Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin’s lymphoma (NHL), accounting for 30% of all newly diagnosed cases and >80% of aggressive lymphomas.
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin’s lymphoma (NHL), accounting for 30% of all newly diagnosed cases and >80% of aggressive lymphomas.
The cyclophosphamide, doxorubicine, vincristine and prednisone (CHOP) regimen has been the mainstay of therapy for several decades, but a marked improvement in the outcome was demonstrated with the development of the anti-CD20 monoclonal antibody rituximab. Several studies have reported a significant advantage of adding rituximab to CHOP (R-CHOP) in elderly newly diagnosed DLBCL patients and young patients with a favourable prognostic profile.1–3 Although the combination of rituximab with CHOP as the standard regimen has led to improved outcomes, there is a group of poor-risk patients who have a lower chance of being cured with standard R-CHOP and who need alternative treatment strategies.
Prognostic Factors
Clinical and molecular models were devised to better discriminate patients with poor prognosis at presentation.
The International Prognostic Index (IPI) has become the primary clinical tool to predict outcome for patients with aggressive NHL.4 Based on the number of negative prognostic features (>60 years of age, stage III–IV, lactate dehydrogenase (LDH) level, performance status (PS) >1 and more than one extranodal site), four distinct risk groups were identified, with a five-year overall survival (OS) ranging from 26 to 73%. Recently, on the basis that risk assessment is a moving target, a Revised International Prognostic Index (R-IPI) was retrospectively applied to patients with DLBCL treated with R-CHOP, and in so doing distinguished between three separate prognostic groups with different four-year OS rates: very good risk 94%, good risk 79% and poor risk 55%.5
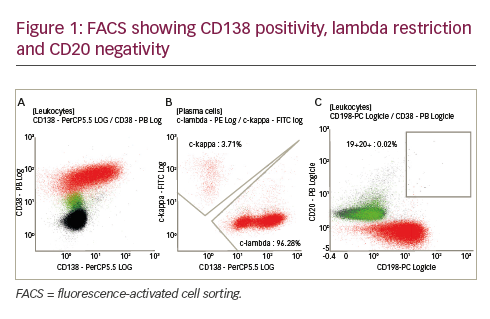
Gene-expression-profiling models defined molecular subgroups of DLBCL, i.e. germinal B cell (GBC) and activated B cell (ABC), with different prognosis: GBC seems to have a more favourable outcome than ABC regardless of rituximab use.6,7 There is clear evidence that DLBCL subtypes are different diseases with distinct oncogenic pathways. Recently, two gene-expression signatures – stromal-1 and stromal-2 – were identified: stromal-1 includes genes that are expressed in fibronectin, suggesting the fibrotic nature of many DLBCLs, while the stromal-2 signature is accompanied by new blood vessel formation and is associated with adverse outcomes (see Figure 1).8
Finally, during the last decade, 18F-2-fluoro-2-deoxy-D-glucose– positron emission tomography (18F-FDG PET) has been shown to be a powerful tool for monitoring response to therapy in most lymphomas and has been introduced into all steps of treatment. Many studies have shown that PET at the end of treatment is highly predictive of progression-free survival (PFS) and OS in aggressive lymphomas with or without residual masses detected with computed tomography (CT) scan. PET scans are able to distinguish between viable lymphoma and necrosis or fibrosis in residual masses. Recently, in a retrospective analysis of 54 patients with NHL, the International Harmonization Project has provided new recommendations for response criteria for aggressive malignant lymphomas, incorporating PET into the definition of response at the end of treatment.9
Some studies have shown that an early PET scan after two to three cycles of chemoimmunotherapy may be predictive of the final response. Haoiun et al.10 prospectively studied 90 patients with aggressive NHL treated with or without rituximab and found higher PFS and OS rates in patients with early negative PET compared with early positive PET (PFS: 82 versus 43%, OS: 90 versus 60%).
However, contradictory results were reported by our group and another that did not show differences in outcome based on early PET results. In fact, the most crucial problem with interim PET analysis in DLBC is its low positive predictive value. Indeed, in another series, positive early PET after two courses of R-CHOP was not predictive, whereas end-of-treatment PET strongly correlated with the outcome.11 However, so far, outside clinical trials, a modification of treatment based on early PET results is not supported by clinical evidence. IPI remains the best tool to separate DLBCL into different prognostic groups and tailor the treatment accordingly.
Treatment
The addition of rituximab to CHOP21 or dose-dense CHOP14 significantly improves the overall and event-free survival (EFS) compared with CHOP alone in both elderly and young low-risk patients with DLBCL. However, patients with poor prognosis still had a chance of cure of ≤45–55%, and these patients should be considered for investigational approaches in the context of clinical trials designed to ensure that potentially curative therapy is not compromised.
Young Patients
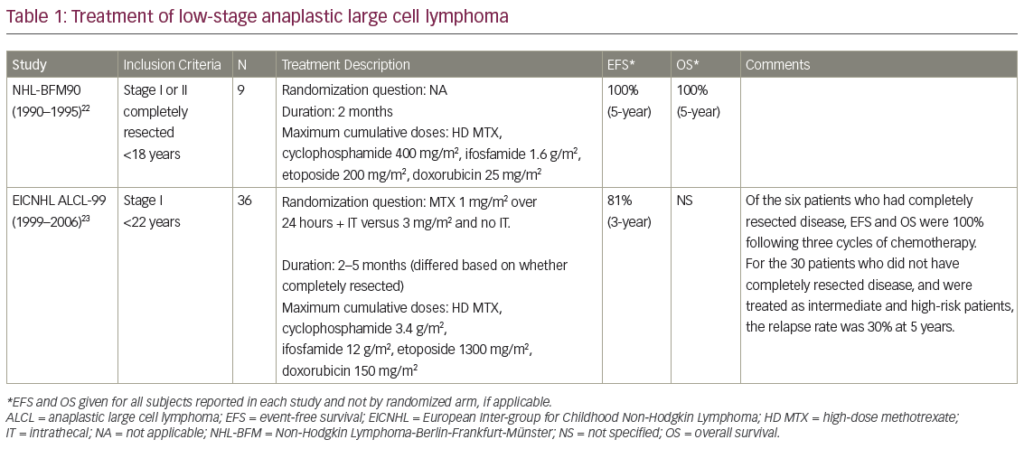
Several phase II non-randomised studies incorporating rituximab into dose-dense or dose-intense schemes, R-CHOP14-like, but without autologous stem-cell transplantation (ASCT) showed that such approaches are feasible and effective in high-risk young DLBCL patients. The estimation of the outcome of young patients with poor prognosis treated with dose-dense or dose-intense schemes, including rituximab, namely R-CHOP14, but without ASCT is difficult; the reported two- or five-year PFS for patients with age-adjusted IPI (aa-IPI) intermediate to high or high-risk score did not exceed 45–61%, therefore indicating that there is a place for new approaches in these patients who are unlikely to be cured by standard R-CHOP.12–14
High-dose chemotherapy (HDC) and ASCT is considered in young patients (<65 years of age) with DLBC without a complete response (CR) after first-line chemotherapy or in patients with chemosensitive DLBCL at relapse. According to guidelines set out by the Italian Society of Haematology and others, this approach to treatment should be considered as first-line in young patients with an intermediate to high or high risk according to the aa-IPI only in approved clinical trials.15 In the pre-rituximab era, conflicting results were generated in randomised studies, with similar survival rates in patients receiving either first-line HDC and ASCT or standard chemotherapy without rituximab.16
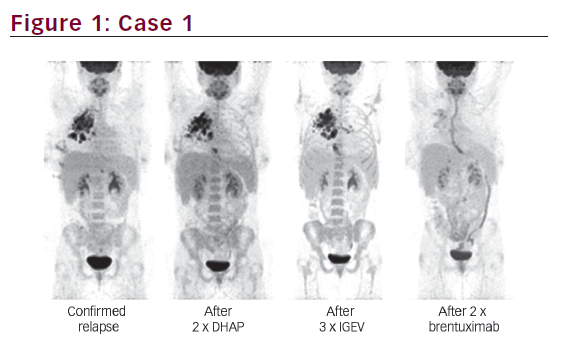
From June 2002 to December 2005, the Gruppo Italiano Multiregionale Linfomi e Leucemie conducted a phase II trial (www.clinicaltrials.gov, NCT00556127) with the aim of exploring the combination of rituximab with dose-dense chemotherapy and HDC with ASCT in 94 untreated young DLBCL patients with a poor prognosis (age-adjusted IPI score 2–3). Briefly, treatment consisted of four courses of a dose-dense R-CHOP-like regimen followed by two courses of HDC with mitoxantrone and high-dose citarabine and ASCT, with carmustine, etoposide, cytosine arabinoside, melphalan (BEAM) as the conditioning regimen. Data were promising: complete remission was obtained in 82% of patients with a four-year failure-free survival (FFS) and OS of 73 and 80%, respectively (see Figure 2).17
On this basis, the cohort treated with rituximab and HDC with ASCT was compared retrospectively with a group of DLBCL patients with the same clinical characteristics treated with a similar approach of HDC, but without rituximab. The significant benefit of adding rituximab was shown in terms of four-year FFS (73% R-HDC versus 44% HDC) and OS (80% R-HDC versus 54% HDC). Recently, similar results were presented in a case–control study comparing dose-dense rituximab–doxorubicin, cyclophosphamide, vindesine, bleomycin, prednisone (R-ACVBP) followed by ASCT versus ACVBP and ASCT; PFS was significantly higher in the R-ACVBP group.18 A summary of the most recent studies in poor-prognosis DLBCL treated with (R) dose-dense chemotherapy with or without R-HDC and ASCT is shown in Table 1.
The question of whether rituximab–HDC may be more effective compared with rituximab–dose-dense chemotherapy is under investigation in randomised phase III trials carried out by the major co-operative groups. A randomised phase II trial by a German group is comparing dose-dense R-doxorubicin, cyclophosphamide, vindesine, bleomycin, prednisone (CHOEP14) with dose-escalated R-CHOEP plus ASCT. The Italian Lymphoma Intergroup (IIL) is currently conducting a randomised trial (IIL-DLCL04) (www.clinicaltrials.gov, NCT00499018) comparing a full course of rituximab–dose-dense chemotherapy (RCHOP14 or R-MegaCHOP14) alone with brief rituximab–dose-dense chemotherapy followed by rituximab–HDC with ASCT in young patients with DLBCL at intermediate to high and high risk (see Figure 3).
Elderly Patients
Two large randomised studies clearly showed that the addition of rituximab to CHOP given every 21 or 14 days significantly improved the outcome of elderly patients (>60 years of age) compared with CHOP or CHOEP but without rituximab. In the Groupe d’Etude des Lymphomes de l’Adulte (GELA) study, patients were randomised to receive eight courses of CHOP with or without rituximab every 21 days.1,26 Rituximab with CHOP21 significantly increased the CR rate (76 versus 63%) and reduced the risk of treatment failure and death (risk ratios 0.58 and 0.64). The superior OS rate of RCHOP was confirmed in both low- and high-risk aaIPI groups. However, the five-year OS rate in high-risk patients did not exceed 50% even in patients treated with RCHOP (R-CHOP versus CHOP: 48 versus 39%), and the five-year EFS in high-risk patients was 41 versus 27% for RCHOP versus CHOP (see Figure 4).
The latter study, conducted by the German High Grade Non-Hodgkin’s Lymphoma Study Group (DSHNHL) (Ricover 60), randomised 1,222 patients to receive six or eight courses of R-CHOP14 with or without rituximab and radiotherapy to sites of initial bulky disease.2 Rituximab–CHOP14 significantly improved EFS, PFS and OS over six cycles of CHOP-14 treatment (three-year R-CHOP14 x 6 versus CHOP14 x 6 EFS 66 versus 47%) (see Figure 5).
A formal demonstration that R-CHOP14 is superior or not to R-CHOP- 21 is lacking. Randomised trials between R-CHOP14 and R-CHOP21 are being undertaken by GELA and the British National Lymphoma Investigation. Therefore, the choice between R-CHOP21 and R-CHOP14, both considered as standard therapy, should be based mainly on the expertise of the centre, performance status of the patients and co-morbidities, favouring the choice of less aggressive treatment (R-CHOP21) in more advanced aged patients. The DSHNHL explored a ‘dense’ R-CHOP14 with an increased dose of rituximab, aimed at improving the efficacy of R-CHOP14 in elderly patients; in fact, the optimal dose of rituximab is not yet well known. In fact, rituximab serum levels build up slowly after infusion and it may also be that dose-dense immunotherapy improves the efficacy of the treatment. Dense-R-CHOP14 explored in elderly patients a supplemented dose-intense rituximab during the first two cycles of R-CHOP14, maintaining a single dose in the subsequent cycles for a total of 12 doses of rituximab delivered in six courses of chemotherapy. The results showed a marked increase in the rituximab serum level and suggested a higher efficacy in poor-risk patients (one-year EFS 74 versus 65%) but also showed an increased incidence of infection, mainly interstitial pneumonia.27 This strategy is currently under investigation in a controlled randomised study.
Novel Approaches
A novel therapeutic option that should be investigated to improve outcome in poor-prognosis DLBCL patients is the addition of radioimmunotherapy. Preliminary data from phase II studies in aggressive lymphomas (DLBCL and mantle cell lymphoma) suggest that 90Y-ibritumomab tiuxetan is also effective in this setting, namely as consolidation treatment after chemoimmunotherapy or as a part of the conditioning regimen before ASCT. Recently, the addition of 90Y-ibritumomab tiuxetan to HDC conditioned with the BEAM regimen was tested in 41 aggressive relapsed/refractory lymphoma patients, including DLBCL, mantle cell lymphoma (MCL) or transformed lymphoma, who were considered poor-prognosis with standard ASCT. The outcome was promising, with a two-year OS and PFS of 88.9 and 69.8%, respectively. Data were encouraging, but larger phase III randomised trials are needed to clarify this matter.28–32
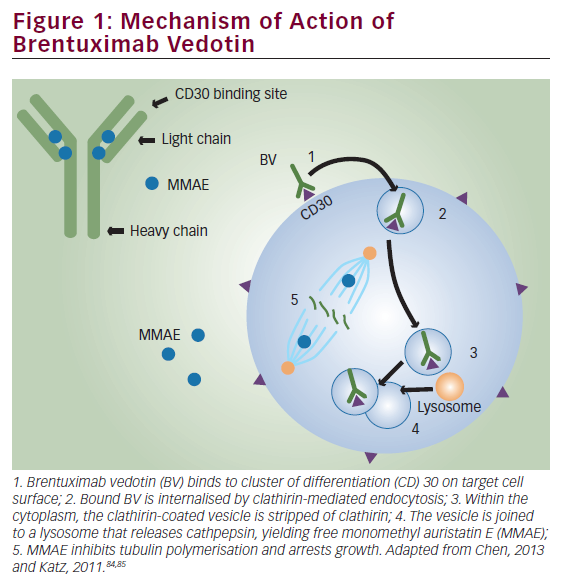
Several novel agents are undergoing evaluation in DLBCL, both as a single agent in the relapsed setting or in combination with standard chemotherapy R-CHOP. These agents have varying degrees of single-agent activity and some of their mechanisms are incompletely understood. These new approaches include immunomodulating agents (IMiDs), dacetuzumab (SGN-40), mammalian target of rapamycin (m-TOR) inihibitors, proteasome inhibitors, histone deacetylase inhibitors and anti-angiogenetic agents (anti-vascular endothelial growth factor [VEGF]).33
IMiDs inhibit angiogenesis and tumour necrosis factor (TNF)- alpha, stimulate immune responses, alter cytokines, inhibit interleukin-12, affect stromal cells, induce apoptosis and inhibit pro-survival factors (Akt). Lenalidomide was tested as a single agent in relapsed or refractory aggressive NHL: the overall response rate (ORR) was 34% for all patients and 24% for DLBCL patients.34 On this basis, the IIL is running a prospective, multicentre, dose-finding phase II pilot trial to evaluate the efficacy and safety of treatment with lenalidomide plus R-CHOP21 (LR-CHOP21) for elderly patients with untreated diffuse large B-cell lymphoma (www.clinical trials.gov, NCT00907348).
The antiapoptotic nuclear factor-kappa B (NFκB) pathway can cause chemoresistance. In ABC DLBCL, the NFκB signalling pathway is constitutively activated and may partially explain the inferior prognosis of this subgroup when treated with doxorubicin-containing chemotherapy. The proteasome inhibitor bortezomib can inhibit NFκB, blocking IkBα degradation. On this basis, Dunleavy et al.35 tested whether bortezomib would enhance the activity of dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide and doxorubicin (DA-EPOCH) in relapsed ABC DLBCL compared with GCB DLBCL. This association demonstrated a significantly higher response (83 versus 13%; p<0.001) and median OS (10.8 versus 3.4 months) in ABC compared with GCB DLBCL. These results provide a rational therapeutic approach to introducing novel agents combined with chemotherapy based on genetically distinct DLBCL subtypes in order to improve the outcome of patients with poor-prognosis DLBCL.35
Bevacizumab (anti-VEGF) was used in aggressive lymphoma as a single agent with poor results; however, its use in combination with standard therapy R-CHOP was promising. In a pilot trial on 13 untreated DLBCL patients, the association of bevacizumab, rituximab and CHOP (RA-CHOP) demonstrated 85% ORR and a 12-month PFS of 77%.36,37 An international phase III double-blindied study (RA-CHOP versus R-CHOP) is ongoing (www.clinicaltrials.gov, NCT00486759).
Conclusions
R-CHOP21 and/or R-CHOP14 are the standard of care for DLBCL. However, the identification of poor-prognosis patients is a priority because these patients have ≤50% chance of cure with R-CHOP. Various therapeutic options have been evaluated to improve the outcome of these patients. These include R-HDC + ASCT as the first-line treatment, increased administration of rituximab in the first courses of R-CHOP (dense-R-CHOP14) and the addition of novel agents to standard R-CHOP or their use as single agents. The enrolment of such patients into clinical trials aimed to test these therapeutic strategies is warranted to improve their outcome. ■