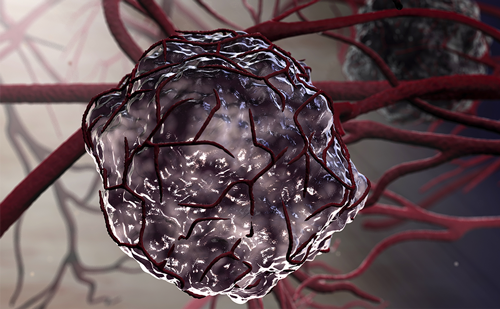
Gastrointestinal stromal tumours (GISTs) are rare mesenchymal tumours that may develop anywhere along the gastrointestinal tract. Approximately 95 % of cases share the expression of the CD117 surface antigen, also known as KIT or stem cell factor receptor. The management of localised GISTs relies on the complete surgical excision of the tumour. Until the introduction of tyrosine kinase inhibitors (TKIs), limited treatment options were available for patients once the tumour had spread or if it was inoperable.1
Unprecedented improvement in the management of advanced GIST has been achieved through the relatively recent recognition of the important biological role of activating mutations in the KIT and PDGFRA (platelet-derived growth factor receptor-alpha) genes. These observations led to the introduction into therapy of imatinib mesylate, a small-molecule selective TKI targeting stem-cell factor receptor (KIT, CD117), breakpoint cluster region/C-abl oncogene 1, non-receptor tyrosine kinase (BCR/ABL) and platelet-derived growth factor receptors (PDGFRs) A and B. Imatinib revolutionised the treatment of patients with advanced CD117-positive GISTs and is currently approved as first-line treatment in metastatic and/or inoperable disease.2–6 However, approximately 10–15 % of GIST patients are initially insensitive to imatinib, around 5 % are intolerant to it, and the spectacular response of the remaining patients is time-limited. As shown by median progression-free survival (PFS), approximately 50 % of patients treated with imatinib ultimately develop secondary resistance and experience disease progression within two years of treatment initiation.2,3,5 The management of GIST resistant to first-line treatment represents a clinical challenge.5 Insights into resistance mechanisms have allowed the development of several alternative strategies for patients who experience disease progression following imatinib treatment, which are currently being tested. In the case of generalised disease progression (or intolerance to imatinib), monotherapy with an alternative multitargeted TKI – i.e., sunitinib – represents the main option. Sunitinib remains the only approved second-line drug for the treatment of advanced GIST after failure of imatinib therapy.7
To view the full article in PDF or eBook formats, please click on the icons above.