other means to reconstruct the pelvic ring.6,12–17 Options for reconstruction include allograft,allograft–prosthetic composite, and endoprosthetic reconstruction.
High complication rates have been reported for the various types of reconstruction following internal hemipelvectomy.12,18,19 Internal hemipelvectomy with endoprosthetic reconstruction carries the unique risk of prosthetic failure. In their 2007 review of 24 consecutive patients who underwent internal hemipelvectomy with endoprosthetic reconstruction, Tunn et al. reported a 41.7 % incidence in deep infection, a 33.3 % incidence of nerve injury, and a 16.7 % incidence of implant loosening. The authors recommended that an alternative method of reconstruction be sought for these complex patients.20 Similarly, Dai described the results of 10 patients who underwent reconstruction of pelvic resections using computer-aided custom endoprostheses.8 Two patients (20 %) experienced early dislocation and three (30 %) faced problems with wound healing.
Endoprosthetic reconstruction is often precluded by severe pelvic bone loss following wide resection. Conventional acetabular implants that primarily rely on screw fixation and press-fit techniques will not typically achieve adequate initial stability to allow for reliable bone ingrowth. A new device based on Wolff’s law (Compress, Biomet, Inc. Warsaw IN) has been employed in the setting of severe long-bone defects with promising results.21,22 If adequate anterior column exists following tumor resection, a custom acetabular component that couples to a Compress device may provide adequate initial stability (see Figure 2). Biologic fixation and bone ingrowth is typically achieved about eight to 12 weeks after implantation.
The complications associated with allograft reconstruction of the pelvic ring are similarly significant.7,13,14 Unique to this type of reconstruction is the possibility of poor graft incorporation, fracture, and disease transmission. In their 2007 review of 24 consecutive pelvic allograft reconstructions following resection of a bone malignancy, Delloye et al. reported a non-union in three of 16 patients with radiographic follow-up. Additionally, 11 out of 24 patients (46 %) underwent repeat surgery. Nine of these cases were directly related to failure of the allograft reconstruction.23 Similarly, Beadel et al. reported a 47.4 % incidence of infection in patients who underwent allograft reconstruction for pelvic malignancy, seven of whom required removal of the allograft or external hemipelvectomy.24 Failure of allograft incorporation typically leads to hardware failure and construct loosening over time. Some authors advocate the used of vascularized tissue to improve the likelihood of achieving biologic fixation.An alternative method of limb salvage following resection of the hemipelvis is resection arthroplasty (see Figure 3). The clinical and functional results following internal hemipelvectomy without reconstruction have been reported previously.25–28 Resection arthroplasty is a well-established procedure for conditions affecting the acromioclavicular, femoroacetabular, proximal radiocarpal, scapulothoracic, and metatarsophalangeal joints, among others.29–33 Despite its widespread use elsewhere, however, most authors criticize the use of resection arthroplasty for conditions involving the pelvic girdle, citing poor function and unacceptable levels of pain.
Following resection arthroplasty, all patients typically ambulate with a Trendelenberg gait and most require the use of a shoe-lift. It is the authors’ experience that stability of the extremity—and thus ambulation—is improved by utilizing a shoe-lift that is approximately 50 % of the total leg-length discrepancy (e.g. a 2.5-inch lift for a 5-inch leg-length discrepancy). This allows the patient to ambulate with the foot in slight equinus. If the lift equals the total leg-length discrepancy, the plantigrade foot rests on an unstable platform, which is less cosmetic and functional than walking on the ball of the foot.
The prolonged rehabilitation course following this procedure should be discussed with the patient pre-operatively. The authors have found that patients with follow-up of more than three years after resection arthroplasty tend to have better function compared with those in the early post-operative period. By three years most patients are able to achieve pain-free, independent ambulation without the use of supports. Critical to the success of this procedure is the meticulous reconstruction of the soft tissues surrounding the hemipelvis. Following resection, the remaining abductors and gluteal muscles are sutured in multiple layers to the abdominal wall musculature. If the anterior resection is through the symphysis, it is frequently necessary to place a prosthetic mesh to facilitate repair of the adductor musculature to the abdominal wall. This prevents herniation of the pelvic contents anteriorly.
Functional outcomes following resection arthroplasty are at least as acceptable, if not better, than those reported for either allograft or endoprosthetic reconstruction. With resection arthroplasty, the spectrum of complications unique to the latter two modes of reconstruction do not occur. Additionally, the cost of internal hemipelvectomy without reconstruction was found to be lower than either reconstruction with an endoprosthesis or classical external hemipelvectomy.34
Conclusion
Internal hemipelvectomy has been firmly established as a reliable method of treatment for the vast majority of patients with primary localized tumors involving the hemipelvis. Tumor resection typically results in severe bone loss and reconstruction can be challenging. Acceptable results have been reported for endoprosthetic, allograft and allograft–prosthetic composite techniques, although all carry the risk of implant/construct failure.
Resection arthroplasty is an alternative to reconstruction and may limit the need for additional procedures, although patients should be counseled regarding the typically lengthy rehabilitation process. Prospective studies based on well-defined objective criteria of patient function, perhaps through gait analysis, are needed to more accurately compare the various reconstructive methods following internal hemipelvectomy.