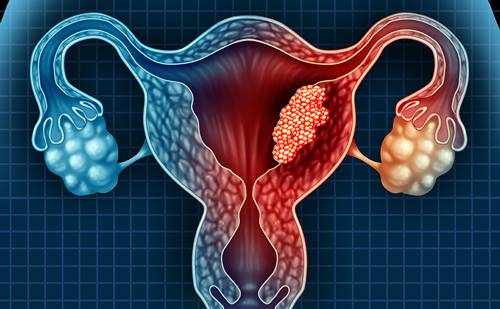
Every year nearly 55,000 people are diagnosed with invasive and in situ breast cancer in the UK:1 around 5,600 are younger women, aged 45 and under.
This group of women have specific information needs and to address this Breast Cancer Care has developed Standards of Care for Younger Women.2
To prioritise these standards, Breast Cancer Care undertook two surveys: with younger women themselves and with healthcare professionals (HCP). The most startling finding was that the majority (88 %) of younger women reported not ever having been offered a fertility referral to discuss the options of fertility preservation.
There were 176 survey responses from younger women with breast cancer and 50 from breast cancer oncologists, surgeons and nurses. Over a third (35 %) of HCP respondents reported not telling younger breast cancer patients at diagnosis how treatment could affect their fertility, leaving the women completely unaware of the risks. Around a third (30 %) of HCPs said they did not discuss fertility options with younger women with breast cancer sufficiently well to enable the women to make informed decisions about their future fertility. Around a quarter (26 %) reported that they did not have a clear system set up to direct patients to fertility clinics promptly. ‘(Fertility) not discussed routinely. Referral pathway for advice not always clear’ (response from an Oncologist involved in the survey).
This is despite recommendations in place since 2011 from the Royal College of Obstetricians and Gynaecologists that, ‘Every breast oncology service should have a designated pathway for prompt referral to a fertility specialist able to offer assisted conception; service provision should not be dependent on local in vitro fertilisation funding arrangements.’3
The latest National Institute for Health and Care Excellence guideline for fertility says the effect of cancer and its treatments on fertility should be discussed at initial diagnosis.4 Egg and embryo cryopreservation should be offered to young women diagnosed with cancer if they are well enough, there is enough time available and it will not worsen their condition.
Fertility preservation today for a woman with breast cancer can involve egg, embryo or tissue freezing. There is also the option of using a gonadotropin-releasing hormone (GnRH) analogue during chemotherapy and current testing of the ovarian reserve: antimullerian hormone (AMH) or ultrasound of the ovaries. For many women a discussion is all that is needed. Then they are in a position to make an informed choice about their future fertility.
‘Although I did not take the option to freeze my embryos, it gave me greater choice and also having been checked out by the specialist, knowing my ovaries were working fine at that time helped me decide which treatment/help to accept’ (response from a young woman involved in the survey).
A breast cancer diagnosis at a young age can have devastating effects. As Victoria, 36, put it when talking about her own diagnosis: ‘A breast cancer diagnosis as a younger woman hits you at the most productive time of your life, when relationships are still to be formed or are in their early years, when families are being created or are young, careers are in full throttle and life is being lived. Suddenly, you are knocked on to a different track and you are alone, you become very, very isolated.’
At Breast Cancer Care’s Younger Women Together events we bring together younger women with breast cancer to gain information and support that addresses their unique needs, share experiences and reduce their sense of isolation. HCPs run information sessions at the events. Often it is the first time the young women have met someone of a similar age having treatment for breast cancer. We sometimes hear from younger women at these events that they did not receive any information about the possibility of treatment affecting their fertility. ‘There was no talk about fertility at all.’ Realistic expectations must be maintained, and the importance of accurate and honest counselling cannot be underestimated. This will include the chances of success from fertility treatment and the possible impact of delaying breast cancer treatment.
But which HCP is best placed to discuss fertility options? Fertility preservation is not always appropriate, but young women deserve to have this discussion with fertility specialists, particularly as oncofertility is an area that is advancing quickly. For instance, the induction of random start stimulation protocols and the use of aromatase inhibitors.
Breast Cancer Care’s Younger Women Champions – breast care nurses from across the UK – are working on fertility pathways and a referral toolkit to facilitate the smooth and timely referral between breast oncology and fertility specialists.
And Breast Cancer Care is campaigning for all younger women to be offered referral to a fertility expert at diagnosis, ensuring they can make informed choices about their future fertility. Visit www.breastcancercare. org.uk/hiddeneffects to join the campaign.