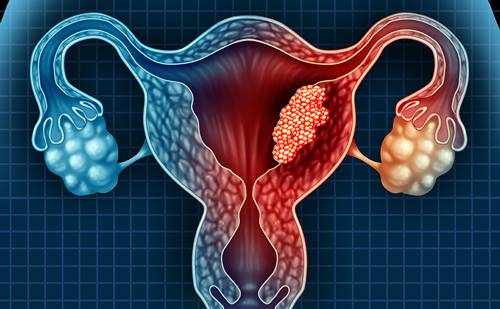
Endometrial Carcinoma
Endometrial cancer is the most common gynecologic malignancy in developed countries.1 According to Surveillance, Epidemiology and End Results (SEER) statistics the estimated incidence of cancers of the uterine corpus for US women in 2013 is 49,560, with an estimated 8,190 deaths. Median survival for women with recurrent or metastatic disease is only 12 to 15 months. The most commonly used systemic treatment for advanced disease at this time is platinum/taxane-based chemotherapy, which has produced higher response rates and longer median progression-free survivals than hormonal therapy, but progestins remain useful, and occasionally produce prolonged disease control. Mammalian target of rapamycin (mTOR) inhibitors have also recently been shown to have modest single-agent activity.
Type I and Type II Endometrial Carcinoma
Endometrial cancers are often divided into two conceptual categories: type I and type II.2 About 80 % of endometrial carcinomas are type I, i.e. of endometrioid histology with low or intermediate grade. These cancers can arise in the setting of persistent unopposed estrogen stimulation, and tend to occur in perimenopausal women.3 They are generally preceded by endometrial hyperplasia and are usually estrogen- and progesterone- receptor (ER/PR) positive. Molecular alterations associated with type I tumors include deletions/inactivating mutations of the PTEN tumor suppressor gene (36–83 %), microsatellite instability (20–40 %), mutations of K-ras (15–30 %), and gain of function mutations in β-catenin (25–40 %).4–6 By contrast, type II tumors are histologically nonendometrioid e.g. serous or clear cell, and have no association with excess endogenous or exogenous estrogen. They tend to occur in older women, and are aggressive with a proclivity for lymphovascular invasion, distant spread, and deep tissue invasion; they account for nearly half of endometrial cancer deaths.7 The genetic alterations associated with type II tumors include aneuploidy, p53 mutations (80–90 %), p16 inactivation (40 %), overexpression of human epidermal growth factor receptor 2 (HER-2)/neu (40–80 %), and E-cadherin alterations (80–90 %).4–6 Mutations in PIK3CA (gene encoding the catalytic subunit of PI3K) and PIK3R (which encodes the regulatory subunit of PI3K) can occur in both subtypes, although they appear to be more common in type I cancers.8,9 Increased signaling of the PI3K/AKT/mTOR pathway is associated with a poor prognosis in both type I and type II carcinomas.10
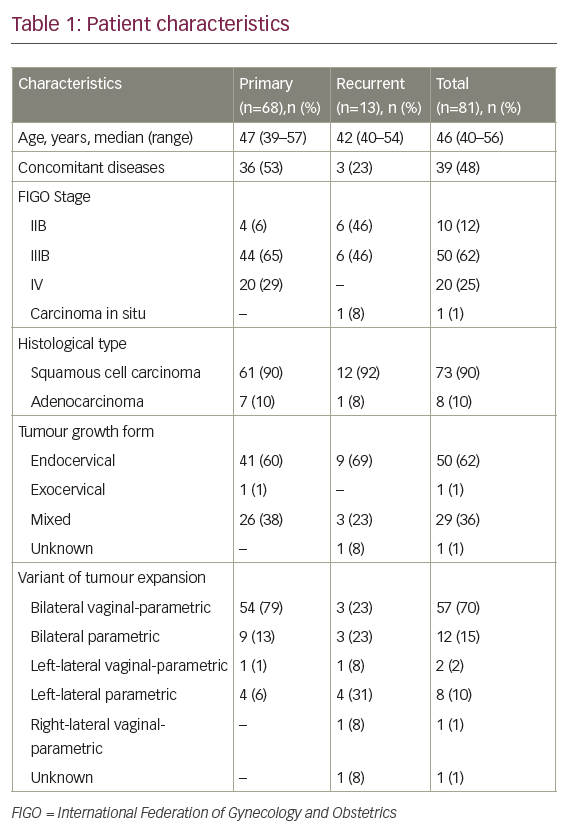
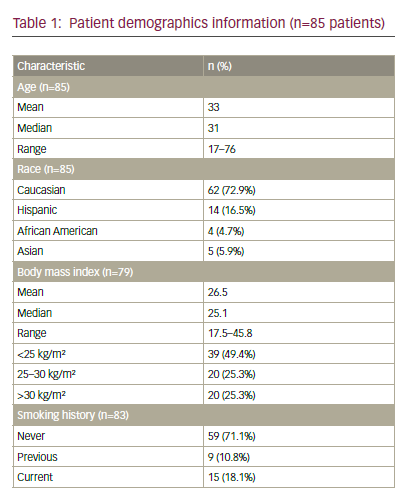
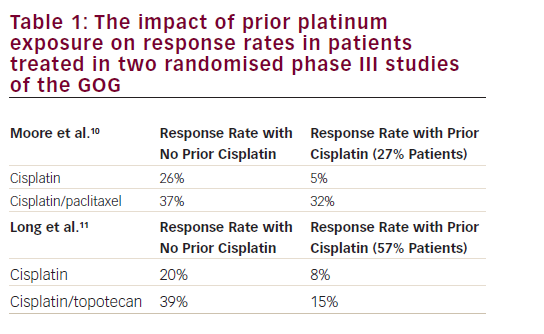
Hormone Therapy in the Treatment of Advanced Endometrial Cancer (see Table 1,)
Since the early studies by Kelly and Baker in 1965, progestin-based therapy has played a role in the treatment of advanced endometrial carcinoma.11,12 Trials in chemotherapy-naïve advanced endometrial carcinoma patients have demonstrated response rates of 18–34 % to progestins with median overall survivals of 6–14 months.13 Commonly used regimens in the US include megestrol acetate (MA) 160 mg/day, or MA for 3 weeks alternating with tamoxifen (TAM) for 3 weeks. The addition of TAM was hypothesized to increase the percentage of endometrial cells that contain PRs, as well as the concentration of surface receptors.14 While this alternating regimen has not been compared with single-agent megestrol therapy in a randomized trial, the 27 % response rate reported is as high as or higher than that reported with any other hormonal regimen, and TAM causes less weight gain than MA. Dose escalations of MA to 1,000 mg/day did not improve overall survival or progression-free survival.15 In general, the highest response rates are found in patients with well-differentiated hormone receptor positive tumors.11 However, objective response rates as high as 17 % have reported in PR-negative tumors, making ER/PR expression an inadequate predictor of benefit from hormone therapy in clinical practice. This may be partly related to heterogeneity of receptor distribution within an individual tumour. The most common side effects of progestin-based therapy are weight gain in about 26 % and venous thrombosis in about 5 % of patients;16 edema can also occur. Selective estrogen modulators, such as TAM or arzoxifene, have also produced modest response rates, although lower than those seen with progestins.13 Aromatase inhibitors including letrozole and anastrozole have shown response rates of less than 10 %.17–19 Of note, patients on the trials of aromatase inhibitors were permitted to have had prior hormonal therapy, although not prior chemotherapy. A small multicentre phase II study of the National Cancer Institute of Canada (NCIC) Clinical Trials Group testing the use of letrozole found a 9.4 % response rate and no correlation between response and expression of the following biomarkers: PR (86 %), ER (86 %), PTEN (82 %), phosphorylated PKB/Akt (59 %), bcl-2 (49 %), p53 (32 %), and HER-2 (0 %).
mTOR Inhibitor Therapy in Endometrial Cancer
The mTOR is a protein downstream of PI3 Kinase that is activated by oncogenic alterations of the pathway. mTOR regulates numerous cell functions, including protein translation, cell growth, and apoptosis. There are two mTOR complexes, mTORC1 and mTORC2, both of which have downstream effects.20 The rapamycin-analog mTOR inhibitors currently available (temsirolimus, everolimus, and ridaforolimus) all act via binding to the cytosolic protein, FK binding-protein 12 (FKBP12), and primarily inhibit mTORC1. As early in vitro work suggested that genetic abnormalities resulting in activation of the PI3K/AKT/mTOR pathway, including loss of PTEN function, were associated with anti-tumor efficacy of mTOR inhibitors, these agents were tested fairly early in endometrial cancer. Bae-Jump et al. demonstrated in vitro activity of rapamycin in both type I and type II endometrial cancer tumor explants21 and, indeed, clinical responses have been observed in both type I and type II endometrial cancers.
The NCIC Clinical Trials Group performed two phase II studies evaluating single-agent temsirolimus, the first in women with recurrent or metastatic chemotherapy-naïve disease, and the second in women who had prior chemotherapy. Temsirolimus 25 mg intravenously (IV) was administered weekly. In the chemotherapy-naïve group, four of 29 evaluable patients (14 %) had a partial response with a median response duration of 5.1 months and 20 (69 %) had stable disease with a median duration of 9.7 months. In the group with prior chemotherapy, only one of 25 evaluable patients (4 %) responded; 12 patients (48 %) had stable disease with a median duration of 3.7 months.22 Neither absence of PTEN by immunohistochemical staining, PTEN mutation, nor molecular markers of PI3K/Akt/mTOR pathway correlated with clinical outcomes.23 Toxicities were typical of those seen with mTOR-inhibitor therapy, and included fatigue, rash, nausea, diarrhea, mucositis, and pneumonitis. Asymptomatic pneumonitis was particularly common in this study (42 %) with five patients (8 %) having grade 3 pneumonitis. Low levels of activity were also seen in phase II trials of ridaforolimus and everolimus in women with pretreated disease (see Table 2).
More recently, a randomized phase II trial compared ridaforolimus with progestin-based therapy and standard chemotherapy in 130 women with advanced disease who had received one or two prior chemotherapy regimens. Almost one-third of patients had tumors of serous histology, and more than 50 % had grade 3 tumors. Ridaforolimus met the primary endpoint of the study by demonstrating a progression-free survival of 3.6 versus 1.9 months with progestins.24 Toxicities with ridaforolimus included hyperglycemia, fatigue, diarrhea, anemia, and mucositis, but no grade 3 pneumonitis.25Given the toxicities with mTOR-inhibitor therapy, a biologic indicator of which patients are most likely to benefit, but no good predictive marker has emerged to date.
Rationale for Combination of mTOR Inhibitors with Hormone Therapy
The PI3K/AKT/mTOR signaling cascade has been widely implicated in resistance to chemotherapy agents, molecularly targeted agents, such as trastuzumab or gefitinib, radiotherapy, and hormonal therapy.26–28 In breast cancer, clinical data have begun to suggest that use of mTOR- inhibitor therapy can overcome acquired resistance to trastuzumab and to aromatase-inhibitor therapy. A phase I/II study reported a 15 % response rate and a 34 % clinical benefit rate with the combination of trastuzumab plus everolimus in women with HER2-positive tumors that had progressed on trastuzumab therapy.29 More definitive evidence is in the setting of the combination of an mTOR inhibitor with hormonal therapy. A randomized, double-blind, placebo-controlled phase III clinical trial (BOLERO-2) randomly assigned 724 hormone-receptor positive advanced breast cancer patients who had recurrence or progression on a nonsteroidal aromatase inhibitor to exemestane (a steroidal aromatase inhibitor) plus everolimus or placebo. The combination therapy showed a superior progression-free survival of 10.6 months versus 4.1 months with exemestane alone.30 The most common grade 3 or 4 adverse events with the combination were stomatitis, anemia, dyspnea, hyperglycemia, fatigue, and pneumonitis (3 %).
Specifically in endometrial cancer, there are in vitro data that mTOR inhibitors increase progesterone messenger RNA (mRNA) expression.21,31 In addition, in vitro and in vivo xenograft mouse models suggest that MPA activates the PI3K/AKT pathway in progestin-resistant cells, and that inhibiting this pathway reverses progestin resistance in these cell lines.32 Two phase II trials combining mTOR inhibitors with hormonal therapy have been completed in endometrial cancer, and both have been reported in abstract form (see Table 2). The Gynecologic Oncology Group (GOG) has completed GOG-0248, a randomized phase II trial in women with hormone therapy-naïve disease; one prior chemotherapy regimen was permitted (in the setting of stage I, II, or III disease, or as radiation sensitizer for pelvic recurrence, or in setting of stage IV disease if patient was without evidence of disease at end of chemotherapy and at least 6 months elapsed prior to progression). Patients received either single-agent temsirolimus 25 mg IV weekly and or the temsirolimus given concomitantly with MA 80 mg bid for 3 weeks alternating with TAM 20 mg bid for 3 weeks. Unfortunately, the arm with the combined regimen closed after the first stage due to an unacceptable rate of venous thrombosis (seven events in 22 patients).34,35 Three of 21 patients (14 %) had a partial response at the time of the preliminary report. Results for the single agent are pending. A two-institution, open-label, singlearm phase II study in patients with recurrent endometrial cancer who had received two or fewer prior chemotherapeutic regimens received the combination of letrozole 2.5 mg daily and everolimus 10 mg daily. Four of 19 patients (21 %) had an objective response and eight of 19 (42 %) had clinical benefit, defined as complete response (CR), partial response (PR), or stable disease (SD) for at least 8 weeks. This response rate appears better than the historic controls with hormone therapy in a chemotherapy pretreated population, as well as being better than results obtained by the same authors in a single-agent trial of everolimus in a similarly pretreated population (no objective responses), although the rate of stable disease at 8 weeks (43 %) was similar. The most common drug toxicities were fatigue, stomatitis, hypertriglyceridemia, nausea, and hyperglycemia.33 Given that response rates of over 10 % with any agent in the setting of chemotherapy pretreated endometrial cancer are unusual, further development of hormone therapy and PI3K pathway inhibitor combinations is clearly warranted.
Other Potential Combinations with mTOR Inhibitors in Endometrial Carcinoma
As described above, activation of the PI3K/AKT/mTOR pathway has been implicated as a mechanism of resistance to both trastuzumab and standard cytotoxic chemotherapy, and combining trastuzumab or chemotherapeutic agents with inhibitors of the pathway has overcome resistance in numerous reports.36,37 Trials combining chemotherapy with mTOR inhibitors have been slow to emerge, in part because the toxicities of the combinations are not always easy to manage.38 However Kollmannsberger et al. successfully developed a regimen combining carboplatin/paclitaxel with temsirolimus on a 2 out of 3-week schedule39 and a trial testing this regimen in the GOG has been completed; results should be available soon. Another opportunity might be combinations with trastuzumab. Endometrial carcinomas can both overexpress and amplify HER2; a phase II GOG trial of single-agent trastuzumab in HER2-positive endometrial cancer found an overall rate of 11.5 % amplification, with highest rates of amplifications in serous carcinomas (seven of 25; 25 %), clear cell carcinomas (three of eight; 38 %), and mixed carcinomas (three of 11, 27 %). The trial, which permitted unlimited prior chemotherapy regimens, reported no objective responses.
However, given the preclinical data suggesting that PI3K/AKT pathway activation is associated with resistance to trastuzumab, and the encouraging clinical results of the everolimus/trastuzumab combination in breast cancer (described above), trials testing a similar combination in endometrial cancer are of interest.