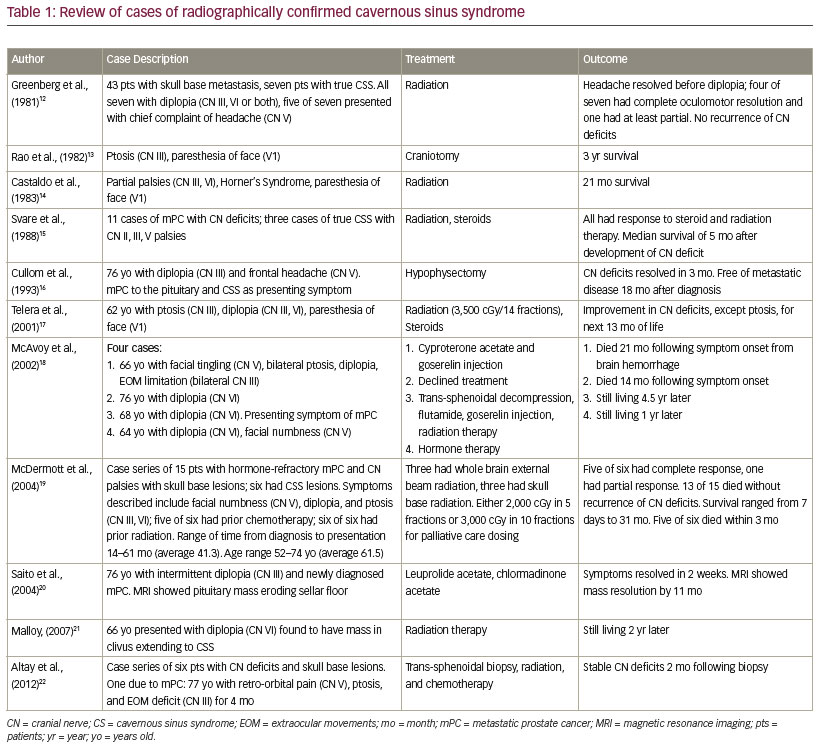
Cavernous sinus syndrome (CSS) is a rare clinical entity characterized by headache, ophthalmoplegia, and neuropathy due to compression of vascular and nerve bundles that course through a narrow anatomical region in the skull.1,2 Myriad conditions lead to this syndrome including bacterial or fungal infection, thrombus, aneurysm, pituitary enlargement due to tumor or apoplexy, and primary or metastatic cancers.1–3 Prostate cancer has predisposition for bone metastasis, and bone is the predominant site of metastasis; however, skull involvement is less common. Metastatic prostate cancer in the skull has been reported in 8–32% of patients after autopsy.4,5 A retrospective review of bone scans of patients with metastatic prostate cancer shows skull involvement in 14% of all metastatic sites.6 Bony metastasis causing CSS is rare. The exact incidence is unknown; although, several case reports of radiographically confirmed CSS due to metastatic prostate cancer have been published, and are summarized in Table 1.7–22 CSS can cause excruciating pain and disconcerting cranial nerve (CN) deficits, so its specific cause should be emergently evaluated. We report the case of metastatic prostate cancer causing CSS and present a review of the literature regarding the diagnosis and treatment of this rarely encountered condition.
Case summary
An 82-year-old gentleman with a history of castrate-resistant metastatic prostate cancer presented to his oncologist for evaluation of worsening headache, mild ptosis, and diplopia. Three weeks earlier he underwent intramedullary rod placement in his femur to stabilize an impending pathologic fracture, with a hospital course complicated by postoperative atrial fibrillation, anemia requiring blood transfusion, and suspected hypertensive emergency. During the admission he complained of progressive right-sided retro-orbital pain, mild right eye ptosis, and increasing inability to abduct the right eye. Symptoms persisted despite improvement in blood pressures. He was evaluated by the Ophthalmology Department which attributed his symptoms to residual effects of the hypertensive emergency. The Neurology Department was also consulted and felt his symptoms were consistent with dural inflammation from known bony metastasis of the calvarium and skull base, though no definitive lesion occupying the cavernous sinus was detected on initial magnetic resonance imaging (MRI). A secondary consideration was Tolosa–Hunt syndrome, an ophthalmoplegia due to idiopathic granulomatous inflammation.23 He was started on 60 mg of prednisone daily and discharged to undergo rehabilitation for his recent surgery.
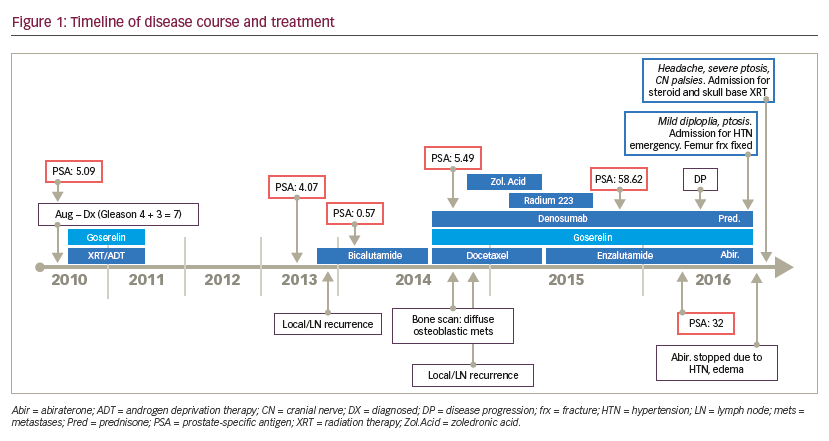
The patient had been diagnosed with localized prostate cancer (Gleason 4 + 3 = 7) 6 years prior and had undergone radiation therapy and androgen deprivation therapy (ADT) initially with goserelin and bicalutamide. He had controlled disease for 3 years before serial prostate-specific antigens (PSAs) demonstrated an acute rise from 0.42 ng/mL to 4.07 ng/mL over a several month interval. Computed tomography (CT) of the abdomen and pelvis (not shown) showed metastatic disease in L2 vertebral body and lymphadenopathy in the right iliac and right paraesophageal regions. He was restarted on ADT over the next 3 years. He ultimately progressed on ADT with widespread bone metastasis to the frontal bone, proximal femurs, iliac bone, and sternum for which he was treated with docetaxel and denosumab. He did not respond to docetaxel and was later treated with enzalutamide, abiraterone, and radium 223 in series (Figure 1). He had stopped abiraterone 2 weeks prior to the time of our encounter due to increasing PSA and the side effects of hypertension and edema.
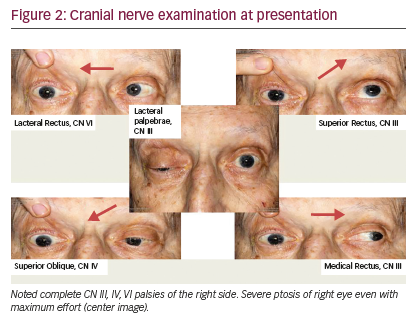
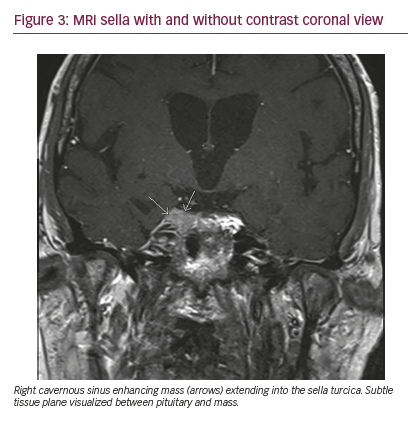
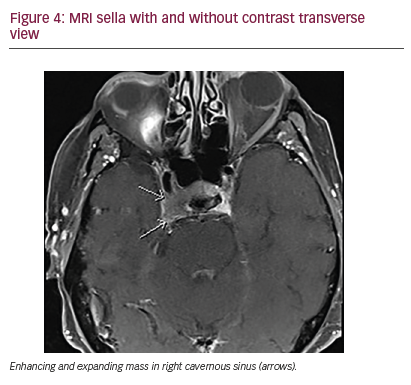
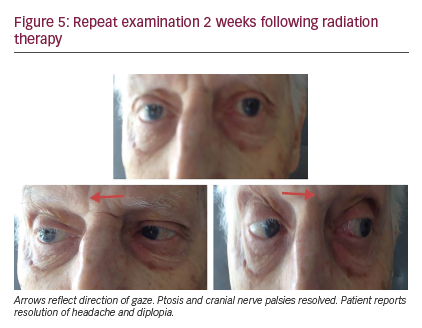
The symptom of retro-orbital pain had improved with steroid therapy during the initial admission but mild ptosis and diplopia persisted. In the several days prior to his visit in our clinic, the retro-orbital pain again worsened. At this point, what had been called retro-orbital pain was determined to be more consistent with a neuropathic burning pain along the CN VI distribution on the right side. In addition, he could no longer open his right eye even with great effort, and he now demonstrated palsies of CNs III, IV, and VI (Figure 2). The patient was admitted for further workup. A brain MRI demonstrated metastatic involvement of the cavernous sinus (Figures 3, 4). An increased dose of intravenous steroids was initiated along with aggressive pain control, and the Radiation Oncology Department was consulted for consideration of localized radiation to the offending bony metastasis. He was treated with 20-Gy dose of radiation in 5 fractions over the right cavernous sinus location over 7 days resulting in remarkable improvement in CN function with near resolution of ptosis and diplopia and complete resolution of the neuropathic pain (Figure 5).
Discussion
The cavernous sinuses are paired dural venous structures which lie on the base of the skull and are bordered by the bony sella turcica and the pituitary gland.2 Through these structures course the internal carotid artery, venules of the parasellar venous complex, oculosympathetic fibers and CNs III, IV, VI, as well as the ophthalmic (V1) and maxillary (V2) branches of CN V.1,2,12,24 The various neurovascular structures that pass through this relatively narrow window lie on the floor of the skull predisposing them to compression from any space-occupying lesions which arise in this area. Compression of these structures can result in palsies of the affected CNs III, IV, or VI, neuropathic pain in the distribution of the branches of CN V1 or V2, or Horner’s syndrome if the parasympathetic fibers are affected as well.1,2 CSS is characterized by any combination of these structures being affected.
CSS has a multitude of etiologies. Infection was classically cited as the most common cause, especially in the immunocompromised or those with poorly controlled diabetes.1 Thrombophlebitis from various bacterial and fungal infections like mucormycosis, aspergillosis, or actinomycosis, is included in this subset.1,25 These infections can gain access to the cavernous sinus through the valveless facial vein that supplies this region from the sinuses in the “danger zone” of the face.2 However, these classic findings are from an era before adequate antibiotics when infections were unrecognized and/or untreated and are much rarer today, except in more rural areas or developing countries where this etiology makes up a relatively greater percentage of cases.25,26 More common are various vascular abnormalities, which can cause expansion and space-occupying lesions within the cavernous sinus and include internal carotid artery aneurysm, carotid artery-cavernous sinus fistula, and venous thrombosis.27 An especially rare but described etiology includes the upward growth of a Rathke’s cleft cyst which can infiltrate and compress the structures of the sinus.28 Inflammatory causes such as herpes zoster, sarcoidosis, or idiopathic granulomatosis, also known as the Tolosa–Hunt syndrome, have also been implicated.1,2,7,23,29 However, one study has demonstrated that nearly 30%
of the cases of CSS are now due to neoplasms, making this now the most commonly recognized etiology.1 Neoplasms may be primarily intracranial such as hemangiomas and meningiomas,2 or result from local expansion as with pituitary adenomas or nasopharyngeal cancers,1,2 and lastly they may present as metastasis from more distant and varied primary cancers most commonly with prostate, breast, and lung but also with reports of colon, melanoma, thymic carcinoid, renal cell, and lymphoma.19,29–33
The predilection for metastatic prostate cancer to bone lends itself to causing just such a syndrome. However, while our review of the literature shows a few hundred cases of CSS reported, there are only a handful of cases that describe invasion of prostate cancer metastases into the cavernous sinus, specifically which are summarized in Table 1.12–15,17–22 Prostate metastases to other regions of the skull base, such as the sphenoid sinus, clivus, or petrous bone, with various neuropathies have been described in just a
few additional reports.9,10,19,34,35 This limited manifestation is remarkable given the prevalence of prostate cancer as there are an estimated 238,500 new cases of prostate cancer annually, accounting for 28% of all cancers diagnosed in men and making it the most commonly diagnosed cancer in males.36 There are an estimated 29,720 deaths related to prostate cancer which accounts for 10% of all cancer-related deaths in men, second only to lung cancer.36 Prostate cancer metastasizes primarily to lymph node and bone with 90% involving the spine, but also to lung in 50%, liver in 25%, and brain much less often and only after an average of 5 years of active
disease.7 In total, only about 4% of all cancers will metastasize to the base of the skull,12 and while prostate cancer is the primary contributor, at 38.5% per one extensive review of 279 cases in the literature,37 it rarely affects the cavernous sinus causing CSS.12 Regardless, prognosis is poor with estimates of median survival of 1 year with skull base metastasis and only 5 months if CNs are affected.11 Despite its rarity, the morbidity associated with CSS mandates a thorough evaluation.
CSS is a medical emergency and urgent diagnosis and treatment must be sought in order to best preserve functionality. Diagnosis requires a high index of suspicion and correlation with history and physical examination. A head CT can help screen for other causes, but in instances of early stage metastasis, it can often miss the diagnosis for a period of weeks to months until the lesion becomes radiographically evident; therefore, MRI is the gold standard for detecting neoplastic etiologies and can differentiate even small lesions affecting the CNs and soft tissues.1,3 Ordering an MRI with a focus on the sella turcica may help elucidate the structures involved.2,8 Caution should be taken as only 70% of cases have radiographic confirmation at time of symptom presentation; therefore, if the primary etiology of CSS is thought strongly to be metastatic cancer, treatment should be considered to relieve symptoms and prevent further neurologic damage even in absence of definitive radiographic evidence of the offending lesion.8 Treatment will depend on etiology, but in cases of metastatic or primary malignancy, high-dose steroids, as was done for this patient, can rapidly reverse symptoms if there is surrounding edema and can slow progression until more focused radiation therapy can provide more lasting relief.8 In fact, skull base radiation therapy may improve pain and CN deficits in 50–90% of cases with resolution of deficits often until time of death.37,38 In this patient, radiation therapy provided remarkable improvement in symptoms and resolution of CN deficits; however, given the extent of systemic disease, the patient still had a poor outcome. Earlier aggressive efforts might spare these unfortunate patients’ significant morbidity associated with this condition, and every effort should be made to address prompt treatment if clinical history and examination suggest the possibility of CSS.













