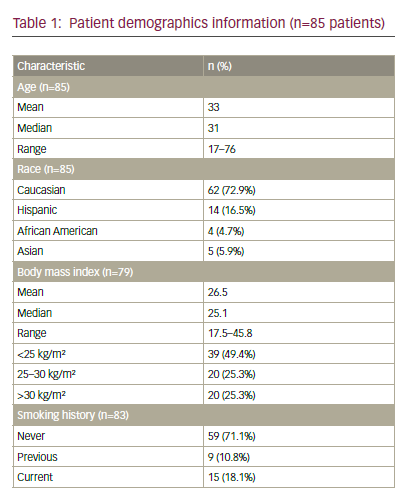
Human papillomavirus (HPV) is thought to be the most common sexually transmitted infection in the US.1 It is estimated that as many as 75–80% of men and women will have contact with HPV at some point in their lives.2 In the US, the highest prevalence of HPV is among females between 20 and 24 years of age. Factors that affect the risk of infection include number of sexual partners, marital status, cigarette smoking, and infection with other sexually transmitted diseases (STDs) such as genital herpes. Infection is also common in women following their first sexual encounter.3
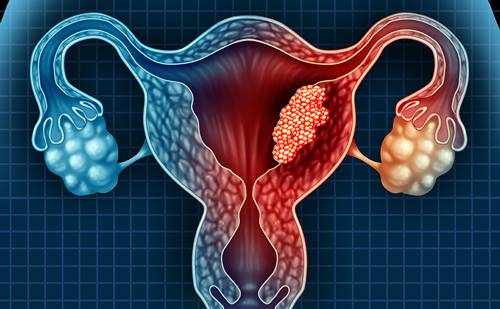
There are approximately 130 identified types of HPV that can result in genital infection. Low-risk types of HPV such as 6 and 11 cause genital warts. HPV infections are the primary cause of cervical cancer, with HPV types 16 or 18 resulting in approximately 70% of all cases. A further 11 high-risk HPV types are carcinogenic.4 Persistent infection with high-risk HPV types is the major factor in the development of cervical cancer precursor lesions, for example cervical intraepithelial neoplasia (CIN), vaginal intraepithelial neoplasia (VaIN), vulvar intraepithelial neoplasia (VIN), and anal intraepithelial neoplasia (AIN). Worldwide, cervical cancer causes 250,000 deaths per year, hence the emphasis is on preventing the disease through vaccination against HPV infection.
Human Papillomavirus Vaccines Two vaccines have been developed to prevent infection with the high-risk HPV types for cervical cancer. The vaccines comprise recombinant viruslike capsules that are morphologically identical to HPV virons, although they contain no actual viral DNA. The first is a quadrivalent vaccine containing HPV high-risk types 16 and 18 and low-risk types 6 and 11, which cause genital warts (Gardasil®, Merck Research Laboratories), and the second is a bivalent vaccine containing types 16 and 18 (Cervarix™, GlaxoSmithKline Biologicals).
Two multicenter phase III trials testing the efficacy of Gardasil have been completed: Females United to Unilaterally Reduce Endo/Ectocervical Disease I and II (FUTURE I and II).5,6 FUTURE I included 5,455 women aged 16–22 years, randomized to receive either the quadrivalent vaccine or a placebo. The women’s progress was followed for an average of three years after the first dose of the vaccine, which was reported to be 100% effective at preventing anogenital diseases associated with HPV types 6, 11, 16, and 18.
The second phase III trial, FUTURE II, included 12,167 women between 15 and 26 years of age. Females were randomized to receive either the vaccine or a placebo, and the end-points were CIN grade 2 or 3, adenocarcinoma, or cervical cancer related to HPV types 16 or 18.6 In this study, the vaccine was reported to have 100% efficacy in the prevention of HPV 16/18, CIN 2/3, or adenocarcinoma in situ (AIS), as well as other cervical cancer lesions. Furthermore, the vaccination demonstrated 99% efficacy in preventing genital warts associated with the same HPV types, and was 100% effective against vulvar and vaginal pre-neoplastic lesions (VIN 2/3 and VaIN 2/3). Thus, widespread immunization of young women with the quadrivalent vaccine would result in a substantial reduction in HPV 16/18-related cervical disease and a reduction in the majority of cases of genital warts.
In the phase II evaluation of the bivalent vaccine, 1,113 women between 15 and 25 years of age were randomized to receive either a three-dose regimen of the vaccine or placebo.7 The vaccine was 91.6% effective at preventing incident infection and 100% effective at preventing persistent infection with the designated HPV types. The vaccine was generally well tolerated and no serious side effects were reported. A follow-up after 4.5 years showed that more than 98% seropositivity was maintained for HPV 16/18 antibodies.8 The vaccine remained 100% effective at protecting against CIN and demonstrated cross-reactivity in preventing HPV types 45 and 31 infections. An interim analysis of 15 months of follow-up data from the phase III testing of the bivalent vaccine demonstrated 90.4% efficacy against development of CIN 2/3 lesions and 80.4% protection against confirmed persistent HPV 16/18 infection.9
Using mathematical modeling, the HPV vaccine appears to be costeffective. 10 The computer-based mathematical model predicted that a 98% prevention of HPV type 16/18 would produce a similar reduction in the amount of HPV 16/18-associated cervical cancers and a 51% decrease in the total number of cases of cervical cancer.
Target Population
Data from all clinical trials for the quadrivalent vaccine demonstrate that the vaccine will not be optimally effective in women who have previously been infected with HPV types 6/11/16/18. Efficacy was much lower (44%) in women who had an HPV 16/18-related CIN or an infection with either type.6 However, those who have been infected with one or more of the vaccine-related types would still remain protected from diseases caused by any of the other HPV types in the vaccine. Thus, it is recommended that the vaccinations be targeted at women prior to sexual initiation to maximize the clinical impact.
From a public health perspective, the vaccination of men alongside that of women should provide further protection within the population. In the UK, the vaccine is licensed for use in girls and boys nine to 15 years of age and women 16–26 years of age, hence men over the age of 16 years may receive the vaccine only off-label. In 2006, the US Food and Drug Administration (FDA) approved the quadrivalent vaccine for use solely in females nine to 26 years of age. The vaccine is not approved for males of any age in the US. However, a study is currently under way to determine its safety and efficacy profile in males.
Implementation of the Vaccine
There is the widespread use of Papanicolaou (Pap) smears in developed countries. Since its introduction, the Pap smear has prevented the development of approximately 50% of cervical cancer cases worldwide. The quadrivalent vaccine will prevent only 70% of infections that cause cancer, and a large number of women over the age of 26 years will not have been vaccinated; hence, for the foreseeable future the Pap test will continue to be part of national programs to prevent cervical cancer, even for women who have been vaccinated.
The quadrivalent HPV vaccine is anticipated to cost approximately $360 for the three-dose series. While the majority of females eligible to receive the vaccine will be covered by private medical insurance, it is estimated that up to 12% of girls nine to 18 years of age and 29% of women 19–26 years of age will be uninsured.11 There are several public funding schemes set up to provide uninsured children with financial support for the vaccine, e.g. the Vaccines for Children program, which covers all vaccines for children who are Medicaid-eligible, uninsured, American Indian or Alaska Native, or underinsured, and the Immunization Grant Program, which awards grants to state, local, and territorial public health agencies.12 This will enable the vaccination program to cover a large majority of the target population. In developing countries, cervical cancer is one of the leading causes of cancer deaths among women, Therefore, the implementation of a vaccination program would have real potential to save lives. National strategies to deliver HPV vaccines in several developing countries are under review and discussion and will likely require public–private partnerships. For the vaccine to be successful it needs to be cost-effective. A study in Australia examined the cost-effectiveness of adding the HPV vaccine to the existing Australian National Screening Program.13 Results were analyzed based on administering a vaccine that prevents 100% of HPV 16/18 type infections to 12-year-old schoolgirls, the end-points being costs per life-year and quality-adjusted life-year saved. It found that the addition of the vaccine was a cost-effective way to reduce cervical cancer. The introduction in Canada of the HPV vaccination also led to a decrease in cervical cancer.14 The main advantage of the vaccine was identified as a reduction of mortality from cervical cancer.
Vaccine Controversies
The HPV vaccine has encountered several difficulties. The first and most important is the general lack of public awareness and knowledge that cervical cancer and cervical dysplasia are caused by infections with HPV, an infection that can be transmitted through skin–skin contact. It is estimated that only 40% of women are aware of the association of HPV virus with cervical cancer.15 One of the biggest public misconceptions has been that immunizing pre-teens against an STD will encourage promiscuity. However, this is considered by most public health experts to be unlikely. Unwanted pregnancy and AIDS are more likely than the threat of cancer, and the distribution of condoms and sexual education regarding these matters has not increased sexual activity in adolescence. Interestingly, a study from the University of Pennsylvania demonstrated that comprehensive sex education delayed initiation of sex, decreased the incidence of unprotected sex, and reduced the number of sexual partners.16
To date, Virginia and the District of Columbia have school entry requirements for mandatory vaccination with the HPV vaccine that should soon take effect, and both have an opt-out option for parents who havemedical, moral, or religious opposition. There has been increasing parental concern over the safety of the vaccine and many parents refuse to allow administration of the vaccine to their children.17 Public knowledge of the safety of the HPV vaccine, as determined in recent clinical trials, will increase the level of parental consent to the vaccination program. Parents with the belief that their child will remain abstinent until marriage view the vaccinations as unnecessary. In the past an abstinence-only sexual education has not been successful at delaying the age of sexual initiation.18 The Centers for Disease Control and Prevention (CDC) has estimated that by 15 years of age 13% of girls are sexually active, and by 17 years of age the figure rises to 43%.19 School-based vaccination programs are important for providing protection from HPV to those most at risk. For the successful implementation of the vaccine, more information needs to be provided to the public on the risks of HPV-related cervical cancer and the benefits stemming from the vaccine.
Summary
HPV is the most common sexually transmitted infection in the US. HPV types 16 and 18 are the most common precursors for cervical cancer, and HPV types 6 and 11 are common causes of genital warts. Persistent infection with highrisk HPV types is the most important factor in the development of cervical cancer precursor lesions. Two vaccines have been developed against HPV: a quadrivalent vaccine comprising types 6, 11, 16, and 18, and a bivalent vaccine including types 16 and 18. The quadrivalent vaccine has been successful at preventing cervical cancer in several clinical trials and was FDAapproved in 2006 to be administered to females nine to 26 years of age. However, the planned introduction of the vaccination has not met with universal welcome. Many parents believe that its introduction will lead to sexual promiscuity. To overcome this obstacle, education on the risks of the disease and benefits of the vaccine need to be presented more effectively.