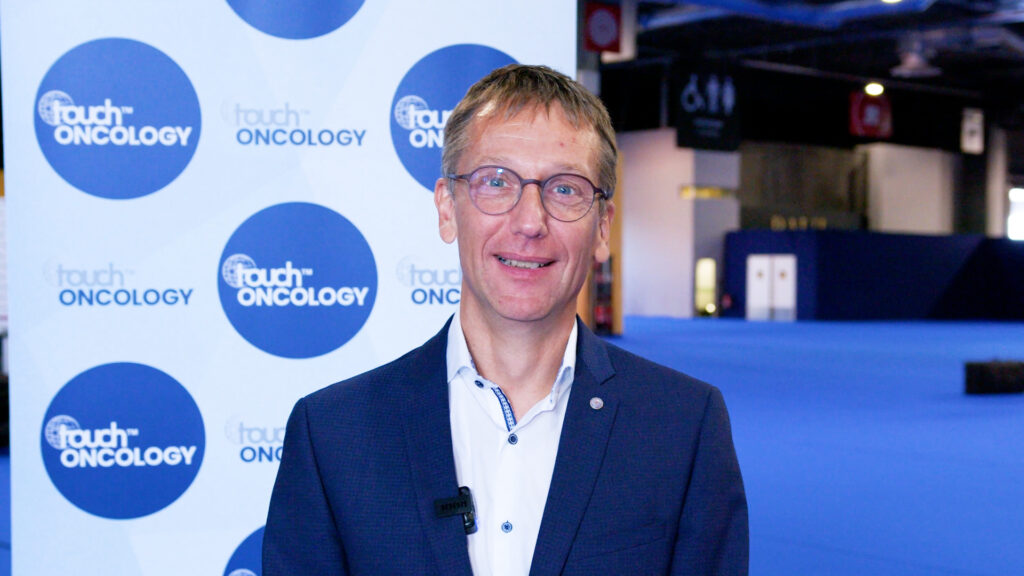
“The patient always comes first – that lesson guides every decision I make”
 Dr Ari Rosenberg (University of Chicago Medicine, Chicago, IL, USA) specializes in the treatment of head and neck cancer, salivary gland cancer and thyroid cancer. His particular academic interest is in developing novel therapeutic strategies for patients with these diseases. As a clinical investigator, he develops and conducts clinical trials for patients while incorporating novel tissue and blood-based biomarkers. He has a particular focus on incorporating novel therapies and immunotherapeutic strategies, as well as developing multimodality treatment paradigms to reduce treatment-related toxicity and improve long-term function and quality of life.
Dr Ari Rosenberg (University of Chicago Medicine, Chicago, IL, USA) specializes in the treatment of head and neck cancer, salivary gland cancer and thyroid cancer. His particular academic interest is in developing novel therapeutic strategies for patients with these diseases. As a clinical investigator, he develops and conducts clinical trials for patients while incorporating novel tissue and blood-based biomarkers. He has a particular focus on incorporating novel therapies and immunotherapeutic strategies, as well as developing multimodality treatment paradigms to reduce treatment-related toxicity and improve long-term function and quality of life.
In this interview, Dr Rosenberg shares his journey into oncology, the pivotal moments that shaped his approach to patient care and the exciting advancements transforming treatment strategies. From a life-changing decision that preserved a patient’s ability to speak, to the promising future of immunotherapy and targeted therapies, this conversation provides valuable insight into the compassionate and innovative world of head and neck cancer treatment.
Q. Is there a particular moment or experience that inspired and/or reinforced your passion for your specialty?
One patient that comes to mind was a middle-aged woman who came to our team with a diagnosis of a stage 4 tongue cancer that had spread to multiple lymph nodes in her neck. She told me that she noticed every time she took a sip of her morning coffee there was a burning sensation in her mouth. She came to us after a surgeon at another hospital had recommended cutting out more than half of her tongue, which would have greatly impacted her ability to speak and swallow from the surgery. She told me that she was inspired by the story of Grant Achatz, a world-renowned chef and the owner of a Michelin-starred Chicago restaurant called Alinea. He was treated by my colleagues at UChicago Medicine on a clinical trial with non-surgical treatment while preserving his tongue. Ultimately, after discussing with our group including the head and neck surgeon, the decision was made that a non-surgical treatment approach would be a good option for her unique case. Today, when I see her for her for follow-up in clinic and she expresses her gratitude for her ability to speak, eat and drink while being cancer free, I am incredibly inspired and reinforced to continue the work.
Q. What is the most valuable lesson a mentor has shared with you, and how has it influenced your work?
I feel greatly indebted to my mentors over the course of my training and medical journey who have inspired and provided invaluable lessons that have moulded my career trajectory. One of the most valuable lessons that I received from Dr Everett Vokes, a world-renowned medical oncologist and international leader in both head and neck and lung cancers, is to remember that the patient always comes first. I keep this in mind every time I am in clinic taking care of patients, recommending a particular clinical trial, or even deciding on the next research question to test – the patient remains at the focal point. Dr. Vokes is not only a prolific researcher and leader within oncology, he is an incredible clinician taking care of each individual patient as if it was his own family member. In a similar way, I strive to always have the patient at the center of everything I do and keep this in mind at all times.
Q. What current development or trend in your specialty excites you the most?
This is a very exciting time with many new innovations and discoveries emerging within the field of head and neck cancer. Over the past decade, the incorporation of immunotherapy into the treatment paradigm for patients with recurrent or metastatic head and neck cancer has improved survival, yet despite this progress there remains a substantial unmet need. Recently, new treatment options have been emerging as quite promising within the field. We have seen the development of bispecific antibodies, which can simultaneously target two distinct targets on either cancer cells or immune cells, with early data looking quite promising. Additionally, we have seen the emergence of antibody-drug conjugates in the treatment of head and neck cancer, which are medications that can both target while also delivering a chemotherapy directly to the cancer cell. We have also seen new medications such a pill forms of targeted therapies (multitargeted kinase inhibitors) that are able to alter the microenvironment (cells and architecture around the cancer cells) to make it easier for immunotherapy to drive the immune cells to eliminate cancer cells. Finally, the discovery of blood-tests that can measure tumor DNA in blood has much potential to better assess how well a particular treatment is working, to adapt and personalize treatment, and even to identify recurrence earlier in a patient’s treatment trajectory. While it is still early, these are very exciting developments that I sincerely hope will lead to improvements in outcomes for patients with head and neck cancer.
SIGN UP to touchONCOLOGY!
Join our global community today for access to thousands of peer-reviewed articles, expert insights, and learn-on-the-go education across 150+ specialties, plus concise email updates and newsletters so you never miss out.