Soft-tissue sarcomas (STSs) should be managed by multidisciplinary teams, including specialist surgeons, radiation oncologists, medical oncologists, pathologists and radiologists. The aim of radical treatment for any STS should be to achieve the best possible local control rates with as little treatment-related morbidity and adverse effect on quality of life, as possible. Combination surgery and radiotherapy is currently regarded as standard treatment for STS of the extremity.1
Soft-tissue sarcomas (STSs) should be managed by multidisciplinary teams, including specialist surgeons, radiation oncologists, medical oncologists, pathologists and radiologists. The aim of radical treatment for any STS should be to achieve the best possible local control rates with as little treatment-related morbidity and adverse effect on quality of life, as possible. Combination surgery and radiotherapy is currently regarded as standard treatment for STS of the extremity.1
This article examines the treatment of non-metastatic STS, particularly the use of radiotherapy as an adjunct to limb-preserving surgery. The arguments for and against neoadjuvant, intraoperative, adjuvant or no radiotherapy will be discussed.
In the 1960s it was shown that radiotherapy alone could produce complete histological response in STS, dispelling the long-held belief that all sarcomas were radioresistant.2 STSs have variable degrees of radiosensitivity. Some subtypes such as myxoid liposarcoma are very radiosensitive while others, such as malignant peripheral nerve sheath tumours (MPNST), are less so. The predicted radiosensitivity of any sarcoma should be considered when deciding on the most appropriate treatment regimen for an individual patient.
In most centres in Europe and North America, radiotherapy is given as external beam techniques (external beam radiotherapy [EBRT]). Brachytherapy is another technique of administering radiotherapy usually in the intraoperative setting.
The major therapeutic goals when treating extremity STS are patient survival, local tumour control, maximising limb function and minimising morbidity from treatment. Treatment-related morbidity can cause considerable physical and psychological disability resulting in reduced quality of life. New treatment paradigms for sarcoma should concentrate not only on local control and survival but also on the consequences of the treatment itself.
Neoadjuvant (Preoperative) Radiotherapy
Historically neoadjuvant radiotherapy has been used in extremity STSs where upfront limb-conserving surgery is considered difficult. If shrinkage of the sarcoma could facilitate conservative surgery then radiotherapy may be tried. This approach requires extensive collaboration between radiologists, surgeons and radiotherapists. It is generally accepted if a sarcoma is truly unresectable without an amputation then neoadjuvant treatment, either radiotherapy or chemotherapy, is unlikely to render the tumour operable. Over the last 15 years, neoadjuvant radiotherapy has become the standard of care in several countries, particularly Canada. Trials have shown equivalent local control and survival rates to adjuvant radiotherapy.3 The toxicity profiles are different, with increased acute wound complications with neoadjuvant radiotherapy and increased late toxicities with adjuvant radiotherapy (see section below).
Traditional Response Evaluation Criteria In Solid Tumors (RECIST) criteria for neoadjuvant radiotherapy in STSs are not reliable predictors of pathological response. Myxoid liposarcomas are extremely radiosensitive tumours that frequently show 100 % necrosis after neoadjuvant radiotherapy.4 Traditional RECIST radiological reporting in these cases usually report stable disease or no response to treatment. This is clearly not the case, and radiologists who are experienced in sarcoma radiology and the radiological changes in response to treatment are crucial in the discussion of these patients’ management.5
Surgery is usually planned for four to six weeks postneoadjuvant radio therapy to allow for any cytoreduction to occur, but before late toxicities such as fibrosis and oedema that could make surgery more difficult.
Adjuvant (Postoperative) Radiotherapy
Potter et al.6 first reported that limb-preserving surgery with radiotherapy had equivalent local control results to amputation in extremity STS patients without affecting overall survival. Adjuvant radiotherapy then became standard of care after the results of several non-randomised studies and one randomised controlled study suggested limb-preserving surgery combined with radiotherapy appeared to give similar disease control but with significantly improved patient function.7 In the only randomised controlled trial (RCT), 91 high-grade extremity STSs were randomised between adjuvant chemotherapy alone or adjuvant chemotherapy plus adjuvant radiotherapy. In the radiotherapy arm, no local recurrences were seen while in the surgery and chemotherapy alone arm the local recurrence rate at 10 years was 22 %. There was no difference in overall survival and indeed no trial to date has reported any survival advantage with adjuvant radiotherapy. Radiotherapy at doses between 50–66 Gy can eradicate microscopic disease beyond the gross lesion. With combined modality treatment, most centres report local control rates between 85–90 % for high-grade extremity STS.
Indications for adjuvant radiotherapy follow European Consensus Guidelines and have recently been supported by UK guidelines on the management of STSs.8 Nearly all intermediate or high-grade STSs require postoperative radiotherapy. Low-grade tumours are unlikely to need radiotherapy unless they are large, deep and have been incompletely resected, with further surgery likely to compromise function.
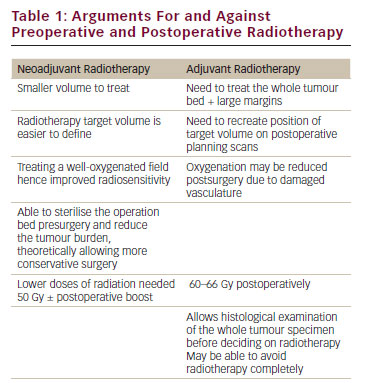
Arguments for Preoperative or Postoperative Radiotherapy
The theoretical radiobiological arguments in favour of neoadjuvant or adjuvant radiotherapy can be seen in Table 1. The only phase III RCT comparing neoadjuvant and adjuvant radiotherapy was performed in Canada by O’Sullivan et al.3 One hundred and ninety patients with extremity STS were randomised to either neoadjuvant or adjuvant radiotherapy. The neoadjuvant group received 50 Gy presurgery with a postoperative boost of 16–20 Gy if the surgical margins were involved. The adjuvant group received 66 Gy. Primary and secondary endpoints included acute and long- term complications, the impact of morbidity on patient function, local recurrence rates and overall survival. The study was terminated early when at interim analysis, with a mean follow up of 3.3 years, acute wound complications were significantly higher in the neoadjuvant radiotherapy arm compared with the adjuvant radiotherapy arm (35 versus 17 %; p=0.01). The latest update at nearly seven years has shown no difference in local control rates between the two arms. Similar results for progression-free and overall survival are reported. However, late grade 2–4 toxicity was significantly higher in patients receiving postoperative radiotherapy (86 versus 68 %). This is predominantly due to an increase in subcutaneous tissue fibrosis causing either severe induration and loss of subcutaneous tissue or contracture >10 % (grade 3) or tissue necrosis (grade 4). With neoadjuvant radiotherapy, the incidence of grade 3–4 fibrosis was 23 % versus 36 % with adjuvant radiotherapy. Late limb oedema and joint stiffness were also more common in patients having adjuvant radiotherapy, but this did not reach statistical significance.9,10
Patients in the study who developed grade 2 or higher fibrosis, joint stiffness or oedema had significantly lower functional scores as measured by the Musculoskeletal Tumour Rating Scale (MSTS) and the Toronto Extremity Salvage Score (TESS).
Brachytherapy
Brachytherapy is the insertion of radioactive sources into a tumour or tumour bed. Compared with external beam radiotherapy it minimises the dose to normal tissue, theoretically reducing late complications, and reduces overall treatment time. Afterloading catheters are placed at the time of surgery to the tumour bed and area at risk of recurrence as defined by the sarcoma surgeon.
A phase III RCT comparing postoperative brachytherapy (45 Gy) versus no radiotherapy was carried out with 164 patients with either extremity or superficial trunk STS. Local control at five years was superior in the radiotherapy arm (82 versus 69%). In a preplanned subgroup analysis, the improvement in local control was seen only in the high-grade subgroup and not in the low-grade subgroup. As in previous radiotherapy sarcoma trials, there was no difference in overall survival.
11 There have been no RCTs comparing EBRT and brachytherapy for either efficacy or morbidity. In the UK, the lack of brachytherapy limits its routine use in sarcoma practice.
Surgery without Radiotherapy
Surgical resections are divided into R0, R1 and R2 as classified by the Union Internationale Contre le Cancer (UICC). R0 resections have clear margins (in sano), R1 have (possible) residual microscopic disease and R2 residual macroscopic disease. There have been various surgical tactics ranging from ablation to conservative surgery for STSs and the evidence for surgery in STS alone is limited. In recent times, surgery has tended to be less extensive rather than more.
The French Sarcoma Group found a fourfold difference in local recurrence rate between R0 and R1 resections.12 Larger tumours have been shown to have an increased likelihood of R1 resection.13 Inadequate resections have been demonstrated to show a doubled risk of local recurrence, but local recurrence and metastatic disease have not been shown to have a causal relationship.
In a series from the Mayo clinic, treated by surgery alone, there was a five-year local recurrence rate of 20 %. This was however with a mixed population and only five deep, high-grade tumours. The recurrence rate in high-grade tumours was 40 %.14 They concluded irradiation could be withheld in low-grade tumours with clear resection margins in whom a functional salvage could be obtained in the event of recurrence.
Cahlon from the Memorial Sloan-Kettering Cancer Center in New York looked at 200 patients treated by surgery (with negative margins). They concluded that patients less than 50 years of age with stage 1 and 2 disease could safely be treated with surgery alone, but those with stage 3 disease or over 50 should have adjuvant treatment.15
From a heterogeneous series from Aarhus unfavourable factors for local recurrence were advanced age, high-grade, lower-extremity tumours and large size (>5 cm).16
From the relatively limited data available, surgery alone is applicable for small (<5 cm), low-grade tumours in the under 50s. Patients with high grade or large tumours or aged over 50 years should all be considered for adjuvant radiotherapy.
Advances in Radiotherapy
Recently, there have been dramatic advances in radiotherapy with the introduction of Intensity Modulated Radiotherapy (IMRT ). IMRT allows more conformal radiotherapy plans and spares more of the normal tissues from high-dose radiation. Theoretically this should lead to reduced normal tissue toxicity when used either in the neoadjuvant and adjuvant setting. Single-centre studies have looked at using IMRT for neoadjuvant radiotherapy with the intention of sparing the subcutaneous tissue where the surgical incision and primary closure will be made in an attempt to reduce acute wound complications, to reduce the dose to the bone (particularly the femur) and reduce the fracture risk. IMRT has not been compared directly with standard computerised tomography planned conformal radiotherapy in the setting of a RCT.17
Complications of Treatment
Acute toxicity from radiotherapy is defined as an adverse event occurring during or within six months of the radiotherapy. This usually causes major wound complications. Late radiation toxicity occurs after six months and includes subcutaneous tissue fibrosis, oedema, joint stiffness, bone fracture and osteonecrosis. Toxicities both acute and late are dependent on the anatomical position of the sarcoma and the normal tissue surrounding it.
Wound Complications
The major surgical concern of preoperative radiotherapy is wound complications. These have been shown to be higher in the proximal lower extremity than at other sites. A series of 317 patients from the University of Florida revealed a 50 % wound complication rate in STSs resected from the medial thigh.18
Wound complications occurred in 44 % of patients treated by induction radiotherapy in Melbourne, Australia. The rate was similar whether the wounds had been closed primarily, by skin grafting or by a flap. There was an increased risk of complications in patients over 40 years of age.19 Surgery was, however, carried out less than three weeks from completion of radiotherapy. Imaging reveals an incidence rate of seroma of 7.7 % (2/26) for surgery alone and 76 % of surgery with radiotherapy.20 Treatment-related osteoporosis occurred in 19 % and 28 % of the treatment groups, respectively. Twelve patients developed lower limb osteoporosis: five were in the surgery alone group and six in the surgery and radiotherapy group of which there were one and five pathological fractures, respectively.
Pathological Fractures
Post-irradiation pathological fractures can be difficult to manage and troublesome to heal. Incidence varies from 2 % to 10 %.18,21,22 In the largest series from Toronto, the major risk factors were for females, over 50 years of age and pertained to the proximal femur. Maintainance of a mean bone dose of less than 37 Gy reduced the risk of fracture.21
The volume of bone irradiated is an important risk factor in determining risk of radiation-induced fracture. Extensive periosteal stripping, particularly of the proximal femur, should alert the surgeon to the risks of radiationinduced fracture and prophylactic fixation should be considered. While pathological fracture can occur, even after prophylactic stabilisation, they often do not require additional surgical management.22
Summary
The decision between neoadjuvant and adjuvant radiotherapy comes down to what is more tolerable: acute, usually reversible wound complications, or late, usually irreversible complications. In upper limb sarcomas very few acute wound healing complications are seen irrespective of radiotherapy or not. The Canadian authors recommend that this group of patients should preferentially receive neoadjuvant radiotherapy. For lower limb sarcomas, the jury is still out.
In the UK, many sarcoma specialist centres are recruiting to the VORT EX study. This is a National Cancer Research Network (NCRN)- run RCT looking at adjuvant radiotherapy. In the experimental arm, smaller treatment fields are used on the basis that the majority of sarcoma recurrences occur within 2 cm from the original tumour. The investigators are hoping that the traditional very large radiation fields may no longer be needed and that toxicity may be reduced while still maintaining excellent local control rates. Larger field sizes are known to correlate with an increased incidence of fibrosis and joint stiffness. While centres are recruiting to this study the widespread introduction of neoadjuvant radiotherapy is unlikely to occur.
For each individual sarcoma patient, the multidisciplinary team should discuss and agree local therapy (both primary and adjuvant therapy) prior to surgery to optimise outcomes. Consideration should be given to the functional deficits and complications expected from all modalities used for local control.
Patients need to be involved in treatment decisions and informed consent should be received in terms of possible complications. Any one individual may have a different view on what is an acceptable functional outcome.
Available evidence suggests that only patients with small, low-grade tumours under the age of 50 years should be spared radiotherapy. This age has not been ratified in large studies.