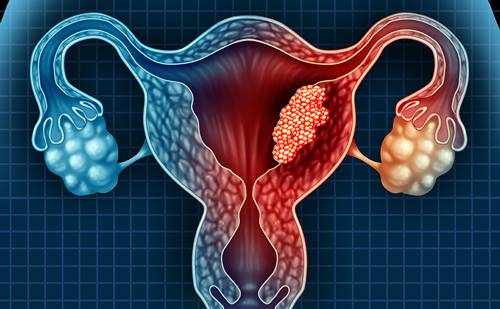
Cervical cancer remains one of the leading causes of cancer-related morbidity and mortality worldwide, and is the fourth leading cause of cancer death in women.1 Human papilloma virus (HPV), particularly types 16 and 18, is significantly associated with subsequent development of cervical cancer, with an increased risk also seen among smokers.2 Cervical cancer incidence has decreased in developed countries since the widespread introduction of cervical screening.3 However, it remains a major health problem in countries without screening programs and in disadvantaged communities within developed countries with screening programs.2,4,5 For example, indigenous Aboriginal and Torres Strait Islander women have double the incidence and five times the mortality risk than other Australians.6–9
Many patients with cervical neoplasia have early lesions detected by Pap smear, which are curable with surgery. However, screening rates are low in women from disadvantaged areas, even in developed countries. Hence we continue to see women present with locally advanced diseases who have much lower cure rates.10–12 In addition, there difficulties continue with detecting the precursors of adenocarcinomas using Pap smears.
The development of the cervical cancer vaccine is a major advance, which will reduce cervical cancer rates for future generations. Realizing the benefit of the vaccine is predicted to take some time given that the incidence of cervical cancer continues to rise with age, and that ongoing screening will be required in addition to the vaccine program, which needs to be initiated prior to the age of commencement of sexual activity to be effective. The current vaccine that has been in clinical use is predicted to protect against 70 % of cervical cancer, but does not provide protection for the 30 % of chronic infections by HPV types other than HPV 6, 11, 16, and 18 and has no role in the treatment of established cancer.1 However, in December 2014, the US Food and Drug Administration (FDA) approved a nonavalent vaccine, which offers protection against seven high-risk HPV subtypes and appears even more effective. A UK modeling analysis suggests that 60 years of an ongoing vaccination program of 12-yearold girls at 80 % coverage will be required to see a 38–82 % reduction in cervical cancer incidence if vaccine protection lasts for 20 years on average.13 Unfortunately, many countries worldwide still have neither screening nor vaccination programs so the need to treat locally advanced cervical cancer will remain a problem in our community for many years and needs ongoing research.
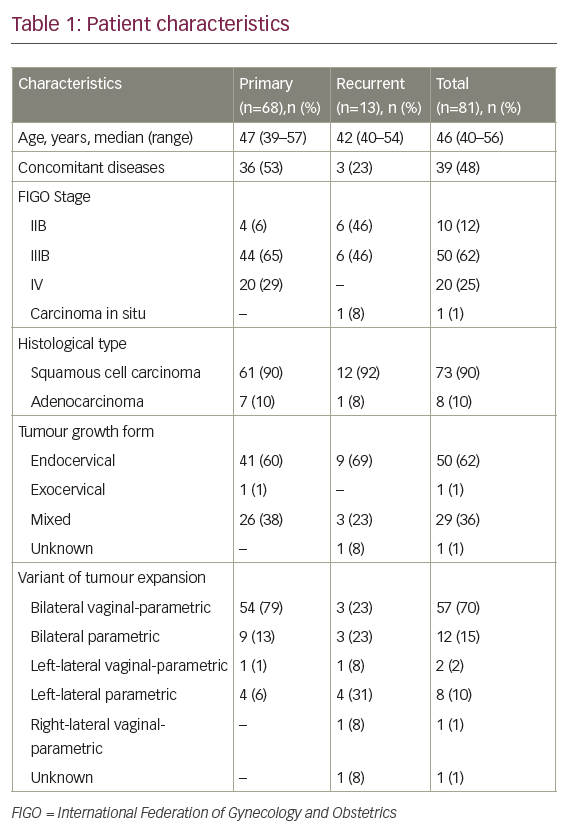
The use of low-dose chemotherapy concurrent with pelvic radiation has been proven to improve survival for locally advanced cervical cancer.14 The Medical Research Council (MRC) individual patient data meta-analysis found that the addition of concurrent chemotherapy to radiation increased the 5-year overall survival rate by 6 % (HR 0.81: 60 versus 66 %).15 On the basis of the studies in this analysis, weekly cisplatin at a dose of 40 mg/m2 during pelvic radiation has become the standard of care for the treatment of locally advanced disease. However, the 5-year disease-free survival rate was only 58 % in the chemoradiation group, which, although superior to 50 % with radiation alone, still leaves significant room for improvement. Although chemoradiation is a generally effective treatment for the primary disease, those who relapse tend to develop distant metastatic disease, and often die from their disease in under a year.16
Recognized pretreatment disease factors that predict worse outcomes with standard chemoradiation include a larger tumor volume, particularly if >50 cc; a higher International Federation of Gynecology and Obstetrics (FIGO) stage; uterine corpus invasion; nodal involvement; and continued smoking.17–19 Although nodal involvement is not part of the current clinical FIGO staging system, this can be noninvasively determined using positron emission tomography–computed tomography (PET/CT), with a reported sensitivity of approximately 75 % and specificity of 92 %.20,21
Although the development of distant disease after chemoradiation is the predominant cause of treatment failure, local relapse remains a problem that causes significant morbidity. In the meta-analysis, locoregional treatment failure was responsible for 35 % of the failure events across trials. Standard radiation treatment usually involves 45–50.4 Gy of external beam radiation therapy (EBRT) delivered in fractions of 1.8–2 Gy to the pelvis ± a parametrial or nodal boost. In addition to EBRT, brachytherapy direct to the primary is considered to be essential to give a sufficient curative dose to the primary. There is a recent concern about declining use of brachytherapy as part of chemoradiation in some countries, such as the US. Instead there has been interest in using more modern forms of radiotherapy, such as intensity modulated radiation therapy or stereotactic radiotherapy, which may be less labor intensive, be associated with higher clinician reimbursement, and not require specific brachytherapy training. However, recent reports from large prospective databases suggest that survival rates are clearly inferior in those women who do not receive brachytherapy.22–24 Ongoing approaches to try and optimize brachytherapy include the use of conformal brachytherapy to prescribe the dose to the residual tumor at the end of EBRT rather than the historical point A as well as the use of image guidance using either magnetic resonance imaging (MRI) or ultrasound to ensure the tandem is accurately placed within the uterus to minimize toxicity and maximize efficacy.25,26
A variety of approaches to intensifying the concurrent chemotherapy component of chemoradiation have been tested, such as adding additional systemic therapy. However, to date no additional regimen has been found to be significantly superior to cisplatin 40 mg/m2 weekly. The meta-analysis does suggest efficacy from nonplatinum regimens, and substituting other agents such as carboplatin or fluorouracil may be considered for women with contraindications to cisplatin.27,28 A variety of clinical trials have concluded that adding additional agents to cisplatin (such as gemcitabine, paclitaxel, tirapazamine, and cetuximab) have increased toxicity rates without clearly improving outcomes.29,30 More promising results have been seen with recent small single-arm trials, which have added bevacizumab or triapine to cisplatin, and these approaches may be further evaluated in further randomized trials.31,32
Given the main cause of treatment failure is distant metastasis, it may be that adding further chemotherapy to chemoradiation will help. A subset analysis of the MRC meta-analysis involving two trials, which gave additional adjuvant chemotherapy after chemoradiation showed an impressive absolute improvement of 19 % in 5-year survival (from 60 % to 79 %) compared with radiation alone.33,34 More recently, Duenas- Gonzalez et al. showed a benefit of adding concurrent gemcitabine to standard cisplatin-based chemoradiation, followed by two further cycles of adjuvant cisplatin-gemcitabine. This multicenter randomized phase III trial performed in South America showed a statistically significant 9 % improvement in the primary outcome of progression-free survival at 3 years (65–74 %).35 Limitations of the study include concern about toxicity rates (grade 3–4 toxicities 86.5 versus 46.3 %), as well as the fact that follow-up data were truncated at 1 year.16,36 It remains unclear how much the additional chemotherapy given concurrent with radiation improved outcomes, as opposed to increasing toxicity, with a recent randomized trial addressing this question closed early for futility.37 It is possible that the two cycles of adjuvant chemotherapy were the part of the treatment of most benefit. There is sufficient evidence to suggest a potential role for adjuvant chemotherapy to result in this being further assessed in the ongoing randomized OUTBACK trial of the Gynecologic Cancer InterGroup (GCIG), which is testing whether or not giving four additional cycles of carboplatin and paclitaxel after standard chemoradiation can improve overall survival rates (NCT01414608). Other approaches being tested in ongoing international randomized trials include the value of adding additional neoadjuvant chemotherapy prior to chemoradation (NCT01566240), and comparison of three weekly with weekly cisplatin chemotherapy during radiation (NCT01561586). There is also interest in testing shorter radiation fraction schedules that may be easier and more practical to deliver in areas of the developing world where access to radiotherapy machines remains problematic. As the majority of the burden of cervical cancer is seen in the developing world, it is essential that ongoing efforts continue to improve access not only to preventive measures such as screening and vaccination but also to treatments and clinical trials for those who present with established disease.