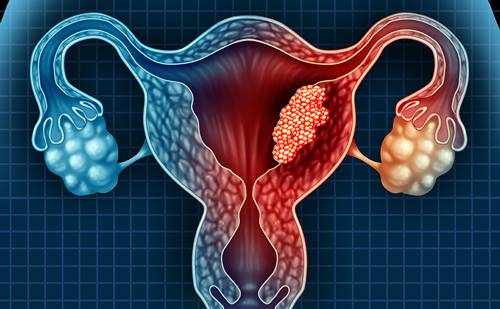
Endometrial carcinoma is the fourth most common female cancer and the most common malignancy of the female reproductive tract.1 Adenocarcinomas arise from the uterine epithelium and constitute 90% of endometrial cancers. The remaining histological types of endometrial carcinoma include adenocarcinoma with squamous differentiation, adenosquamous carcinoma, clear cell carcinoma and papillary serous carcinoma. Serous papillary carcinoma behaves like ovarian cancer and hence has a worse prognosis compared with grade 1 and 2 endometrial adenocarcinoma. Endometrial cancer primarily presents at stage I (80% of cases) and the standard treatment is either laparoscopic hysterectomy or total abdominal hysterectomy and bilateral salpingooophorectomy. The prognosis for endometrial carcinoma depends on a number of factors, including stage, depth of myometrial invasion,lymphovascular invasion, nodal status and histological grade. Determination of the depth of myometrial invasion is important, since it correlates with the incidence of lymph node metastases. Pre-operative evaluation of prognostic factors helps in sub-specialist treatment planning. Although endometrial carcinomas are typically diagnosed at endometrial biopsy, imaging fulfils an important role in both the assessment and staging of these patients.
Role of Ultrasound
The main role of transvaginal ultrasound (TVS) is the accurate assessment of endometrial thickness in patients presenting with postmenopausal bleeding. Ultrasound is widely available, does not involve the use of ionising radiation and has a high negative predictive value, facilitating the assessment of post-menopausal patients into high- and low-risk groups. Ultrasound has a high sensitivity in assessing whether the endometrium is abnormal but a low specificity because benign conditions can also cause a thickened endometrium.2 Usually, a normal post-menopausal endometrium is atrophic, measuring less than 5mm in thickness and appearing as a thin echogenic line. Endometrial thickness must be assessed on TVS by measuring the two opposing endometrial layers in the sagittal plane, excluding endometrial fluid in the measurement. Endometrial cancer appears as non-specific thickening of the endometrium that is difficult to distinguish from hyperplasia or a polyp, unless myometrial invasion is present. The diagnosis of endometrial cancer is then usually established on the basis of endometrial biopsy or curettage, often undertaken at the time of hysteroscopy. Colour and pulsed Doppler improves diagnostic accuracy as most endometrial carcinomas have abnormal blood flow with intratumoural or peritumoural blood vessels. Endometrial carcinoma can be associated with low impedance flow, both in the intramyometrial arteries and in the uterine arteries. Hysterosonography is a rarely used technique that has been shown to improve the sensitivity3 and specificity4 of ultrasound examination. It involves the instillation of normal saline via a small catheter under TVS and therefore distends the endometrial cavity with fluid. This helps in identifying whether there is an intracavitary lesion, such as endometrial polyp, causing thickening or whether there is a subendometrial cause, such as leiomyoma. In patients with endometrial carcinoma, the endometrial cavity cannot be easily distended and there is irregular thickening of the endometrium.4 Although ultrasound is excellent at assessing the thickness of the endometrium, staging of endometrial carcinoma once histological diagnosis has been made is better served by other imaging modalities, especially magnetic resonance imaging (MRI). The main role of ultrasound is to gain an accurate assessment of endometrial thickness with TVS in patients presenting with post-menopausal bleeding.
To read full article please click here