Melanoma is the fifth leading cancer in men and the seventh in women. The incidence is increasing and it is estimated that in 2012 76,250 people in the US were diagnosed with melanoma of the skin and 9,180 died of the disease.1The majority of patients are cured following primary resection of the tumor; however, in approximately 16 % of cases, the disease will ultimately metastasize.2 Melanoma has a propensity for hematogenous and lymphatic dissemination to regional and distant sites and has a low response rate (RR) to most systemic therapies.3 The five-year survival rate for metastatic melanoma is poor, ranging from 5 % to 10 %4 with a median survival of 8 to 9 months.5 however, recent advances in immunotherapy and targeted therapy have translated into improved survival rates up to a median of 10–13 months.6,7
Approved Therapies
There are currently four US Food and Drug Administration (FDA)-approved treatments for metastatic melanoma: intravenous bolus high-dose interleukin-2 (hD IL-2), dacarbazine (DTIC), ipilimumab, and vemurafenib.
DTIC was the first FDA-approved treatment and was considered the standard first-line therapy for patients with metastatic disease treatment prior to the emergence of ipilimumab and vemurafenib. DTIC is a cytotoxic alkylating agent and is associated with RRs of 5–15 %, with median response duration of 4–8 months,8 a progression-free survival (PFS) of 1.5–3 months and limited overall survival (oS). To date, no clinical trials with DTIC or other chemotherapies have been reported to improve the oS of patients with metastatic melanoma. Although not approved for use in melanoma by the FDA, the oral prodrug temozolomide yields the same active intermediate (3-methyl-[triazen-1-yl]imidazole-4-carboxamide) as DTIC, is able to cross the blood–brain barrier, and has similar activity to DTIC. It is often used as an alternative to DTIC. A randomized phase III study of temozolomide versus DTIC for patients with advanced melanoma demonstrated that these agents have equal efficacy. The median oS was 7.7 months for patients treated with temozolomide and 6.4 months for those treated with DTIC.9
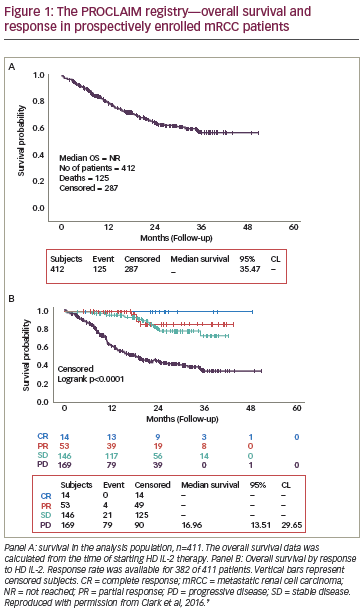
Immunotherapy with hD IL-2, a type 1 cytokine, at a dose of 600,000– 720,000 IU given to tolerance every 8 hours for up to 5 days is associated with an overall RR of approximately 16 %, with around 6 % of patients achieving durable complete responses (CRs)10 Although this therapy can be associated with significant toxicities including hypotension, pulmonary edema, renal failure, and mental status changes, these side effects are transient and can be safely managed by experienced clinicians. A recent retrospective study suggested that patients with an elevated lactate dehydrogenase (LDh) may be less likely to derive benefit from hD IL-2 and those with nRAS mutations were more likely to derive benefit.11 In summary, hD IL-2 should be considered only for select patients with a good performance status.12
In 2011, the FDA approved two further therapies for the treatment of metastatic melanoma—ipilimumab and vemurafenib. Ipilimumab is a fully human immunoglobulin g1 (Igg1) monoclonal antibody that blocks cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4), a T-cell immunosuppressive receptor.13 In a phase III study comparing ipilimumab with or without glycoprotein 100 (gp100) peptide vaccine, to gp100 vaccine alone, reported an overall RR (oRR) of 10.9 % to ipilimumab and a median oS of 10.1 months.7 In a phase III trial of ipilimumab in treatment-naive patients with metastatic melanoma, ipilimumab plus DTIC demonstrated improvement in oS versus single agent DTIC (11.2 versus 9.2 months, respectively).14 There was a near doubling of oS at the two- and three- year time points in patients treated with ipilimumab compared with the control group.
The second drug approved in 2011 was the B-Raf (BRAF) v600E kinase- inhibitor vemurafenib. Approximately 40 % to 50 % of melanomas carry an activating mutation in the BRAF gene, and of these mutations 90 % result in the substitution of glutamic acid for valine at codon 600 (BRAF v600E).15 The use of vermurafenib is limited to patients with a demonstrated BRAF v600E mutation. In a phase III trial, vemurafenib was superior to DTIC in terms of RR, PFS and oS benefit.6 While the objective RR of vemurafenib is nearly 50 % and ~90 % of patients experience some degree of tumor regression, the median duration of response is only ~6 months15 with resistance occurring in virtually all patients.
Surgical Resection for Cure
The role for surgical excision of all known metastatic disease in patients with stage Iv melanoma is the subject of debate. The high likelihood that individuals with advanced melanoma have widespread yet undetected disease, combined with a lack of well-controlled trials demonstrating increased survival from metastasectomy, makes many clinicians reluctant to recommend surgery to asymptomatic patients. Patients with solitary brain metastasis represent a notable exception. Controlled randomized trials have demonstrated that individuals with solitary brain metastasis have improved survival and quality of life when they receive resection plus radiotherapy.16 Data to support resection of metastatic melanoma for curative intent at sites other than brain is limited to retrospective series, largely produced by single institutions. Multiple retrospective series suggest that patients with pulmonary metastasis benefit from resection and have 5-year survival rates of over 20 %.17,18 Stage Iv patients with disease limited to skin, subcutaneous sites and nodes also appear to benefit from resection. Survival differences have been reported in selected patients undergoing surgery for metastatic melanoma at various sites compared with historic controls. There is strong evidence to suggest that patients with a solitary site of disease have a better prognosis following surgery that individuals with multiple sites of disease.19 Patients who achieve a response to immunotherapy may also benefit from resection.20 Combination Therapy
Immunotherapy Combinations
Currently, hD IL-2 and ipilimumab are the only two approved immunotherapy options for the treatment of metastatic melanoma. A phase I study evaluating treatment with hD IL-2 and escalating doses of ipilimumab (at 0.1, 0.3, 1, 2, and 3 mg/kg) reported that the combination of ipilimumab and IL-2 had an oRR of 22 % in the 36 patients treated.21 The long-term follow-up data of this study was recently published: with a median followup of 84 months, the median survival was 16 months and the overall CR rate was 17 % in this cohort of patients.22 A randomized trial comparing ipilimumab alone versus ipilimumab plus hD IL-2 was recommended.
Various vaccination strategies to induce active immunity targeting melanoma cells are currently being tested and include vaccination with peptides, nucleic acids, dendritic cells, and heat shock protein complexes. Results of studies using a combination of immunotherapy and vaccination have been varied. In a randomized phase III trial, the addition of gp100 vaccine to hD IL-2 demonstrated an improved objective RR (16 % versus 6 %; p=0.03) and oS (17.8 versus 11.1 months; p=0.06).23 A phase III trial, in which patients were randomly assigned to receive ipilimumab plus gp100, ipilimumab alone, or gp100 alone, found that the efficacy of ipilimumab was not improved by the addition of gp100.7 A recent phase II trial failed to demonstrate that allogeneic large multivalent immunogen (LMI) vaccine and low-dose IL-2 improved survival in patients with melanoma compared with low-dose IL-2 alone.24
Biochemotherapy
The term biochemotherapy refers to treatment regimens that combine cytotoxic agents such as DITC with immunotherapy agents such as IL- 2, interferon (IFn)-alpha or ipilimumab. Although results from early trials of biochemotherapy using IFn-alpha and/or IL-2 suggested a benefit in patients with metastatic disease25,26 those benefits have not been confirmed in large-scale, multicenter, phase III trials.27,28 A 2007 metaanalysis of 18 biochemotherapy randomized clinical trials found that although biochemotherapy clearly improved RRs, no survival benefit was noted and biochemotherapy was associated with increased hematologic toxicity.29 Similarly, a 2007 Cochrane review failed to find any clear evidence that the addition of immunotherapy to chemotherapy increases survival of people with metastatic melanoma.30 A 2008 systematic review noted that RRs to biochemotherapy were superior to chemotherapy; however, there was little benefit in time-to-progression, and survival.31 A systematic review on the effects of chemotherapy and immunotherapy on metastatic melanoma concluded that immunotherapy was unlikely to increase survival when added to chemotherapy.32
Several research groups have investigated, or are currently investigating, the efficacy of biochemotherapy combinations containing ipilimumab. In a randomized phase II study of ipilimumab versus ipilimumab and DTIC, the ipilimumab/DTIC combination resulted in an increased oRR (14.3 % versus 5.4 % for ipilimumab monotherapy) and improved one-, two-, and three-year survival.33 Similarly, in a phase III randomized trial, ipilimumab in combination with DTIC was reported to increase median oS compared with DTIC alone (11.2 versus 9.1 months).14 Preliminary results from a single-arm phase II study found that the combination of ipilimumab and temozolamide achieved overall disease control (CR/partial response [PR], and stable disease [SD]) of 67 %.34 The combination of ipilimumab and bevacizumab in a phase I trial resulted in a RR of 36 % and achieved overall disease control in 67 %; however, immune-related adverse reactions were increased using this combination.35 Finally, a phase II study combining ipilimumab with fotemustine demonstrated a RR of around 30 %, and achieved disease control in 47 %, including activity in patients with brain metastases.36
Targeted Therapies
Currently, the only FDA-approved targeted therapy for use in metastatic melanoma is the BRAF inhibitor vemurafenib. however, resistance to BRAF inhibitors develops within 6–7 months following initiation of treatment and the duration of response is limited. Determining the factors that promote resistance to BRAF inhibitors is currently a topic of intensive research. Combination therapy that simultaneously inhibits different pathways may prove effective in increasing the duration of response to BRAF inhibitors and warrants further investigation. Preclinical data suggests that BRAF inhibitors in combination with mitogen-activated protein kinase (MEK) inhibitors or P13/mammalian target of rapamycin (mToR) inhibitors may have great potential as combination therapy.37 A phase I/II study is currently ongoing to test the safety and efficacy of combining vemurafenib with the PI3K inhibitor, BKM120.
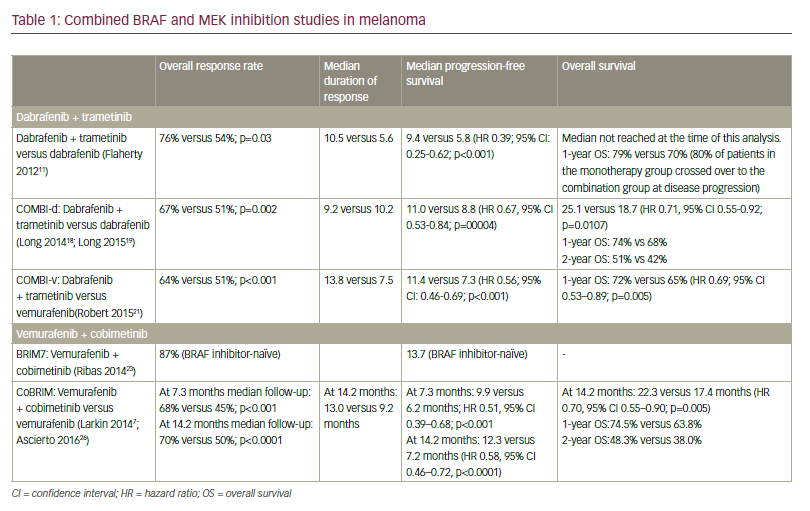
Dabrafenib is a selective BRAF inhibitor that does not have FDA approval, but has demonstrated improved oS compared with DTIC in phase III trials as a treatment for metastatic melanoma.38 A recent phase I/II trial of combined treatment with dabrafenib (a selective BRAF inhibitor), and trametinib (a selective MEK inhibitor) reported a CR/PR with combination therapy of 76 %, compared with 54 % with dabrafenib monotherapy.39 After one year of treatment, 41 % of those receiving full-dose combination treatment had no progression of their cancer, compared with only 9 % of those receiving one drug, and the median PFS in the combination group was 9.4 months, compared with 5.8 months in the monotherapy group. While combinational therapy delayed the onset of drug resistance, it did not prevent resistance in the majority of participants. Phase III testing of this drug combination is currently ongoing. In addition to BRAF inhibitors, other combinations of targeted therapies are being explored to treat metastatic melanoma; however, clinical data to date does not support the efficacy of these regimes. A recent study on the efficacy and toxicity of everolimus (an mToR inhibitor) in combination with paclitaxel/carboplatin in patients with advanced melanoma found that the combination was well tolerated; however, efficacy data were similar to that reported with paclitaxel/ carboplatin alone.40 Similarly, a recent phase III trial of the tyrosine protein kinase inhibitor sorafenib found that there was no improvement in oS when sorafenib was given in combination with paclitaxel/carboplatin for chemotherapy-naive patients with metastatic melanoma.41
Radiotherapy
historically, melanoma has been considered to be relatively radioresistant and radiotherapy has generally only been used as a treatment option in patients with central nervous system (CnS) involvement and brain metastases. Following preclinical data that suggested that focal highdose radiation can make tumors more immunogenic,42,43 a phase I study of stereotactic body radiation therapy (SBRT) followed by hD IL-2 was undertaken for patients with metastatic renal cancer or melanoma.44of the seven patients with melanoma in this study, five had objective responses.44 Additional research may be warranted to investigate the molecular basis of this response and to determine the whether the result is reproducible in a larger trial. A randomized clinical trial comparing SBRT and IL-2 versus IL-2 alone is currently under way.
Other Investigational Strategies
Recent discoveries in the biology of melanoma biology and immunology have led to the development of novel therapeutics, and several immunotherapies are in development for use in metastatic melanoma. A novel immunotherapy strategy for the treatment of melanoma involves blockade of programmed death ligand 1 (PD-L1), a negative regulator of the immune system. one mechanism by which melanoma cells are thought to evade immune system surveillance is through tumor surface expression of PD-L1 which, when bound to PD-1 (present on activated lymphocytes), induces immune tolerance. Recently, two separate trials have demonstrated the safety and efficacy of an anti-PD-1 and an anti-PD-L1.45,46 In both, responses occurred up to 30 % of patients and most importantly the response were durable (>12 months) in the majority of patients. In addition, treatment with anti-PD-1 and anti-PD-L1 antibodies is associated with manageable toxicities.
Adoptive cell therapy (ACT) represents another promising strategy for patients with advanced melanoma. This strategy involves the ex vivo expansion of tumor infiltrating lymphocytes (TILs) obtained from the resection of metastatic tumor deposits and their subsequent reinfusion into lymphodepleted patients, accompanied by IL-2 administration. ACT has shown oRRs of 49–72 % and with increased lymphodepletion, CR rates can approach 40 % and are associated with durable responses of over 7 years.47 Although patients need to be medically fit for this inpatient treatment, and this strategy is both labor-intensive and requires laboratory expertise, the safety and efficacy of this treatment have been demonstrated in clinical trial data from six centers.48
Sequential Therapy
Given that there are four first-line therapeutic options for patients with advanced melanoma and also that each patient has a unique clinical situation, choosing the order of therapies poses a dilemma given the lack of randomized, prospective trials to help guide decision-making. A recent retrospective study, presented at the 2012 American Society of Clinical oncology (ASCo) meeting, examined the sequencing of vemurafenib with immunotherapy (ipilimumab or IL-2).49 In patients treated with vemurafenib following immunotherapy, RRs were similar to that seen in previously untreated patients. Conversely, the median PFS and oS for patients receiving immunotherapy after discontinuation of vemurafenib were poor. This was hypothesized to be due to rapid progression of disease following vemurafenib discontinuation, and it was suggested that immunotherapy should be considered prior to the development of resistance to vemurafenib. The Eastern Cooperative oncology group (ECog) is planning the E1612 study to test the optimal sequencing of ipilimumab and vemurafenib (i.e. ipilimumab followed by vemurafenib against vemurafenib followed by ipilimumab).50 Appropriate sequencing of current immunotherapies is also under investigation. A recent retrospective study aimed to determine if prior response or PFS to hD IL-2 therapy was associated with oS to subsequent treatment with ipilimumab11 and found that prior clinical response to hD IL-2 did not predict benefit to subsequent ipilimumab treatment. Similarly, a 12 % oRR to ipilimumab was demonstrated in patients who had received IL-2 and progressed before receiving ipilimumab.22 Interestingly, in the retrospective study,11 17 % of the patients treated with hD IL-2 required no further systemic treatment, highlighting the value of hD IL-2 as a first-line treatment in select patient.
Summary and Concluding Remarks
Expert opinions of optimum therapeutic approaches to malignant melanoma are given below, and Figure 1 presents case studies to illustrate these approaches. If patients have limited metastatic disease, without evidence of rapid widespread progression, then complete resection of all disease is an option to consider. This is a more favorable option when the site is solitary. For other patients, options most likely to be curative such hD IL-2 or ipilimumab would seem appropriate for patients that are suitable for these strategies. Targeted therapies such as vemurafenib offer the possibility of a rapid anti-tumor response and would seem to be most appropriate for patients with a BRAF mutation who are not suitable for immunotherapy. ACT with TIL and PD-L1 represent investigational options. given the promising preliminary findings of both ACT and PD-L1, it is reasonable to suggest either of these options as a front-line strategy in the setting of a controlled clinical trial. Emerging therapies for the treatment of metastatic melanoma still need to be proven to be safe and efficacious, while all of the currently approved therapies for metastatic melanoma have limitations. The major challenge is to improve the RRs to ipilimumab, IL-2 and DTIC, and increase the duration of response to vemurafenib. The optimal sequencing of these therapies remains unknown, and there is little prospective data to guide clinicians. If eligible, patients should undergo therapy in the context of a clinical trial setting so that optimal therapies, sequencing, or combinations defined by efficacy, safety, and durability can be identified. Sequential therapy, and/or treatment with combinations of targeted agents, will hopefully lead to improved treatment efficacy and is currently an area of intensive clinical research.
Expert Panel Opinion in Terms of Current Therapies and Future Directions for Metastatic Melanoma Treatment
With the emergence of new and effective therapies for metastatic melanoma, clinicians and patients are presented with the dilemma of trying to determine treatment selection and sequencing without the benefit of randomized, prospective data to guide these decisions. When first meeting a new patient with metastatic melanoma or presented with a patient with high-risk disease who has evidence of new metastatic disease, several important pieces of information are required to make a treatment decision. These include:
- Presence or absence of brain metastasis.
- Breadth and rate of growth of disease.
- Performance status and medical co-morbidities.
- Fitness for high-dose IL-2 (i.e. cardiac, pulmonary function).
- history of autoimmune disease.
- BRAF mutational status.
- Presence of other oncogenic mutations.
In general, we explore the possibility of immunotherapies such as highdose IL-2, ipilimumab, or anti-PD-1 (on clinical trial) as first-line therapy independent of BRAF status. A patient may not be an IL-2 candidate or clinical trial candidate for many reasons including active brain metastases, rapidly progressing disease, infirmity/poor performance status, advanced age (rarely offered to patients greater than 70 years old), and comorbid conditions such as cardiovascular, cerebrovascular, or pulmonary disease.
The presence of active brain metastases is problematic, as this requires dedicated therapy (surgery, stereotatic radiosurgery [SRS], whole brain radiation [WBXRT]), typically prevents enrollment to a clinical trial. Importantly, both ipilimumab and BRAF inhibitors have shown activity in patients with brain metastases and are reasonable options for these patients.51,52 In the case of patients with limited brain disease and good performance status, the brain disease should be addressed by surgery and/or stereotactic radiotherapy. Interestingly, the fact that ipilimumab and ACT have been documented to have an impact on active brain metastases, suggests that activated lymphocytes can effectively traffic to the brain.53
For patients with rapidly progressing disease and an elevated LDh, ipilimumab and high-dose IL-2 are typically less effective,11 as response take weeks to months to be realized. For these patients, we favor an approach that will slow the progression of disease so that an immunotherapy may be used later. For patients with high volume or rapidly progressing disease harboring a BRAF mutation, we would favor starting with a BRAF inhibitor either as single agent or in combination on a clinical trial. For patients who are BRAF wild-type, again we would favor a clinical trial utilizing either targeted or cytotoxic agents.
Future Directions of Sequencing or Combining Immune and Targeted Therapy
As mentioned, the optimal combination or sequencing of immune and targeted therapy remains unknown and requires prospective testing to identify a “best” regimen if such thing exists. Several factors need to be considered when trial designing. First, the optimal sequence of immune therapy and targeted therapy should be addressed, and trials that start with one therapy and then switching to another at the time of progression are in development. Second, the subtler question of trying to optimize the timing of the sequence therapies also must be answered. For example, there is emerging preclinical data to suggest that a tumor is more immune evasive at the time of BRAF resistance suggesting that immune therapies may be less effective once BRAF resistance has occurred in the patient.54,55 Trials that address an optimal time to add an immune therapy after a patient begins a targeted agent but before they develop resistance to the targeted agent is a worthwhile objective. Third, in addition to sequencing immune and targeted therapies, trials that combine immune and targeted therapies should be performed to evaluate both the safety and efficacy.
Two Case Studies with Suggested Treatment Strategies for Each Case
Case 1
A 41-year-old female with no prior history of melanoma presents with abdominal fullness and increased fatigue. Imaging reveals widespread metastatic disease of the liver, lungs, and mesentery. A liver biopsy reveals metastatic melanoma and mutational testing reveals a v600E BRAF mutation. Magnetic resonance imaging (MRI) of the brain is without metastatic disease. Patient’s performance status is ECog 1 and limited by abdominal pain. her labs reveal a mild transaminitis and an LDh that is three times normal.
Suggested Therapy In this scenario, the patient clearly has high-volume disease with an elevated LDh. Retrospective data from the analysis of 208 patients who received high-dose IL-2 with metastatic melanoma revealed that patients with an elevated LDh were unlikely to respond to high-dose IL-2, and prior studies have also suggested that patients with extensive disease are less likely to respond to high-dose IL-2 than patients with cutaneous, lymph node, or lung metastasis.10 Also, in a subset analysis of the phase III study involving ipilimumab versus gp100, the hazard ratio for patients with an LDh greater than normal crossed 1.0 indicating these patients did not receive a significant oS benefit from ipilimumab compared with the patients who received gp100.7 given this rationale, we would prefer to start the patient either on a BRAF inhibitor as a single agent or in combination with another targeted agent on a clinical trial with a goal of achieving a rapid and to slow disease progression. Switching to an immune therapy either at the time of progression or the time of best response to vemurafenib are rationale second-line options.
Case 2 A 43-year-old gentleman with a history of 0.54 thick, non-ulcerated melanoma presents with new onset right axillary adenopathy. Imaging reveals a right axillary mass, four lung nodules, and no brain metastasis. An excisional biopsy of the right axilla lymph node reveals metastatic melanoma and BRAF testing is wild-type. The patient undergoes surgical resection of the axillary lymph nodes for palliative reasons and he has an uneventful recovery from surgery. his current performance status is 0, and his labs are all within normal limits including LDh.
Suggested Therapy
The patient is BRAF wild-type, has low-volume disease, and an excellent performance status. In our opinion, this patient would be a good candidate to start with immune therapy, including hD IL-2, ipilimumab, or participation in a clinical trial that involves anti-PD-1 agents or a combination immunotherapy based on hD IL-2 and ipilimumab. If the patient progresses on front-line immunotherapy, we would again assess the patient’s performance status, rate and degree of progression, and LDh levels. If the patient again has low-volume disease that is slowly progressing, we again would favor a immune therapy in the second line. If the patient rapidly progresses after front-line immune therapy, we would tend to favor an alterative to immune therapy and likely a clinical trial.