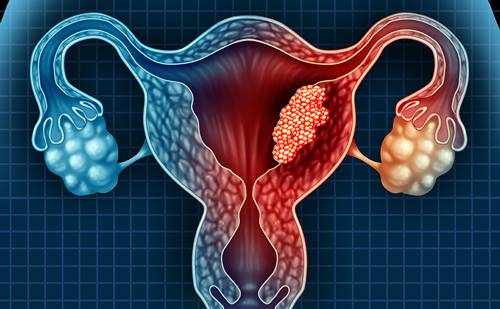
Over 130 HPV types have been identified, and approximately 40 of these cause genital infections. Infection with low-risk types, such as 6 and 11, may cause anogenital warts. Vertical transmission of lowrisk HPV types from mother to neonate may cause recurrent respiratory papillomatosis (RRP), which are warts in the upper airway of young children. Approximately 90% of genital warts and almost all cases of RRP are caused by these two HPV types. Genetic and epidemiologic studies have demonstrated that infection with high-risk types, such as 16 and 18, is a necessary cause of cervical cancer. At least 99% of cervical cancers contain one or more of the 15 recognised high-risk types, and approximately 70% contain HPV types 16 or 18. Natural history studies have demonstrated that persistent infection with high-risk HPV types, indicating on-going viral replication, is the key factor in the development of cervical cancer precursor lesions. These include moderate/severe cervical intraepithelial neoplasia (CIN 2/3), precursors to cervical squamous cell carcinoma, and adenocarcinoma in situ (AIS), a precursor to cervical adenocarcinoma. HPV infection also causes up to 50% of vulvar and vaginal cancers in women and a proportion of penile and anal cancers in men. Head, neck, and oesophageal cancers have also been linked to HPV infection.
HPV Vaccines
Vaccines that prevent infection with the most common HPV types have been developed and are being evaluated for efficacy in large, phase III clinical trials. These vaccines are comprised of virus-like particles (VLP), recombinant viral capsids that are identical morphologically to HPV virions, but contain no viral DNA. Thus, they can induce a neutralising antibody response but pose no risk of HPV infection or cancer.
These vaccines target HPV types 16 and 18, with or without types 6 and 11. The results of a randomised, double-blind, placebo-controlled trial evaluating the clinical efficacy of an HPV-16,18 vaccine (Glaxo- SmithKline Biologicals, Rixensart, Belgium), were published in 2004. A total of 1,113 women 15 to 25 years of age were randomised to receive HPV-16,18 vaccine or placebo at day 0, month 1 and month 6. In the according-to-protocol analysis, which included those participants who followed the research protocol closely, the vaccine was 100% effective (95% confidence interval 47.0 100%) against persistent infection with HPV 16, 18, or both. The vaccine was 91.6% effective (95% confidence interval 64.5 98.0%) against incident infection with HPV 16, 18, or both. In the intention-to-treat analysis, which included all participants who received at least one dose of vaccine or placebo, vaccine efficacy was 95.1% (95% confidence interval 63.5 99.3%) against persistent cervical infection with HPV 16, 18, or both. Efficacy was 92.9% (95% confidence interval 70.0 98.3%) against HPV 16- or 18-related Pap abnormalities. There were no serious adverse events related to vaccination. Recent data indicate that both antibody levels and clinical efficacy are sustained for at least 4.5 years after vaccination.
Additional studies are on-going to evaluate vaccine efficacy, including studies of older women. Data presented at the 2006 American Society of Clinical Oncology (ASCO) annual meeting demonstrated that 100% of women 15 to 55 years of age who were vaccinated developed an antibody response to HPV 16 and 18 after completing vaccination. The results of a randomised, double-blind placebocontrolled multicentre phase II trial of an HPV 6,11,16,18 vaccine (Merck Research Laboratories, West Point, PA, USA) were published in 2005. Women (n=1,106) from Brazil, Europe and the US who participated in the study received three preparations of the vaccine containing different dosages of the four VLPs at day 1, month 2 and month 6, and subsets were randomised to receive low-dose vaccine (n=277) or placebo (n=275). In the according-to-protocol cohort, the incidence of persistent HPV 6, 11, 16 or 18 infection or disease associated with these four HPV types decreased by 90% (95% confidence interval 71 97%) in women who received the low-dose vaccine compared to placebo. The results were similar in an intentionto- treat analysis. There were no vaccine-related serious adverse events. In a larger clinical trial involving 12,157 young women 16 to 23 years of age, vaccine efficacy in the per-protocol group was 100.0% (95% confidence interval 80.9 100%) in preventing HPV 16- or 18-related CIN 2/3 or AIS, cervical cancer precursor lesions. Vaccination was 98.3% effective (95% confidence interval 90.2 100.0%) in preventing genital warts associated with HPV 6, 11, 16 or 18. Data presented recently demonstrate similarly high effectiveness in preventing vulvar and vaginal high-grade precancerous lesions.
Data from clinical trials of the HPV 6,11,16,18 vaccine demonstrate that if women were already infected with the types contained in the vaccines prior to vaccination, they were not protected against disease caused by those vaccine types. However, those who were infected with one or more vaccinerelated types before vaccination were protected from disease caused by the remaining vaccine types. These results indicate that vaccines should be administered prior to sexual initiation in order to maximise their clinical impact. However, immunisation of young women after sexual initiation is reasonable, because they may not be infected with all types contained in the vaccine, and it will not be feasible to test women for HPV infection with individual HPV types prior to vaccination.
Several important questions remain about the HPV vaccines in development. These include the necessity of booster immunisations after initial vaccination, efficacy of vaccination in immunocompromised individuals and in men, cost-effectiveness of vaccination in different populations, feasibility of vaccination in developing countries, impact of vaccination on Pap screening guidelines, and potential impact of vaccination on sexual behaviours and compliance with Pap screening. On-going research should begin to provide answers to these questions over the coming years. Potential Public Health Impact of HPV Vaccination
Prophylactic HPV vaccines could have an enormous public health impact in the US and worldwide. Despite a dramatic decline in cervical cancer incidence and mortality in more developed countries of the world since implementation of widespread Pap screening, it remains the fourth most commonly diagnosed cancer among women in these countries. It is estimated that in 2006, almost 10,000 new cases of cervical cancer will be diagnosed in US women and about 3,700 of these women will die from the disease. Marked racial and ethnic disparities in cervical cancer incidence and mortality exist in the US, which could be decreased with widespread vaccination. Cervical cancer is the second most commonly diagnosed cancer and a leading cause of cancer-related mortality among women in less developed regions of the world, accounting for approximately 400,000 diagnoses and 230,000 deaths per year. Vaccines containing HPV types 16 and 18 could prevent up to 70% of cervical cancers and a substantial proportion of other anogenital and aerodigestive malignancies. A vaccine directed against HPV 6 and 11 could prevent the vast majority of respiratory papillomas in young children and anogenital warts. Respiratory papillomas, although rare, may cause significant upper airway compromise and necessitate repeated surgical procedures in children. Genital warts are more common, with estimated prevalence rates of 1% to 5% in the general population and up to 40% in men and women attending STI clinics.1, 17, 18 Genital warts may be difficult to treat and often recur despite appropriate therapy. An effective HPV vaccine could also reduce the substantial psychosocial distress and healthcare costs associated with HPV infection and related diseases. to proceedings of a recent ACIP meeting, the organisation will likely recommend that the vaccine be targeted toward 11- to 12-yearold girls, with vaccination of nine- to ten-year-olds under some circumstances and catch-up immunisation of 13- to 26-year-old girls and women. Other professional organisations, such as the American Academy of Pediatrics, will also publish recommendations for vaccination. GlaxoSmithKline is expected to submit an application to the FDA for approval of the HPV 16,18 vaccine (CERVARIX) by the end of 2006.
Key Issues for Vaccine Delivery and Uptake
The public health impact of HPV vaccination will depend on widespread vaccination of young women, ideally prior to sexual initiation. However, a number of challenges remain. First, most women have a poor understanding of HPV infection and its link to cervical cancer. Paediatricians and family physicians, who will be recommending HPV vaccines, may not have extensive knowledge about, or experience with, HPV-related disease. Reaching the most vulnerable adolescents will be difficult, e.g. those who are homeless, do not attend school, or do not have access to a healthcare provider. Even among those adolescents who have a consistent healthcare provider, it will be challenging to ensure that they receive three immunisations over a sixmonth period. The cost of vaccination, which will likely exceed US$300 for the series, may be a significant barrier to vaccination, particularly if third-party payors or the Vaccines for Children Program do not provide coverage. Furthermore, previous experience with new vaccines has demonstrated that vaccine uptake generally is slow in the absence of state legislation mandating immunisation. It is unlikely that mandated immunisation will occur in the near future, both because it will take time to pass legislation and because some organisations may oppose mandated immunisation. Finally, successful vaccine uptake will depend upon HPV vaccine acceptability among providers, parents, and adolescents.
Despite initial concerns about HPV vaccine acceptability, recent studies suggest that the majority of providers, parents, and young adults find HPV vaccination to be acceptable. In national studies of US paediatricians and family physicians, approximately 75% indicated that they would recommend an HPV vaccine if licensed. Physicians identified parental concerns about HPV vaccination as potential barriers to vaccination. However, most parents are supportive of vaccination: 67 83% of parents participating in recent studies indicated that they would agree to have their daughters vaccinated. Key factors in parents decisions to vaccinate their children include a desire to protect their child from cancer; beliefs about the severity of HPV-related disease and their child s susceptibility to HPV infection; attitudes about vaccine safety and efficacy; physician recommendation for vaccination; and personal experience with HPV-related diseases. Although some parents are concerned about a possible adverse impact of HPV vaccination on sexual risk behaviours and compliance with Pap screening, there is currently no evidence that suggests adolescents will practice riskier behaviours if vaccinated.
Public health initiatives and vaccine-related policies may help to maximise vaccine uptake and thus the public health impact of vaccination. Educational materials must be developed for physicians and nurses, both to provide information about vaccination and guide them in terms of addressing any parental concerns. Educational materials for parents and adolescents that are culturally sensitive and promote healthy behaviours are urgently needed. Young women must understand that HPV vaccines will not prevent the acquisition of other STIs, so they should continue to try to minimise STI exposure through abstinence, limiting sexual partners and consistent condom use. Young women must also understand that they should continue to obtain regular Pap tests even after vaccination. The primary rationale for continued Pap screening is that the vaccines will not prevent all cases of cervical cancer, because high-risk types not contained in the vaccines cause approximately 30% of cervical cancers. Pap screening after vaccination will also be important because vaccine efficacy may be compromised if women have been infected previously with HPV types contained in the vaccines, if they do not receive all three immunisations, or if immunity wanes over time. Other strategies that may promote vaccine uptake should be explored, such as vaccination in alternative settings (e.g. schoolbased health centres), legislation to mandate vaccination for school entry and efforts to promote insurance coverage for HPV vaccines.