Neuroendocrine tumours (NETs) is a collective term for a diverse range of neoplasms that arise from cells that originate in the endocrine and nervous systems and share common morphological and immunohistochemical features, including the presence of secretory granules. These tumours can secrete a variety of neuropeptides, which may or may not cause characteristic hormonal symptoms (functioning or non-functioning NETs).
NETs have generally been considered rare; their incidence has been estimated at 2.5 to 5 per 100,000 people per year and prevalence of 35 per 100,0001 and may be higher if undiagnosed NETs are included. Autopsy studies have indicated that pancreatic NETs (pNETs) occur in 0.8 % to 10 % of patients undergoing a post-mortem examination.2 However, data from the largest US epidemiological database (SEER) indicate that the incidence of gastroenteropancreatic NETs (GEP-NETs ) is increasing dramatically in the US: a fivefold increase has been reported between 1973 and 2004 (see Figure 1). The incidence of GEP-NETs has risen steeply since 1992, and more than doubled since 1985.3 This is in contrast to the overall incidence of malignant neoplasms, which has remained relatively consistent since 1992. NETs of the lung, rectum and small intestine are currently the most frequently diagnosed NETs in the US and are also the three subgroups of NETs that have increased in incidence by the greatest margin from 1973 to 2004.3 The age-adjusted incidence of NETs of the small intestine and digestive system has increased by 460 % and 720 %, respectively, over the past 30 years.4
NETs that secrete peptides and neuroamines can cause recognisable clinical syndromes, including carcinoid syndrome.4 However, due to the indolent nature of NETs, many patients are asymptomatic in the early stages, or present with only vague symptoms such as abdominal pain.4 As a result, NETs are frequently metastatic at the time of diagnosis: liver metastases are observed in 40 % of patients who present with small intestinal and 60–70 % of patients with pNETS.3,5 Other factors influencing the presence of liver metastases include the primary tumour site, tumour stage, histological differentiation and proliferative activity (grading; G1–G3). Carcinoid syndrome is frequently associated with distant metastases, especially in the liver. The prognosis for NETs varies according to proliferative activity: median survival in distant metastatic disease was 33 months in patients with G1–G2 graded NETs, but only 5 months in patients with poorly differentiated carcinomas.3 The 5-year survival rate was 35 % in well to moderately differentiated (grade 1/2) NETs, but less than 5 % in poorly differentiated grade 3 NETs.3
The first-line treatment strategy for NETs is surgery, but this is rarely curative, as most patients present at advanced stages of disease.3,5 Other treatment options include cytoreduction, radiological intervention (by embolisation and radiofrequency ablation) and chemotherapy.4 Surgical debulking can reduce the extent of hormone production and relieve symptoms, but owing to the long disease course, palliative care is important. Somatostatin analogues (SSAS), including octreotide and lanreotide, were introduced to control symptoms that result from release of peptides and neuroamines. Octreotide is the most studied SSA. This article aims to review the 25 years of clinical experience with octreotide in treatment of NETs.
Development and Clinical Uses of Octreotide
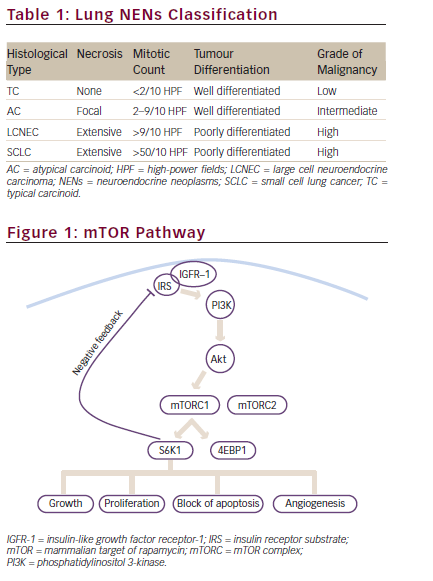
Octreotide is a synthetic octapeptide SSA with more prolonged pharmacological actions than the endogenous hormone. Native somatostatin has a half-life of 2–3 minutes; octreotide has a halflife of 90–120 minutes when administered subcutaneously, and a pharmacodynamic action lasting up to 8–12 hours.6 Since octreotide resembles somatostatin in its physiological activities, it affects numerous pathways that may confer antiproliferative effects in NETs through inhibition of tumour angiogenesis and inhibition of secretion of growth factors.7,8 Direct mechanisms by which octreotide achieves tumour regression include binding to somatostatin receptors sst2 and sst5 , which are found in high density on tumour cells,9 and thereby inhibiting hormone secretion from the tumour, inducing apoptosis and cell cycle arrest, mainly through the regulation of phosphotyrosine phosphatase (PTP) and mitogen-activated protein (MAP) kinase. Binding to sst2 and sst5 receptors, octreotide blocks the effects of growth factor receptor stimulation and results in increased production of the cell cycle inhibitor p27.7 Binding to sst2 receptors, SSAs affect the PI3K/Akt/mammalian target of rapamycin (mTOR) pathway and SHP1 signalling and may overlap with pathways used by the mTOR inhibitor, everolimus.10 Indirect effects include inhibition of angiogenesis and the release of secretory factors required for tumour growth, as well as modulation of the immune system (see Figure 2), and inhibition of insulin-like growth factor 1 (IGF-1) secretion.7,8,11
Octreotide is approved in the US and Europe for treatment of severe diarrhoea/flushing episodes associated with metastatic carcinoid tumours and profuse watery diarrhoea associated with vasoactive intestinal polypeptide (VIP)-secreting tumours.12,13 Octreotide is also approved in 42 countries for tumour control for advanced midgut NETs based on the Placebo-Controlled Prospective Randomized Study on the Antiproliferative Efficacy of Octreotide acetate LAR in Patients with Metastatic Neuroendocrine Midgut Tumours (PROMID) study.14 Additionally, treatment guidelines now recommend the use of octreotide as an antiproliferative agent in patients with functional and non-functional midgut NET,15,16 based on results from the randomised phase III PROMID trial.17 Pooled data from more than 14 trials including almost 400 patients revealed that 71 % of patients with GEP-NETs and carcinoid syndrome experience resolution or improvement of diarrhoea (range: 40–88 %) and flushing (range: 48–100 %) during treatment with octreotide.18–20 Octreotide can be used peri-operatively and may prevent carcinoid crisis, i.e. the immediate onset of debilitating and lifethreatening symptoms that are associated with carcinoid syndrome.21
Octreotide may also be used in asymptomatic patients at the time of diagnosis of metastatic disease.19 There is evidence that the impact of octreotide extends beyond symptom relief. A single-institution retrospective study of 90 consecutive patients with advanced GEP-NETs who received octreotide for carcinoid syndrome, found that a much greater percentage of patients treated with octreotide achieved 5-year survival from diagnosis compared with historical controls (67 % versus 18 %, respectively).22 Subsequent analysis of the SEER database found that survival in patients with metastatic NETs increased from 19 months (1973 to 1987) to 39 months (1988 to 2004) following the introduction of octreotide (see Figure 3).3 This increased survival was observed in patients with GEP-NETs and distant metastases; patients with localised and regional disease did not exhibit significantly extended survival time. A possible explanation for this improvement may be that not only does octreotide achieve control of the symptoms of carcinoid syndrome but also has a potential antiproliferative effect, which could alter the natural history of NETs. Potential lethal consequences associated with carcinoid crisis, such as severe flushing, diarrhoea, valvular heart disease and haemodynamic instability, are now rare occurrences. Complications due to tumour progression tend to occur later in the disease course.3
The development of the long-acting release (LAR) formulation of octreotide in 1997 (Sandostatin® LAR, Novartis) further improved the clinical utility of this drug. Octreotide acetate LAR (octreotide LAR) is a formulation in which octreotide acetate is encapsulated in microspheres of a slowly dissolving polymer, providing a predictable pharmacokinetic profile and steady-state kinetics when injected intramuscularly once every 28 days.23 Octreotide LAR retains the pharmacological characteristics of the previous subcutaneously (SC) administered formulation of octreotide, and reaches steady-state concentrations within three injections.24 A retrospective study compared survival in 145 patients with carcinoid syndrome who received octreotide LAR between 1996 and 2004 to 90 patients who received SC octreotide between 1986 and 1995. Patients who received treatment with octreotide LAR had a 66 % (range 46–82 %) lower risk of death than patients who had received SC octreotide (p<0.0001).25
The benefits of octreotide LAR therapy are clearly established. However, recently, the effect of octreotide LAR in controlling tumour growth has been demonstrated.17,26–28 Multiple uncontrolled studies showed that administration of octreotide is associated with tumour stabilisation in patients with progressive NETs.11,29–32 However, these early studies failed to comprehensively define the role of octreotide in controlling tumour growth, since studies were small, single-centre and not placebo controlled. Furthermore, patients were not treatment naïve and data from GEP-NETs of different origin, (foregut, midgut and hindgut) were analysed together. The observed growth-inhibiting effects of SSAs were not identical in these subgroups and, because of the small numbers involved, firm conclusions could not be drawn. A randomised, double blind, placebo-controlled trial enrolling a homogenous group of patients was necessary to provide definitive evidence of an antiproliferative effect of octreotide LAR.
Clinical Data Demonstrating the Antiproliferative Effect of Octreotide
There is a long history of evidence for the antiproliferative effects of octreotide. Evidence from preclinical cancer models showed that octreotide LAR had antitumour activity.33 In prospective studies, octreotide LAR has exhibited an antiproliferative effect in the following types of NET: entero-pancreatic, well-differentiated endocrine carcinomas,29 gastric carcinoid tumours,11 metastatic or locally advanced, well-differentiated NETs,30 progressive NETs of the pancreas and bronchial tract31 and advanced, progressive metastatic gastrinoma characterised by Zollinger- Ellison syndrome (ZES) and liver metastases.32 Table 1 summarises clinical studies that have demonstrated the antiproliferative effect of short- and long-acting formulations of octreotide.
The most robust data have been provided by the phase III PROMID trial. In this study, newly diagnosed and treatment-naïve patients were randomised to placebo or octreotide LAR administered intramuscularly every 28 days for 18 months or until tumour progression or death.17 To avoid a heterogeneous patient population with GEP-NETs of different origin and biological behaviour, only patients with well-differentiated metastatic or locally inoperable midgut tumours were included.
Midgut NETs represent the largest subgroup of NETs, and by targeting these patients, the PROMID study therefore involved the largest homogeneous NET patient population. Enrolment criteria permitted patients to have either a functioning (patients that could tolerate symptoms with loperamide and clinical support) or non-functioning tumour: those with symptoms of carcinoid syndrome and increased urinary 5-hydroxyindole acetic acid (5-HIAA) were classified as having a functioning tumour. Hepatic tumour load (HL) was quantified by computed tomography (CT) or magnetic resonance imaging (MRI).
Results from 85 patients showed that the median time to tumour progression (TTP) in the octreotide LAR and placebo groups was 14.3 and 6 months, respectively (hazard ratio [HR] = 0.34; 95 % confidence interval [CI] 0.20.0.59; p=0.000072) (see Figure 4).17 After 6 months of treatment, stable disease was observed in 66.7 % of patients in the octreotide LAR group and 37.2 % of patients in the placebo group. he HR for overall survival (OS) was 0.81 (95 % CI 0.30.2.18). Most patients in the PROMID study benefited from octreotide LAR 30 mg therapy, although those patients with non-functioning NETs experienced the most benefit. Safety data were consistent with those seen in previous studies of octreotide LAR. While the proportion of patients with extended TTP was highest in those with low HL (.10 %) versus placebo, subgroup analysis of data from patients with HL >10 % (n=21) revealed that octreotide LAR extends TTP regardless of HL.27
The beneficial effects of octreotide LAR may also include OS: patients from the PROMID trial were followed at least once a year until January 2013. In the HL <10 % subgroup, median OS was not reached (octreotide LAR) versus 80.5 months (placebo) (HR=0.56, 95 % CI 0.25.1.23; p=0.14). In the HL >10% subgroup, OS was 35 versus 84 months (HR=2.18, 95 % CI 0.75.6.33; p=0.14). The estimated HR of 0.56 in octreotide LAR-treated patients in the subgroup with low HL indicated a risk reduction of 44 % compared with placebo.26 This benefit was confirmed after 84.7 months of median follow-up.26 Also, the recently presented phase III, randomised, double-blind, placebo-controlled Lanreotide Antiproliferative Response in patients with GEP-NET (CLARINET) study with 204 NET patients enrolled, demonstrated the antiproliferative effects of another SSA . lanreotide.34
The RAD001 in Advanced Neuroendocrine Tumors, Second Trial (RADIANT-2) was a multinational, randomised, double-blind phase III trial with 429 patients with functioning NET that aimed to evaluate the combination of everolimus + octreotide versus placebo + octreotide.28 Patients included in the study had functioning NETs, low or intermediate grade, with inoperable or locally advanced disease. All patients had radiological documentation of progression within 12 months of randomisation. About 50 % of the patients had primary tumours from the small intestine and 80 % of patients had well-differentiated tumours.About 80 % of patients had used SSAs for about 2.5 years; 78 % ofpatients had used octreotide LAR (at doses between 10 to 20 mg/day, more commonly used at that time). By restricting the analysis to the placebo group only, the RADIANT-2 also evaluated the anti-proliferativeeffect of SSAs. The median duration of treatment was 37 weeks for patients treated with octreotide LAR only group (placebo). The medianprogression-free survival (PFS) in this group was 11.3 months. These data may support the antiproliferative effects of octreotide acetate LAR demonstrated in the PROMID study.
As a result of these data, the European Neuroendocrine TumorSociety (ENETS) 2012 guidelines stated that the use of SSAs, especially octreotide acetate LAR, is recommended for antiproliferative purposes in functioning and non-functioning midgut tumours.15 The National Comprehensive Cancer Network also recommends octreotide acetate LAR as a treatment option in patients with asymptomatic metastatic GI-NETs in addition to use in symptomatic patients and patients with significant tumour burden, progressive disease and local effects.16 Additionally, the recently presented CLARINET study demonstrated that dence f the antiproliferative effect of SSAs.
Future studies should establish the efficacy and safety of octreotide LAR in combined treatment regimens. Although higher doses have been used and have been effective when needed to relieve refractory symptoms,9 30 mg is the approved dose based on clinical trial evidence.17,28 Numerous clinical studies have examined the efficacy and safety of octreotide in combination regimens. A randomised study (n=109) compared subcutaneous octreotide alone or in combination with IFN-a. Survival in the combined arm was prolonged but did not achieve statistical significance. Response rates in both arms were less than 6 %.35 Another trial with interferon alpha (IFN-a) failed to reach statistical significance.36 The underpowered nature of the studies to date precludes any definitive conclusions regarding the effects of IFN-a on OS. Furthermore, the adverse events (AEs) associated with IFN-a have lessened enthusiasm for this combined regime.
Octreotide LAR, in combination with everolimus, has shown reduced disease progression in low- to intermediate-grade metastatic, unresectable carcinoid tumours or islet cell tumours,37 advanced pNETs38 and lung39 and colorectal NETs.40 Further analyses of the placebo arm of the RADIANT-2 study may reveal more data on the effect of octreotide in this study population.
Safety and Tolerability of Octreotide
The safety profile of octreotide is well established, and both the shortand long-acting formulations are well tolerated in clinical practice and have been associated in improvements in quality of life.41 The most frequent AEs associated with the use of octreotide LAR include pain at the injection site (10–20 % of patients), mild hyperglycaemia and mild-to-moderate GI disturbances, such as loose stools, abdominal cramping, nausea and flatulence, which persist in 5–15 % of patients.17,28,42,43 Octreotide therapy confers a risk of cholelithiasis, which may increase with longer treatment periods. Octreotide-associated biliary tract alterations, such as gallstones, sediment and sludge, have Ben reported in up to 20 % of patients, but are usually asymptomatic and do not require surgical or pharmacological intervention.44 It should be stressed that most studies investigating the safety and tolerability of octreotide have short-term follow up but in clinical practice, the drug is often administered for many years. Long-term AEs are less certain and could potentially be underestimated.
Summary and Concluding Remarks
The incidence of GEP-NETs is increasing dramatically. Over the past 2Q5 years, octreotide has become an essential component in the management of patients with GEP-NETs. Its potent anti-secretory effects and multiple mechanisms of action, combined with its established safety profile, make it a reliable treatment option. Furthermore, clinical data support the antiproliferative effect of octreotide LAR in patients with well-differentiated metastatic midgut NETs. Octreotide LAR may also be considered as treatment option for patients with welldifferentiated metastatic non-midgut NETs, regardless of functional status. These expanded therapeutic indications for octreotide LAR are under investigation in numerous clinical settings.