Follicular lymphoma (FL) is the second most common subtype of non-Hodgkin lymphoma worldwide in adults (~20–25%). The origin of FL cells is follicle centre B lymphocytes. In the majority of patients the disease is diagnosed in advanced stages III/IV (~80%). For asymptomatic patients, watchful waiting may be appropriate since deferred therapy tested in three randomised trials showed no detrimental effect on cause-specific or overall survival (OS)1–3 and a substantial rate of spontaneous regression has been reported.4 In case of symptomatic disease, patients require systemic therapy. The exploration of different chemotherapy regimens that provide initially high response rates (75–90%)5–7did not lead to a significant improvement of long-term prognosis. The median survival time was over three decades in a range between eight and 10 years.8 More recently, a significant prolongation of overall survival was reported due to the introduction of novel therapeutic strategies such as chemoimmunotherapy, radioimmunotherapy and use of autologous/allogeneic haematopoietic stem cell transplantation. This article will discuss the different treatment approaches, addressing the issues of current first-line and salvage strategies in patients with advanced-stage FL.
First-line Treatment Strategies in Advanced-stage Follicular Lymphoma
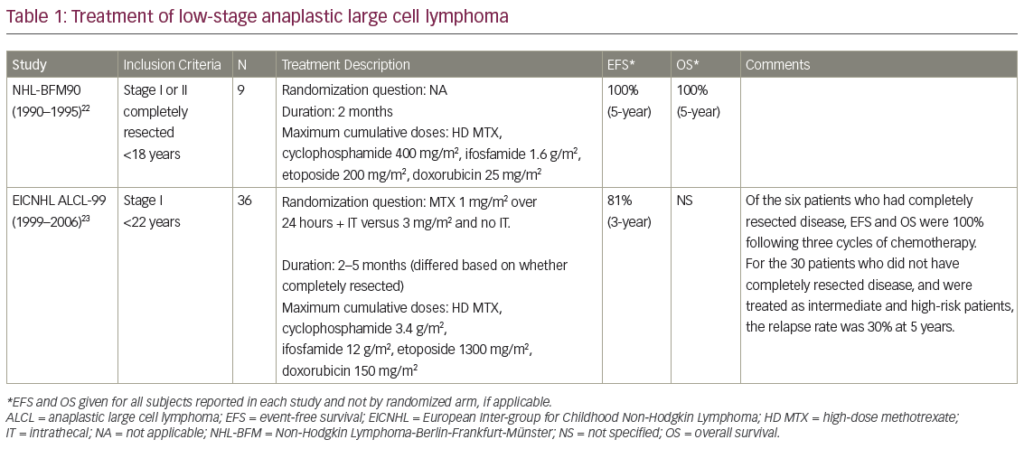
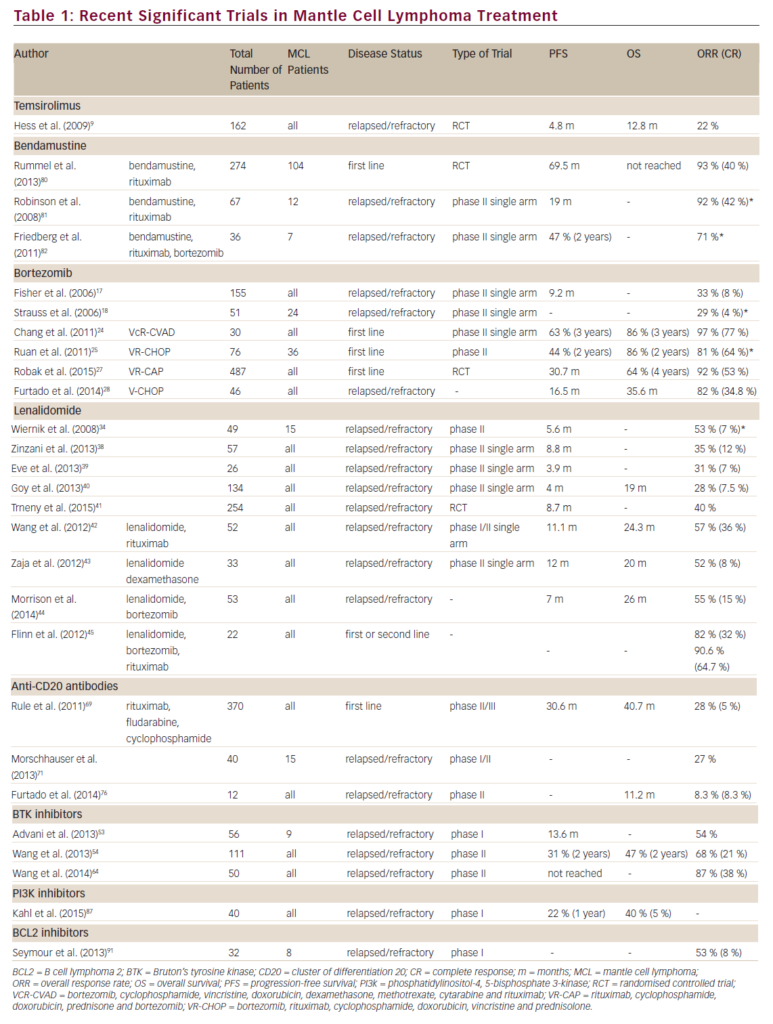
In recent years, promising first-line treatment approaches have been developed in patients with advanced-stage FL. The implementation of the monoclonal anti-CD20 antibody rituximab has demonstrated efficacy with an excellent toxicity profile. Binding of rituximab to the CD20 surface antigen, which is expressed by more than 90% of follicular lymphoma cells, leads to complement-mediated lysis and cell-mediated cytotoxicity and induces apoptosis. Rituximab has been successfully applied as a single agent9,10 and in combination with different chemotherapy regimens (chemoimmunotherapy). Chemoimmunotherapy enhanced response rates and significantly improved progression-free survival (PFS) and overall survival (OS) when compared with chemotherapy alone (see Table 1).11–15
In order to prevent relapses, the concept of rituximab maintenance therapy following first-line induction with various chemoimmunotherapy regimens is currently under evaluation in international phase III randomised trials such as the Primary Rituximab Maintenance (PRIMA) study. The first interim analysis of the PRIMA study compared two years of rituximab maintenance therapy versus observation in FL patients responding to first-line immunochemotherapy with either eight cycles of rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone (R CHOP) (75%), rituximab, cyclophosphamide, vincristine and prednisone (R-CVP) (22%) or rituximab, fludarabine, cyclophosphamide and mitoxantrone (R-FCM) (3%). After a median follow-up of 25 months, the PRIMA study demonstrated a significant improvement of two-year PFS (rituximab maintenance 82% versus observation 66%; p<0.0001) with little additional toxicity (neutropenia 4 versus 1%; infections 4 versus 1%) and indicated that maintenance therapy with rituximab may become a new standard of care for the first-line treatment of patients with advanced FL.16 In the era before rituximab, interferon-α (IFN-α) maintenance therapy was also shown to prolong remission duration and OS,17 but poor tolerance has prevented its widespread use.
In recent years, radiolabelled anti-CD20 antibodies (complexing radioisotope to a monoclonal anti-CD20 antibody) have been evaluated with regard to their ability to potentiate the direct cytotoxic effect of rituximab.18 The efficacy and safety of sup>90Y-ibritumomab tiuxetan and 131I-tositumomab have been analysed as single-agent therapy and as part of multimodality treatment regimens, resulting in convincing high response/OS/PFS rates (see Table 2). Toxicities were manageable and comprised haematological (e.g. neutropenia, thrombocytopenia) and non-haematological (e.g. asthenia, nausea, fever and rash) side effects.19–24 A recent phase III trial (first-line indolent trial [FIT]) evaluated the potential effect of consolidation90Y-ibritumomab tiuxetan therapy in responders of different induction chemotherapy regimens (~15% rituximab-based).90Y-ibritumomab tiuxetan therapy significantly prolonged median PFS in all patients (36.5 versus 13.3 months), regardless of the response rate (complete response [CR] 53.5 versus 29.5 months; partial response [PR] 29.3 versus 6.2 months) and yielded high PR-to-CR conversion rates. Interestingly, in the subgroup of patients who received rituximabbased induction chemotherapy, PFS was not different between treatment arms.25
To exploit the comparably high intrinsic chemosensitivity of lymphoma cells early in the course of the disease, the efficacy and safety of high-dose therapy followed by autologous haematopoietic stem cell transplantation (HSCT) has been investigated in five European randomised phase III trials (see Table 3).26–30 Despite the fact that follow-up times varied markedly from about four to nine years, all five randomised trials showed a significant improvement of PFS in patients treated with autologous HSCT (autologous HSCT ~60% versus standard chemotherapy 30%). However, no OS benefit could be demonstrated for patients undergoing autologous HSCT as consolidation therapy in first remission compared with conventional treatment approaches.
Moreover, it should be taken into account that most studies were initiated in the era before rituximab, so that the control arm was not optimal from a current point of view. Therefore, the prognostic relevance of autologous HSCT compared with current chemoimmunotherapy is being evaluated in a phase III trial by the German Low-grade Lymphoma Study Group (GLSG): after induction treatment with six cycles of CHOP/R-CHOP, responding patients <60 years of age underwent a second randomisation for autologous HSCT or to interferon-α maintenance. After a median follow-up of 58 months, a significant improvement of response duration was only documented in the patient group not treated with autologous HSCT.15 Interestingly, a small prospective phase II trial (n=31 patients with FL or mantle cell lymphoma) provided evidence for a potential effect of post-autologous HSCT rituximab maintenance. One single course of rituximab helped to prevent relapses by the elimination of minimal residual disease approved by PCR analysis and may translate into improved event-free survival (EFS).31
To date, chemoimmunotherapy alone has not yet been compared in randomised trials with the promising option of consolidation radioimmunotherapy. In order to evaluate the best first-line treatment in patients with FL, the US Intergroup trial compared R-CHOP with CHOP followed by 131I-tositumomab in a randomised phase III trial that closed in 2009. In summary, in symptomatic patients, chemoimmunotherapy is the current treatment of choice based on five randomised trials with no consensus on the best chemotherapy arm.11–15 In a randomised phase III study R-bendamustin (R-B) appeared to be superior to R-CHOP with regard to CR rate (40 versus 30%) and EFS (54.8 versus 34.8 months). In addition, the bendamustin arm provided a significantly better toxicity/tolerability profile.32
Salvage Treatment Strategies in Relapsed/Refractory Follicular Lymphoma
In patients with relapsed or recurrent FL, conventional chemotherapy is unable to induce a permanent second remission. The median survival of these patients is in the range of four to five years from first relapse.33 Therefore, different approaches for second-line treatment have been evaluated: chemoimmunotherapy, radioimmunotherapy, autologous and allogeneic HSCT.
The concept of chemoimmunotherapy has been evaluated both in rituximab-naïve and rituximab-pre-treated patients. A clear benefit in terms of remission induction, PFS and OS and an additional advantage of maintenance rituximab treatment could be observed when compared with chemotherapy alone.34,35
The implementation of radioimmunotherapy in relapsed/refractory FL produces convincing overall response rates (ORR) ranging from 73 to 83% with tolerable toxicity.36–40 In a randomised trial, radioimmunotherapy with 90Y-ibritumomab tiuxetan produced a statistically and clinically significant higher ORR and CR compared with rituximab alone,37 and a trend towards longer time to progression (15 versus 10.2 months), duration of response (16.7 versus 11.2 months) and time to next therapy (21.1 versus 13.8 months).39 Moreover, a single dose of 90Y-ibritumomab tiuxetan can produce durable responses and prolonged survival in a substantial number of patients in whom previous therapies have failed.41
Several phase II studies indicated a potential OS/disease-free survival (DFS) benefit of autologous HSCT compared with conventional chemotherapy in patients with recurrent FL.42–47 However, only one multicentre randomised phase III study (the chemotherapy/unpurged autologous/purged autologous [CUP] trial) assessed the role of autologous HSCT in patients with relapsed FL. The results showed a prolonged two-year PFS/four-year OS after autologous HSCT. However, a small patient number (n=89) being randomised to a three-arm study design and short follow-up compromise the reliability of these data.48 In addition, this trial was performed before the introduction of chemoimmunotherapy regimens, which are now considered to be the treatment of choice in the salvage situation.35 The data for the use of autologous HSCT are conflicting. In a recently published retrospective analysis of 246 patients who relapsed or had disease progression after initial treatment in the Groupe d’Etude des Lymphomas de l’Adulte (GELA) prospective/randomised trials,28,47 a salvage regimen containing rituximab with subsequent autologous HSCT led to a dramatic improvement of five-year DFS/OS.49 In contrast, two retrospective analyses and one randomised study found no significant differences in survival outcomes in FL patients receiving pre-HSCT rituximab versus no rituximab.50–52
Since cure of advanced FL by chemo-, radioimmunotherapy and autologous HSCT has not yet been established, there is an increasing interest in exploring the role of allogeneic HSCT. As opposed to autologous HSCT, the allogeneic stem cell source provides a progenitor pool free of contaminated tumour cells and adds T-cells promoting a graft versus lymphoma (GvL) effect as part of an alloreactive mechanism.53,54 In this context, the inclusion of total body irradiation (TBI) in the conditioning regimen prior to allogeneic HSCT55–59 has some major advantages. TBI is efficient in order to eradicate malignant clonogeneic cells (median: ~105 log level), to achieve a sufficient immunosuppression and to enable engraftment of bone marrow/peripheral-blood-derived stem cells.60 In contrast to chemotherapy, TBI is able to reach liquor spaces and inadequately perfused tissues without any limitations. Since even in situations of CR ~107 clonogeneic stem cells may persist, TBI is routinely combined with high doses of chemotherapy drugs. However, there are not yet any randomised trials comparing chemotherapy-alone-based conditioning with TBI-based conditioning concepts in patients with FL. The first series of successful allogeneic transplantations in patients with relapsed/chemorefractory FL were published in the mid-1990s predominantly using a TBI-based conventional myeloablative conditioning protocol.61 In multivariate analyses the use of TBI was associated with better survival62 and decreased recurrence rates but with higher treatment-related mortality (TRM), mainly due to pulmonary complications (e.g. pneumonitis) compared with chemotherapy-alonebased conditioning protocols.63 Up to date, the value of conventional myeloablative allogeneic HSCT in patients with relapsed/ refractory FL was extensively evaluated. (see Table 4 ).54,61–74These data show that this treatment modality may have the potential for cure in relapsed/refractory FL, shown by low recurrence rates after transplant (0–25%), although long-term followup data for allogeneic HSCT are still pending. However, the high TRM (20–40%) due to fatal graft versus host disease (GvHD) and infection is still a matter for concern with this type of transplantation, limiting its use to patients <50 years of age. Chemotherapy-alone-based conditioning, poor performance status, chemorefractory disease and age >40 years of age were predictors for worse outcome.63,75
In order to extend the applicability of allogeneic HSCT for patients with advanced age and co-morbidities, reduced intensity conditioning (RIC) protocols were developed with the intent to decrease TRM while preserving GvL effects.76–79 RIC initially results in mixed chimaerism, which can be transformed to complete donor chimaerism by donor lymphocyte infusions applied several months after transplantation. RIC protocols are generally ludarabine-based and often include low-dose TBI or alkylating agents. The majority of studies confirm high DFS/OS rates after RIC HSCT (see Table 5).71,74,80–90 Despite the fact that some studies report similar TRM74,85,88,90 and a significantly enhanced risk of relapse after RIC compared with myeloablative HSCT in multivariate analyses,71 the practice of allogeneic transplantation has shifted in favour of RIC conditioning, representing ~80% of allogeneic transplants in 2002.71 Recently, new, mainly treosulphan-based, myeloablative conditioning protocols with reduced toxicity were developed in an effort to combine the advantages of myeloablative and RIC.91,92
The Role of External Beam Radiotherapy as Consolidation Therapy in Advanced Follicular Lymphoma
Since FL is considered to be one of the most radiosensitive tumours,93–95 the role of radiotherapy (RT) as consolidation treatment of regions with bulky disease after completion of chemotherapy has been investigated. In the pre-rituximab era after a median follow-up of 13.6 years, the use of consolidation RT (30–40 Gray [Gy]) after chemotherapy induction significantly enhanced DFS/OS rates compared with chemotherapy alone (68/89 versus 41/71%) in the first-line treatment of patients with bulky stage III/IV FL, possibly implying cure in selected patients.96 Currently, the role of RT has to be redefined since chemotherapy and radioimmunotherapy lead to substantially improved PFS/OS rates with tolerable toxicity. Strategies for adequate selection of patients who may benefit from consolidation RT are still pending. Palliative Role of External Beam Radiotherapy in Advanced Follicular Lymphoma
Patients with advanced FL may occasionally develop localised lesions such as spinal cord compression, painful splenomegaly and compression of vital organs by lymphoma masses. In this regard, involved-field RT is used with the intent of palliating symptomatic areas of disease. Even in patients with chemorefractory disease, low-dose involved-field RT (4Gy given in two fractions) is able to provide a fast and long-lasting response with minimal side effects in a considerable number of patients.97–102 This phenomenon may be explained by the predominance of apoptotic cell death in irradiated lymphoma cells.103 A further advantage of the low-dose strategy is the fact that it does not compromise the use of full-dose RT in a second-line treatment. In case of failure of low-dose RT, full-dose involved-field RT (30–40Gy) plays a major role in providing symptom relief and local control.104,105
Currently, non-toxic involved-field RT (two times 2Gy) is being compared with standard chlorambucil chemotherapy in the randomised phase III Hovon 47/European Organisation for Research and Treatment of Cancer (EORTC) trial.106
Conclusion
symptomatic patients can be managed expectantly in advanced FL. In symptomatic stages of FL, use of chemoimmunotherapy is the current first-line treatment of choice based on several randomised trials, with a significant impact on response rates, longer durations of response and improved PFS/OS compared with chemotherapy alone. The exact role of (consolidation) radioimmunotherapy has yet to be defined by ongoing trials.
In elderly patients with relevant co-morbidities, single-agent rituximab ± monochemotherapy or low-dose involved-field radiotherapy are suitable. In case of symptomatic relapse, chemoimmunotherapy followed by rituximab maintenance is widely used. For younger patients suitable for transplantation, high-dose therapy followed by autologous HSCT can be offered in chemoresponsive relapsed disease in order to prolong PFS and potentially OS. In case of relapse after autologous HSCT or chemoresistant disease, allogeneic HSCT may provide a curative treatment option for selected patients. However, despite advances in supportive care and better patient selection resulting in improved long-term OS/DFS, conventional allogeneic HSCT is restricted to younger patients with good performance status. Use of RIC yields a similar cure rate with lower TRM, counterbalanced by higher relapse rates when compared with conventional conditioning.
To date, the best pre-transplant conditioning regimens remain to be defined by prospective trials. The role of radiotherapy as additional local treatment in high-risk situations like bulky disease and/or incomplete morphological remission is poorly defined with regard to newly developed systemic treatment strategies.
A major challenge for the future will be the development of reliable tools for patient selection to the diversity of different treatment approaches available. ■