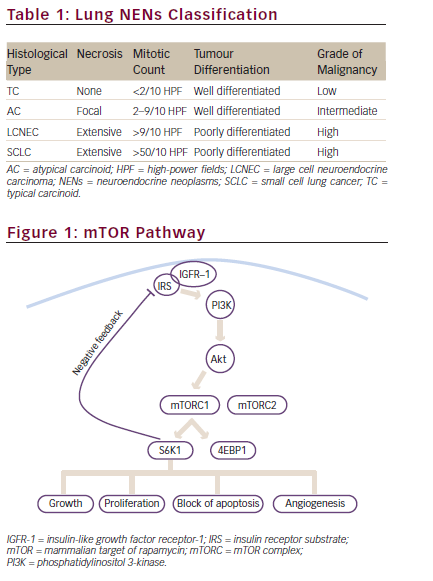
Octreotide and Lanreotide
Octreotide and lanreotide are currently the most widely used somatostatin analogs to date. They control symptoms by inhibiting the synthesis and secretion of peptides and amines associated with functional sst 2- positive tumors. Following sst 2 binding, inhibition of G-protein-associated signal transduction pathways block secretory vesicle exocytosis and, thus, the release of the target peptide or amine. Pancreatic and digestive tract endocrine tumors can express multiple sst subtypes, but sst 2 predominance is found in >80% of these tumors. US Food and Drug Administration (FDA)-approved indications for octreotide are for the control of secretory diarrhea from carcinoid and vasoactive intestinal peptide (VIP)-omas and the control of growth hormone secretion in patients with acromegaly.Although a wide variety of other out-of-indication uses for this drug have been proposed, octreotide is currently the only somatostatin analog available in the US for the treatment of neuroendocrine tumors.
Some investigators believe that octreotide has both a suppressive effect on the growth of tumor cells in vitro and an antiproliferative or tumorostatic effect clinically. Octreotide growth inhibitory action in tumor cells may be independent of its neuroendocrine functions. In a variety of in vitro studies, octreotide has been shown to inhibit the growth of tumor cells and a variety of other sst 2-expressing cell types such as retinal pigment epithelial cells and smooth muscle cells. Interestingly, in these in vitro studies, the antiproliferative effect of octreotide is biphasic. At concentrations of 10–12 mol/l or less, octreotide has little or no effect on cell growth. Increasing drug concentrations up to levels of 10-9 to 10- 8 mol/l is associated with concentration-dependent inhibition of cell growth, with maximum inhibition seen in the range of 10-9 to 10-8 mol/l. Further increases in drug concentration (>10-8 mol/l) are not associated with additional increases in cell growth inhibition. Instead, higher drug concentrations are associated with a dosedependent loss of cell growth inhibition compared with the 10-9 to 10-8 mol/l concentrations of octreotide.Thus, the optimum antiproliferative effects of octreotide occur in a relatively narrow concentration range, and under- or overdosing of this drug might lead to higher rates of tumor cell proliferation.
This table lists the binding affinities (IC50 values in nM) of somatostatin-14 and three of its analogs for various somatostatin receptors. HSST = human somatostatin receptor.
Octreotide has also been shown to have a direct effect on the growth of angiogenic vessels, based on the unique expression of sst 2 on proliferating, but not normal, blood vessels. Thus, octreotide therapy—when administered at optimal doses—should have an antiproliferative effect on the tumor (at the cell level), the angiogenic blood vessels, or both. Gulec et al. recently reported on the use of nude mouse-human tumor xenografts (which contained either sst 2-positive or sst 2-negative tumor cells) in a unique tumor fragment-based in vitro angiogenesis assay. These authors showed that sst 2-preferring radiolabeled somatostatin analogs could destroy sst 2-expressing tumor cells and destroy their sst 2-expressing angiogenic response. In contrast, sst 2 nonexpressing tumor fragments were not destroyed by these sst 2-preferring radiolabeled somatostatin analogs, but their angiogenic vessels (sst 2 positive) were destroyed.These studies show that the sst 2 receptor is uniquely expressed on angiogenic vessel endothelium. In contrast, endothelial cells in normal human blood vessels do not express sst 2 receptors. This unique expression of sst 2 in angiogenic blood vessels may make this receptor an excellent target for somatostatin-based therapies.
This figure illustrates the inverse relationship between patient weight and mean octreotide plasma level (i.e. when weight is increased, plasma level is decreased) when patients are treated with 30mg of Sandostatin® LAR.
Use of Somatostatin Analogs
While the antiproliferative actions of somatostatin analogs remain disputed, the more accepted use of these reagents is for control of symptoms due to amine-induced syndromes. Octreotide reduces the incidence of amineinduced diarrhea by 50% and reduces the incidence of amine-induced flushing by 68%. Additional uses include the peri-operative administration of octreotide in order to prevent ‘carcinoid crisis’. Other more controversial indications include: use after debulking procedures such as surgical, radiofrequency ablation or embolization to delay tumor regrowth; adjuvant treatment in patients who have no evidence of residual disease; and asymptomatic patients at the time of diagnosis of metastatic disease.
Octreotide is available in two forms. It is marketed as an immediate release form (aqueous) that can be clinically administered by multiple subcutaneous (SC) injections, by continuous SC infusion, or by intravenous (IV) routes. It is also available in a long-acting repeatable (LAR) formulation (Sandostatin® LAR). Clinically, the LAR form is widely used for long-term symptom control, while the aqueous form of octreotide is commonly used as rescue medication for the acute control of symptoms.5
Current consensus recommendations regarding LAR administration suggest an intramuscular (IM) dosing once every four weeks.5 The current FDA approval is for a maximal dose of 30mg/month. However, FDA regulations allow physicians to use higher doses at their discretion.The registration trials for this drug reported that up to 40% of patients require SC rescue medications weekly to control their symptoms, despite being on 30mg of octreotide per month overall.28 In the same trial, 70% of patients treated at doses of LAR 10, 20 or 30mg/month at some point over a six-month period required the use of rescue medication. In addition,Anthony et al.showed that, in current clinical practice, 20–40% of patients received LAR doses higher than the FDA-approved maximal dose (30mg/mo) to adequately control symptoms or to suppress tumor progression. The reasons for this are controversial and potentially multiple: the development of tachyphylaxis, an increased volume of tumor, an increase in the production of amines per a given volume of tumor, or the downregulation of sst 2 receptor number. Recently, Gunn et al. demonstrated that chronic in vitro exposure of sst 2 expressing cells to octreotide does not significantly change the sst gene copy number nor sst 2 binding to radiolabeled somatostatin analogs.Thus, the concept of sst 2 receptor downregulation is unlikely to be responsible for larger dose requirements of octreotide. However, a more plausible possibility is that circulating drug levels produced by current doses of octreotide are inadequate to completely saturate sst 2.Thus, patients may be requiring more octreotide simply because the drug levels achieved with 30mg/month LAR doses are not adequate to maximally suppress symptoms or tumor growth.
The Kd of octreotide for sst 2 is approximately 1nmol/l (1,000pg/ml).18,21 This level is often achieved in patients receiving LAR doses of 20mg/mo. A monthly dose of 30mg/month typically achieves a plasma octreotide level in the range of 5nmol/l (5,000pg/ml). While this level exceeds the Kd of octreotide for sst 2 by five-fold, clinically these patients still require rescue medication.Many authors have described patients receiving 10, 20, or 30mg of octreotide per month who, nonetheless, still experience symptoms that require excessive administration of rescue medication to gain symptom relief. Theoretically, octreotide’s maximal clinical benefit should be achieved by saturating sst 2, and this occurs in humans at a mean plasma level of approximately 11,000pg/ml in most, but not all, patients. Recent work by Woltering et al., using a blood test developed by InterScience Institute (Inglewood,CA), demonstrated that a monthly dose of 60mg of octreotide can achieve this desired plasma level, i.e. approximately 11,000pg/ml, in most, but not all, patients.
In the figure at the top, the dark line on each box-plot represents the median of the range, whereas the bottom and top of the solid box represents the 25th and 75th percentile of the plasma levels.The two reference lines are drawn at the Kd and saturation levels of the sst2 receptor. Only the 60 mg/mo LAR dose covers the concentrations that would saturate sst2. Circles and asterisks with values represent data that is out of range.The values below represent the mean plasma octreotide (pg/ml +/- SD) found at various monthly doses of Sandostatin® LAR. (LAR = long-acting repeatable.)
Individualizing Doses
These authors state that the dose required to achieve of this target level is variable and needs to be individualized. First, the target blood level is weight dependent. Figure 1 demonstrates that among all patients receiving 30mg of octreotide per month, heavier patients tended to have a lower drug level than did lighter patients.Thus, a larger LAR dose is required to achieve the therapeutic blood level in a heavier individual, while a smaller dose is needed in a lighter patient. In addition, the bioavailability of octreotide LAR is 60% compared to nearly 100% bioactivity of SC octreotide. This suggests that a larger dose of LAR may be required to achieve the same symptom control as seen with significantly lower doses of SC-infused aqueous octreotide. For these reasons, dosing needs to be individualized, and to this end, interval measurement of octreotide levels may be indicated.This measurement will be useful not only to assist the clinician in achieving an sst 2-saturating blood level, but it may also help differentiate a patient who has simply experienced a one-time ‘bad’ injection from one who chronically needs more medication.
In the authors’ practice, it is not uncommon to treat patients with 60mg/month (30mg every two weeks) of octreotide LAR, with some patients requiring as much as 120mg/month to achieve the target blood level. In our experience, patients have tolerated 60–100mg/month without any adverse complications. Other authors have demonstrated no significant toxicity in patients on doses as high as 6mg/day, and the octreotide drug trials report IV doses as high as 120mg administered over eight hours without serious ill effects. This safety profile provides the clinician with a great deal of latitude in selecting an appropriate dose for those patients whose symptoms are difficult to control. In addition, for patients who lack symptoms but are experiencing tumor growth, their clinician may be warranted in increasing the dose of octreotide with the hopes of achieving an antitumor effect. Forty per cent of patients on the FDA-maximal dose of 30mg/month of octreotide LAR require rescue medication weekly, and 70% of patients require rescue medication at some point in their therapy. Blood levels of octreotide in patients on this maximal dose approximate 5,000pg/ml. This level exceeds the Kd of sst 2, but does not completely saturate the receptor. In addition, the plasma blood level of this drug appears to be dependent on the weight of the patient, with heavier patients requiring a larger LAR dose.This may explain the need for frequent administration of rescue medication or the frequency of use of doses of LAR that exceed the 30mg/mo FDA guidelines. The standard regimen in our group is to base the starting dose of LAR on the patient’s weight. Accordingly, patients who weigh less than 70kg are starting on a dose of 20mg/month, while those weighing greater than or equal to 70kg are started on 30mg/month. Following three doses of LAR, a stable, steady-state level should be present, and a trough plasma level will be measured immediately prior to the next LAR dose. The plasma level of octreotide is then used to titrate the medication dose in order to achieve our target level.
High doses of LAR appear to be safe, and no toxic overdose has ever been reported in any patient to date. Although a dose of 60mg/month can achieve plasma levels that completely saturate sst 2 in most patients, dosing regimens should be individualized to the patient and monitored with trough steady-state octreotide levels.