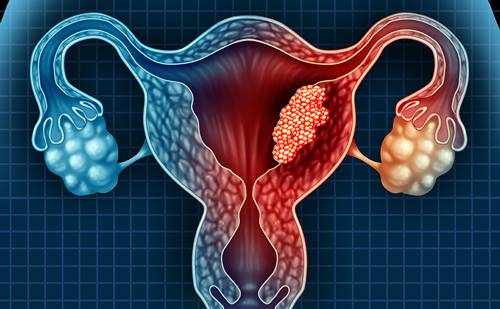
While gynecologists have used laparoscopy for nearly 50 years, it was not until the 1990s that laparoscopy gained acceptance among gynecological oncologists for advanced procedures such as hysterectomy with lymphadenectomy for endometrial cancer. More recently, total laparoscopic radical hysterectomy (TLRH) for earlystage cervical cancer (International Federation of Gynecology and Obstetrics [FIGO] stages IA2 and IB1) has proved both safe and feasible. First described in the early 1990s,1,2 growing evidence supports its benefits and possibly even superiority over laparotomy in radical hysterectomy. While technically challenging with a steep learning curve, clear advantages include decreased operating time, lower patient morbidity, shorter length of inpatient hospitalization, less blood loss, improved cosmesis, and comparable outcomes to laparotomy, including recurrence rates and lymph-node yield. Newer robotic technology alleviates some of the shortcomings of laparoscopy, and robot-assisted radical hysterectomy (RRH) may soon surpass TLRH as a minimally invasive procedure.
Total Laparoscopic Radical Hysterectomy
Both patients and physicians have driven the advancement of minimally invasive surgery. The pursuit of cutting-edge technology by physicians and academic institutions has promoted the expansion of minimally invasive techniques, and training opportunities abound. With increasing public awareness, many patients are now requesting minimally invasive surgery. Patients with early-stage, IA2, or IB1 cervical cancer are traditionally offered an abdominal radical hysterectomy (ARH) and pelvic lymphadenectomy. First described by Canis et al.1 and Nezhat et al,2 TLRH for early-stage cervical cancer has been proved efficacious and safe by a number of other groups3–9 and is gaining in popularity. The best candidates for TLRH include those with early-stage disease (IA2 or IB1), tumor size < 4cm, and uterine size < 12cm. Patients with a bulky uterus or bulky cervical tumors, severe hip or joint disease, or intraperitoneal metastases are generally not suitable candidates for the procedure.
Technique
Informed consent is obtained. All patients undergo pre-operative bowel preparation and receive prophylactic antibiotics. After placement in the lithotomy position with the arms tucked at the sides, a Foley catheter is inserted. A uterine manipulator is placed. The patient is placed in the steep Trendelenburg position. Based on surgeon preference of endoscope size, a 5, 10, or 12mm bladeless trocar is situated at the umbilicus under direct visualization of the abdominal cavity. If the patient has a prior mid-line incision, entry can be made at Palmer’s point 2cm below the left costal margin in the mid-clavicular line. The abdomen is insufflated, and three additional bladeless trocars (5, 10, or 12mm) are placed in the right lower quadrant, left lower quadrant, and the mid-line 2cm above the pubic symphysis. At least one of the three trocars must measure 10 or 12mm in order to permit lymphadenectomy. An abdominal survey is then performed to rule out intraperitoneal disease. The bowel is mobilized out of the surgical field.
The round ligaments are then transected bilaterally. The peritoneum is incised over the psoas muscle immediately lateral to the infundibulopelvic ligament, and the ureters are identified. Any suspicious-appearing lymph nodes are then removed and sent for frozen pathology, as the procedure is aborted in the presence of metastatic disease. Next, the paravesical and pararectal spaces are identified and exposed. The uterine vessels are identified and transected at the point of origin from the iliac vessels. The bladder is then mobilized inferiorly. The ureters are freed from their medial attachments to the peritoneum, and then dissected off the parametrium down to their insertion into the bladder. The vesicouterine ligament is divided at its lateral aspect, and the bladder further mobilized so as to provide ample vaginal margins.
The infundibulopelvic ligaments are transected to accomplish bilateral salpingo-oophorectomy. If ovarian preservation is desired, the utero–ovarian ligaments are transected. The posterior peritoneum is incised and the rectovaginal space entered in order to expose the uterosacral ligaments, which are then transected. A colpotomy is performed and the entire specimen is removed vaginally. The vaginal cuff is then sutured laparoscopically. Attention is then turned to pelvic lymphadenectomy, which is performed from the level of the aortic bifurcation along the external iliac vessels to the circumflex iliac vein. The obturator lymph nodes are then separately removed. If paraaortic lymphadenectomy is performed, it is carried out from the aortic bifurcation in a cephalad fashion to the inferior border of the renal vessels. This is performed only in the presence of positive pelvic lymph nodes. Outcomes
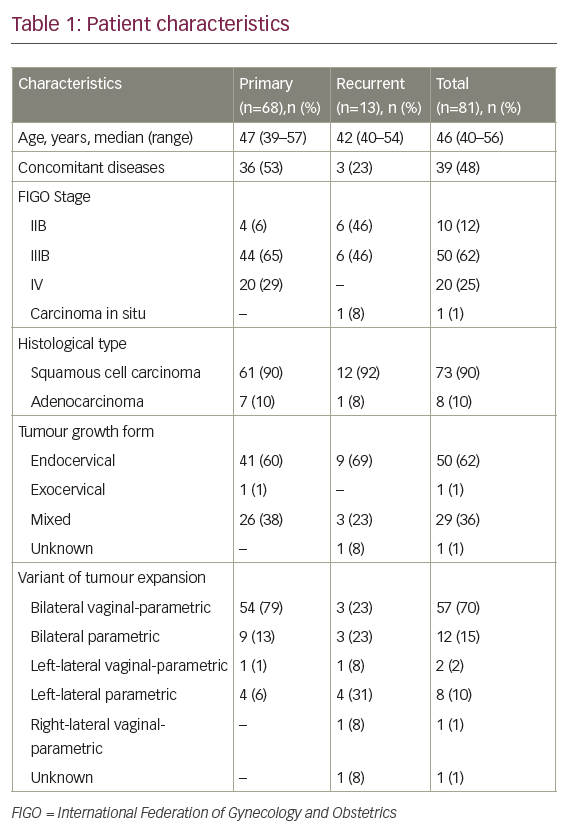
For TLRH, reported operative times range from 162 to 371 minutes (see Table 1), which is generally longer than laparotomy. Frumovitz et al.3 compared these two groups, and found the mean operative time in laparotomy was 307 minutes (n=54) versus 344 minutes (n=35) in the laparoscopic group. However, efficiency improves with experience. For example, in 78 patients undergoing TLRH for earlystage cervical cancer, Spirtos et al.4 reported an initial operative time of 255 minutes for the first 26 cases, which improved to 186 minutes during the last 52 cases. Similarly, in a recent large study by Chen et al.,5 operative time improved from 287 to 153 minutes between the first 50 and subsequent 275 procedures. Hospital stay is significantly lower in TLRH than ARH. Ramirez et al. were the first to report an average length of stay of only one day.6
Blood loss for TLRH averages 200–300cc, which represents a substantial improvement over laparotomy, with an average estimated blood loss (EBL) of >400cc. Intra-operative complications are comparable to those experienced with laparotomy. Chen et al.5 reported a 5.1% intraoperative complication rate including vascular injury, cystotomy, ureteral injury, bowel injury, and hypercapnea. Five of these (1.7%) required open conversion, while the rest were repaired laparoscopically. Ten percent of these patients experienced long-term post-operative complications. Both Ramirez et al.6 and Pomel et al.7 reported no conversions to open laparotomy. Of 20 patients in the former group,6 only one required a blood transfusion; there were three short-term complications (cystotomy, pneumo-mediastinum, and pulmonary embolus) and two long-term complications (vaginal evisceration and a lymphocyst). Of 50 patients in the latter group,7 10 presented with early complications and three required re-operation, while three had late complications, two of which required re-operation. In direct comparison with laparotomy, Frumovitz et al.3 found no difference in post-operative morbidity in the laparoscopic group. However, there was a significantly lower postoperative infection rate in the patients who underwent laparoscopy.
Laparoscopy for cervical cancer yields a higher number of lymph nodes than laparotomy and achieves adequate tissue margins. Of 78 patients in one study,4 three had close or microscopically positive margins and 5% of these patients recurred over 67 months. While Chen et al. reported negative surgical margins for all 295 patients, 16.3% recurred. However, this study included patients with stage IIIA and IIIB cervical cancer. Frumovitz et al.3 compared resection margins between TLRH versus ARH groups, and found no difference in the amount of vaginal cuff or parametrial tissue resected, or in the number of patients with negative tissue margins. Li et al.8 compared morbidity, recurrence rates, and mortality of patients who underwent TLRH versus ARH, and found that recurrence and mortality rates were similar between groups. There are no data providing five-year survival estimates within the TLRH group. Robotic Radical Hysterectomy
Shortcomings of laparoscopy include only four degrees of motion, rigid instruments, and reduced depth perception. There is increasing evidence supporting the use of robotic surgery for radical hysterectomy, which allows for a full seven degrees of motion, employs 3D vision, and reduces tremor through motion-dampening controls. Drawbacks include cost (approximately $1.5 million for the da Vinci® robot [Sunnyvale, California]), loss of tactile feedback, large bulky arms with long positioning times, and the requirement of a large, well-trained operating room staff.
Technique
Informed consent is obtained. All patients undergo pre-operative bowel preparation and receive prophylactic antibiotics. After placement in the lithotomy position with the arms out to the sides, a Foley catheter is inserted. A V-care® uterine manipulator (ConMed, Utica, New York) is placed. Under direct visualization, a 12mm bladeless trocar is placed 3cm above the umbilicus. A second 12mm bladeless trocar is then placed above and 8cm to the left of the first trocar, and is used by the assistant. The abdomen is then insufflated, and the patient is placed in steep Trendelenburg position. Three additional robotic trocars are then placed: one 15° below and 8cm to the left of the assistant trocar, another 8cm to the right of the umbilical trocar, and a third 8cm to the right and 15° below the second robotic trocar. The robot is then docked, as are the camera and robotic arms. The steps for the RRH are subsequently the same as described for the laparoscopic approach.
Outcomes
Sert and Abeler9 were the first to describe the robotic technique for radical hysterectomy in cervical cancer. Since then, a number of investigators have published larger studies comparing robotic versus abdominal and laparoscopic radical hysterectomy (see Table 2). Boggess et al.10 examined 51 patients with early-stage cervical cancer who underwent RRH compared with 49 historic controls who underwent ARH. Patients who underwent RRH had a much lower EBL (96.5 versus 417cc; p<0.0001), and there was a higher lymph-node yield (33.8 versus 23.3; p<0.0001). There were significantly fewer complications in the RRH group, and hospital stay was only one day (versus 3.2 in the ARH group). Operative time was actually shorter in the RRH group (211 minutes versus 250 minutes). Recently, Nezhat et al.11 compared 30 patients who underwent TLRH with 13 who underwent RRH, and found no difference in operative times, EBL, or hospital stay. No cases were converted to open procedures, and no patients recurred.
Magrina et al.12 have published the only account comparing RRH, TLRH, and ARH. They found mean operating times were 190, 220, and 167 minutes, EBL was 133, 208, and 444cc, and mean length of stay was 1.7, 2.4, and 3.6 days, respectively. There were no conversions to open procedures in the laparoscopic or robotic groups, and there were no differences in intra-operative or long-term complications between all three groups. A multi institutional trial15 based at MD Anderson Cancer Center has recently opened for accrual in which patients with early-stage cervical cancer will be randomized to radical hysterectomy through laparotomy versus minimally invasive surgery (laparoscopy or robotics).
Conclusion
Total laparoscopic hysterectomy for early-stage cervical cancer has several advantages over abdominal hysterectomy: less blood loss, fewer complications, improved cosmesis, and a shorter hospital stay. Therefore, it is both a safe and a feasible procedure. Robotic surgery may surpass both laparoscopy and laparotomy for radical hysterectomy, and we look forward to the results of larger trials comparing these modalities.■