KIT is transmembrane protein that functions as the receptor of the stem cell factor (SCF) and as a tyrosine kinase. Most KIT mutations occur in untreated GISTs in exon 11 that encodes the intracellular juxtamembrane part of the protein, and only rarely in exons that encode the intracellular kinase domain.
In imatinib-treated patients secondary mutations are frequent in exons encoding for the kinase domain (the ATP/imatinib binding pocket or the kinase activation loop).
Diagnosis
GISTs vary in malignancy potential ranging from small, incidentally detected tumours with excellent outcome to aggressive sarcomas. The proportion of overtly malignant or high risk GISTs is 20–35% of all GISTs.1,2 This suggests that the annual incidence of GISTs with a high malignancy potential is about five per one million.
Many small, asymptomatic GISTs may remain undetected, and the frequency of reported GISTs could change with time because of evolving diagnostic criteria and greater awareness of GIST.3
The KIT protein is detectable by immunohistochemical (IHC) assays, and the gene mutations can be detected by DNA sequencing. Other useful diagnostic features for GIST are negative immunostaining for desmin and absence of lymph node and lung metastases. Clinical Presentation
The most common symptom at presentation is bleeding.4 Large GISTs often protrude from the site of origin and grow between the bowel loops and the abdominal organs, but they may also erode the GI tract lumen. Patients may also have various other symptoms, such as abdominal pain or discomfort, early satiety, bloating, obstructive jaundice, dysphagia, fever and anaemia-related symptoms, such as fatigue and palpitations,4 or they may present with an abdominal tumour with no symptoms. Ten per cent to 25% of patients present with metastatic disease.1,5
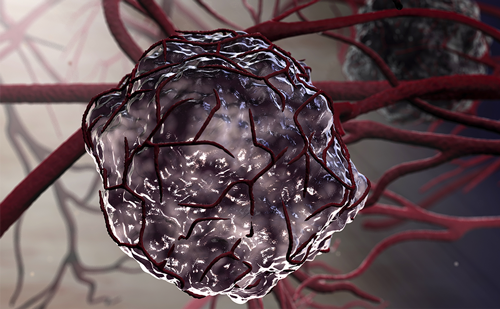
GISTs can originate anywhere in the GI tract. The stomach (40–60%) and small intestine (30–40%) are the most common locations. The colon, rectum and oesophagus are other sites of origin. GISTs frequently give rise to numerous intra-abdominal metastases located on the peritoneal, omental, mesenteric and other serosal surfaces, and to liver metastases, but metastases outside the abdomen are rare. GISTs have a high tendency to seed. The intraabdominal lesions probably result from tumour cell seeding into the abdominal cavity, whereas liver metastases probably result from haematogenous spread. GISTs range in size from a few millimetres to 35cm, with a median size of between 5cm and 8cm.1,6 GISTs probably originate from the interstitial cells of Cajal or their precursors.7 Interstitial cells of Cajal are the pacemaker cells of the GI tract controlling gut motility.
Prognosis
Many GISTs have an uncertain malignancy potential. The most commonly used scheme to assess the risk of recurrence is the consensus approach, which is based on the primary tumour diameter and the mitotic count.8
According to Surveillance, Epidemiology, and End Results (SEER) registry data, the relative five-year survival rate for GIST patients diagnosed in the US between 1992 and 2000 was 45%.5 The five-year survival rate ranges from 50% to 65% after complete resection of localised primary tumour,9 but 40–90% of surgical patients have a post-operative recurrence or metastasis. Median survival time of patients with metastatic or locally recurrent GIST was 10–20 months before the imatinib era.9