Non-Hodgkin’s lymphoma (NHL) is a heterogeneous group of lymphoid malignancies that most commonly occur in individuals over the age of 60 years. Aggressive (high-grade) subtypes progress rapidly but are potentially curable, whereas indolent (low-grade) subtypes grow more slowly but usually relapse after conventional treatment. The introduction of immunotherapy and its combination with chemotherapy greatly improved remission rates compared with chemotherapy alone in NHL; more recently, the combination of immunotherapy plus yttrium-90 (90Y) or iodine-131 (131I) radiation has shown much greater efficacy than immunotherapy alone and may improve overall survival (OS).
The greatest challenge in NHL is keeping patients in remission once they have responded to therapy. Conventional chemotherapy for indolent lymphoma has a high response rate, but relapses will occur. Although patients may respond to salvage therapy, the duration of remissions decreases progressively. High-dose chemotherapy (HDC) with autologous stem cell transplantation (ASCT) has been shown to increase progression free survival (PFS) with a two-year probability of 70%;1 however, the curative potential in these patients is unclear.
Rationale for Using Yttrium-90–Ibritumomab Tiuxetan in Autologous Stem Cell Transplantation
NHL is inherently radiosensitive, providing a rationale for using radiation to treat lymphomas, and the targeted delivery of radiation directly to tumour sites is better tolerated and more efficient than total body irradiation (TBI). The principles of radiolabelled immunotherapy, which allows targeted delivery of a therapeutic dose of radiation not only to the surface of tumour cells at multiple sites but also to neighbouring deeper cells, have been reviewed extensively in recent publications.2–4 The only radiolabelled immunoconjugates currently approved for the treatment of NHL are 90Y–ibritumomab tiuxetan and 131I–tositumomab (Bexxar®, GlaxoSmithKline, US; only approved in the US), both of which are directed against the CD20 cell surface antigen. 90Y-ibritumomab tiuxetan comprises the anti-CD20 monoclonal antibody ibritumomab, conjugated via the tiuxetan chelator to the pure beta-emitting radioisotope 90Y. It is currently approved for the treatment of adult patients with rituximabrelapsed or -refractory CD20-positive follicular B cell-NHL, and is the only therapy approved for use after rituximab failure. Adverse events with 90Y–ibritumomab tiuxetan are predictable and manageable, with the primary toxicity being transient reversible haematotoxicity, as expected.
No preparative regimens prior to ASCT have been shown to be clearly superior and none has ever been tested in a randomised study. Fractionated TBI has been used in the past, especially in indolent lymphoid malignancies, with encouraging results, but is not recommended for patients above 60 years of age or for those treated with previous radiotherapy.
Therefore, radiolabelled immunotherapy agents such as 90Y– ibritumomab tiuxetan are likely to play an increasingly significant role in ASCT by increasing the efficacy of the conditioning regimen and reducing the relapse risk. Owing to its good tolerability profile, the use of 90Y–ibritumomab tiuxetan at high doses as the sole conditioning agent in place of HDC is also showing promise, and may allow transplantation in patients who cannot tolerate the more aggressive conditioning regimens, such as the elderly or those with co-morbidities (especially cardiovascular disease). The dose-limiting toxicity of radiolabelled immunotherapy is haematotoxicity, which can be circumvented by ASCT and may allow further dose escalation.
Standard-dose Yttrium-90–Ibritumomab Tiuxetan Associated with BEAM Chemotherapy plus Autologous Stem Cell Transplantation
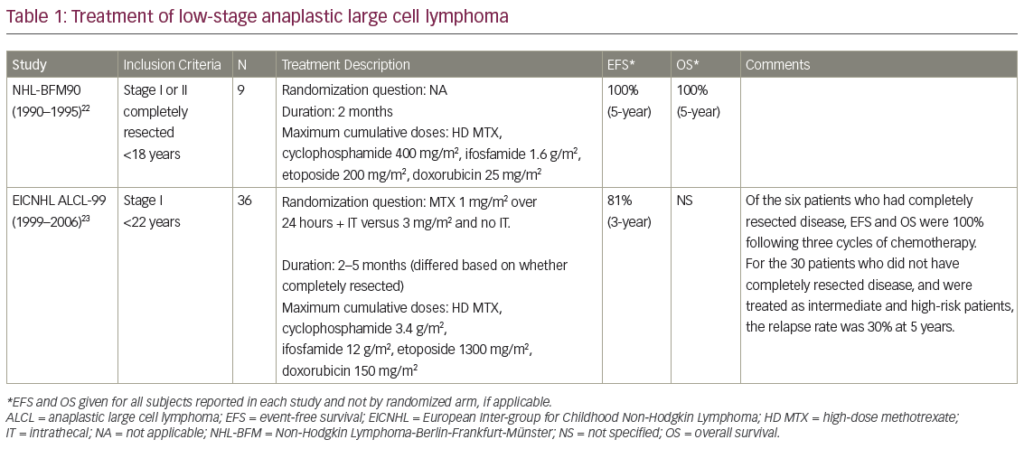
Experience has been gained in several phase II studies with the combination of Zevalin with other conditioning regimens before auto- or allotransplantion.5 The Groupe d’Etude des Lymphomes de l’Adulte (GELA) in France investigated the Z-BEAM conditioning regimen prior to ASTC in patients with relapsing low-grade NHL.6 Radiolabelled immunotherapy 90Y–ibritumomab tiuxetan (Zevalin) is effective in B-cell lymphoma and delivers targeted radiation without TBI toxicity. To take advantage of this antilymphoma effect, a conventional dose of 90Y–ibritumomab tiuxetan 15MBq/kg (maximum total dose 1,200MBq) was given without dosimetry on day -14 before ASCT and combined with a standard-dose BEAM regimen starting at day -7.
The goal of this phase II study was to evaluate the efficacy and toxicity of Z-BEAM. Patients <65 years of age with CD20+ low-grade B-cell lymphoma in first or second relapses, or not achieving complete remission after first-line treatment, were included in the trial. They had to be chemosensitive to prior salvage therapy, have had no more than three lines of treatment and be eligible for ASCT. The primary end-point was to detect a two-year event-free survival (EFS) rate of at least 80%.
Haematological reconstitution was evaluated after transplant and during the first year of follow-up. Between March 2005 and August 2006, 77 patients were included. Patient characteristics at last salvage chemotherapy inclusion were: 68 follicular lymphoma, six marginal zone and one mantle cell plus two transformed histology after pathological review; median age 53 years (range 31–64); follicular lymphoma international prognostic index (FLIPI) low-risk 32, intermediate-risk 20, high-risk 20; and 24 bone marrow involvement. Thirty-nine patients had first relapse, 10 second relapse, 21 partial response (PR), four stable disease and three progressive disease after first-line treatment.
Median delay between first-line therapy and ASCT was 31 months and median delay between last salvage and ASCT was 4.4 months. Response rates before ASCT were complete response (CR) and complete response unconfirmed (CRu) 77%, PR 22% and stable 1%. As first-line treatment, patients received mostly cyclophosphamide, doxorubicin, vincristine and prednisone (CHOP), associated in 29 cases with rituximab. Twenty-nine patients received a second-line chemotherapy with rituximab in 22 cases prior to last salvage chemotherapy; 49 patients after first-line treatment received directly after relapse another line of chemotherapy before ASCT. Overall, among the 77 patients, last salvage chemotherapy regimen included rituximab in 74, and ASCT was performed in 75. The haematological reconstitution after Z-BEAM followed by ASCT in 75 patients was: time to neutrophils >1g/l 12 days (9–35) and time to platelets >20g/l 12 days (range three to 42).
Median number of platelet transfusions was four; median number of red blood cell transfusions was two. Grade 3–4 toxicities were infection (83%), mucositis (47%) and pulmonary (4%). Safety data indicated 35 serious adverse events in 24 patients; these did not appear to significantly differ from those usually seen after ASCT is performed. No cases of toxic death were observed. At weeks 12 and 42 after ASCT, median haemoglobin levels were 11.6g/dl and 11.3g/dl, respectively. Median platelets counts were 111g/l and 148g/l and leukocyte counts were 3.48g/l and 4.80g/l, respectively. After transplant, 91% of the patients were in CR or CRu. Only five adverse events were reported. After a minimum follow-up of one year for all patients, estimated event-free survival (EFS) was 93%. Z-BEAM is a safe conditioning regimen that can be used for B-cell lymphoma. Longer follow-up is necessary to evaluate long-term toxicity and efficacy.
The Z-BEAM regimen is used in other types of lymphoma, for example in those patients who are ineligible for TBI due to older age or prior radiotherapy. The group of City of Hope was a pioneer in their domain and reported their experience7 of a study of 41 patients with a median age of 60 years. Disease histology were diffuse large B-cell (n=20), mantle-cell (n=13), follicular (n=4) and transformed (n=4) lymphoma. There was a median follow-up of 18.4 months and the estimated twoyear OS and PFS were 88.9 and 69.8%, respectively.
Shimoni and others8,9 have investigated the inclusion of standard-dose 90Y–ibritumomab tiuxetan in the conditioning regimen prior to ASCT in refractory, aggressive NHL expected to have poor outcome with standard conditioning (see Table 2). Presence of active disease was determined using positron emission tomography (PET) and computed tomography (CT) scanning. Overall, 11 patients had primary refractory disease, 12 had refractory relapsed disease and 14 had bulky disease at transplant. Patients received the Z-BEAM conditioning regimen. All patients engrafted rapidly, in a median of 10 days (range 10–22 days).
Overall, 16 of 21 evaluable patients achieved a CR (76%): 11 achieved a CR, nine achieved a PR, of whom five converted to CR with additional radiation therapy to eliminate residual disease. After a median follow-up of 17 months (range six to 27 months), 16 of 23 patients were alive. Non-relapse mortality at day 100 in these heavily-pre-treated refractory patients was 9% (95% confidence interval [CI] 2–33). There was no apparent additional toxicity related to the use of 90Y–ibritumomab tiuxetan and the investigators concluded that its inclusion in this conditioning regimen was relatively safe and improved outcomes in patients with refractory lymphoma.
Escalating-dose 90Y–ibritumomab tiuxetan (0.3–1.2mCi/kg) plus high-dose BEAM was investigated in a phase I trial of relapsed or refractory CD20-positive NHL.10,11 Based on dosimetry results, patient-specific doses of 90Y–ibritumomab tiuxetan calculated to deliver escalating radiation doses (300–2,100cGy) to critical organs (liver, lung or kidney) were administered. The median age of the patients was 54 years (range 25–72 years) and most had received three or more treatment regimens, including rituximab. The toxicity profile of the 90Y–ibritumomab tiuxetan-containing conditioning regimen was similar to that seen with high-dose BEAM alone. The most common grade III or IV toxicities were infection, fever, stomatitis, nausea, vomiting, diarrhoea, haemorrhage and oedema. Engraftment was rapid and three-year OS and PFS rates were good.
Tolerability
These preliminary data indicate that 90Y–ibritumomab tiuxetan at standard- and high-/escalating-dose was well tolerated as a component of transplant-conditioning regimens. Toxicity profiles were similar to those seen with other high-dose regimens such as TBI, etoposide and cyclophosphamide, with no additional toxicity and no adverse events or allergic reactions specifically attributed to 90Y–ibritumomab tiuxetan.
Adverse events observed following 90Y–ibritumomab tiuxetan plus HDC and transplant were as expected and included skin rashes, nausea/ vomiting, mucositis, infection and cardiac, pulmonary and hepatic toxicity. In studies where 90Y–ibritumomab tiuxetan was the sole myeloablative agent, adverse events were as expected for monotherapy (neutropoenia, infections) and were relatively mild. The most frequent, severe complications normally seen with conventional HDC conditioning were not observed. Tolerability findings were similar in 131I–tositumomab studies; abnormal levels of thyroid-stimulating hormone were also frequently observed following 131I–tositumomab-based conditioning.
Conventional chemotherapy for NHL is associated with an increased risk of myelodyspalstic syndrome. This usually develops within 10 years of treatment exposure. Analysis estimated the risk of myelodysplastic syndrome or acute myeloid leukaemia in NHL patients receiving high-dose chemotherapy and ASCT to be between 5 and 10%. Clinical data for 90Y–ibritumomab tiuxetan in 746 patients reported 17 myelodysplastic syndromes, with an annualised rate of 0.7% from the time of treatment, indicating that there is no increase in risk compared with conventional chemotherapy.12
Current and Future Directions for Yttrium-90–Ibritumomab Tiuxetan in Autologous Stem Cell Transplantation
There is still a substantial need to further improve conditioning regimens in SCT through a safe treatment modality. The high relapse rates observed after ASCT suggest that most conditioning regimens are inadequate and more effective options are needed. Radiolabelled immunotherapy, in particular 90Y–ibritumomab tiuxetan, has shown great promise as part of conditioning regimens both as high-dose monotherapy and at standard- and escalated-dose alongside HDC, and appears to offer an effective and well-tolerated alternative to TBI.
Future research to evaluate the role of 90Y–ibritumomab tiuxetan alone with peripheral blood SC support should take a stepwise approach, focusing initially on phase II studies in patients with different histological NHL subtypes. Clear eligibility criteria should be included to define a homogenous population of lymphoma patients and those with a poor prognosis. Research also needs to be carried out with 90Y–ibritumomab tiuxetan as first-line therapy and following relapse. Subsequently, these results can be compared with a standard regimen in historical controls before making the decision to move on to randomised studies in poorprognosis NHL patients. ■
My Learning
Login
Sign Up FREE
Register Register
Login
Trending Topic

12 mins
Trending Topic
Developed by Touch
Mark CompleteCompleted
BookmarkBookmarked
Allan A Lima Pereira, Gabriel Lenz, Tiago Biachi de Castria
NEW
Despite being considered a rare type of malignancy, constituting only 3% of all gastrointestinal cancers, the incidence of biliary tract cancers (BTCs) has been increasing worldwide in recent years, with about 20,000 new cases annually only in the USA.1–3 These cancers arise from the biliary epithelium of the small ducts in the periphery of the liver […]
touchREVIEWS in Oncology & Haematology. 2025;21(1):Online ahead of journal publication