The past decade has witnessed tremendous progress in oncology. In lymphoma, methods such as gene expression profiling have led to the identification of exciting new targets for drug discovery. The most important advance of this decade has been the introduction of the anti- CD20 antibody rituximab. The addition of rituximab to cyclophosphamide, hydroxydaunorubicin (aka doxorubicin), Oncovin® (aka vincristine), and prednisone (CHOP) chemotherapy for diffuse large B-cell lymphoma (DLBCL) has improved the long-term survival rate from 9 to 13%.1,2 In addition, rituximab has become a mainstay in the treatment of indolent B-cell non-Hodgkin’s lymphoma (NHL), either alone or in combination with chemotherapy.
Since the astounding success of rituximab, the development of new antibodies for the treatment of lymphoma has become the main focus of drug development. One area of interest is in creating a fully humanized version of an anti-CD20 antibody. Putatively, humanization would lead to fewer infusion reactions, allowing for the more rapid infusion of the drug. Also, a fully humanized molecule may better initiate antibody-dependent cellular cytotoxicity and enhance the efficacy of the drug. Finally, the humanized antibody may recognize a different epitope on CD20, theoretically overcoming one mechanism of rituximab resistance— downregulation or alteration of CD20.3 In one trial of relapsed/refractory chronic lymphocytic leukemia (CLL), 12 of 26 patients (43%) responded to the humanized anti-CD20 antibody ofatumumab.4 Ofatumumab and other humanized anti-CD20 antibodies are now in clinical trials targeting, in particular, patients with follicular lymphoma and chronic lymphocytic leukemia who are rituximab -refractory.
A variety of antigenic targets besides CD20 are now also being pursued. Galiximab is an immunoglobulin (Ig)-G1 antibody that binds to CD80, a costimulatory molecule expressed on B cells that is involved in T-cell activation.5 A phase I/II trial of galiximab in combination with rituximab in patients with rituximab -sensitive follicular lymphoma demonstrated an overall response rate of 66% (19% complete response (CR), 14% unconfirmed (u) CR, and 33% partial response (PR)) in the group of patients treated at the highest dose level (500mg/m2).6 Co-administration of the two antibodies did not appear to affect the pharmacokinetics of either. An ongoing trial is studying rituximab with or without galiximab in patients with rituximab-sensitive follicular lymphoma. Another target is CD40, a member of the tumor necrosis factor receptor family that is expressed on B cells. A recent phase I trial of the humanized anti-CD40 antibody SGN-40 demonstrated a response rate of 37.5%, including one CR, in relapsed/ refractory DLBCL.7 Responses were also seen in mantle cell lymphoma and marginal zone lymphoma. A larger phase II trial in DLBCL is imminent. Lumiliximab is an antibody with human IgG1 constant regions and macaque variable regions targeting CD23. In a phase I/II study of lumiliximab in combination with fludarabine, cyclophosphamide, and rituximab (FCR) in CD23+ CLL, the overall response rate was 71% with 48% CR, 10% PR, and 13% uPR.8 Toxicity did not appear to differ substantially from that historically observed with FCR alone. A large international randomized trial comparing FCR with or without lumiliximab will be forthcoming. Epratuzumab, an antibody targeting CD22, has also demonstrated single-agent activity as well as activity in combination with chemotherapy and/or rituximab in a variety of lymphomas, most notably follicular lymphoma.9 For instance, in a phase I/II trial 24% of follicular lymphoma patients responded to single-agent epratuzumab.10 Trials of this agent in combination with other chemotherapies and other antibodies are ongoing. At present, monoclonal antibody combinations appear to be safe. In the future, combinations of antibodies analogous to combinations of chemotherapeutics may emerge as the standard for treating, in particular, low-grade lymphomas.
Other promising therapies continue to emerge beyond the realm of monoclonal antibodies. The following list is not exhaustive, but is merely a sampling of some of the more promising emerging agents. Protein kinase C beta (PKCβ) is a serine/threonine kinase associated with poor outcome in DLBCL.11,12 Enzastaurin is an oral drug that selectively inhibits PKCβ. In a phase II study of 55 patients with relapsed/refractory DLBCL, three patients experienced a CR and eight patients remained free from progression for four cycles.13 Although the overall response rate was not tremendously high, this was a heavily pre-treated group of patients and occasional dramatic responses were observed. The drug was also well tolerated, with grade III toxicities including fatigue, edema, headache, motor neuropathy (one patient), and thrombocytopenia, with no grade III or IV neutropenia. Due to the small—but real—CR rate, oral administration, and favorable toxicity profile, it is reasonable to study the drug further. An ongoing randomized phase III trial is examining the effect of enzastaurin consolidation in patients with DLBCL and an International Prognostic Index (IPI) score of three or greater who achieve a CR/uCR after rituximab–CHOP. Perhaps introducing the drug in the up-front setting in patients with debulked disease will decrease relapses and improve survival. Expression of B-cell lymphoma 2 (Bcl-2) protein is associated with chemotherapy resistance and decreased survival in B-cell malignancies. The antisense oligonucleotide oblimersen, designed to downregulate Bcl-2 messenger (m)-RNA, demonstrated marginal activity in combination with fludarabine and cyclophosphamide in CLL.14 The drug was further complicated by the need for seven-day continuous infusion. The US Food and Drug Administration (FDA) did not approve oblimersen based on a perceived lack of sufficient efficacy. A new small-molecule oral inhibitor of Bcl-2, ABT-263, is now entering phase I/II clinical trials in B-cell malignancies and will hopefully offer better efficacy and easier administration than oblimersen.
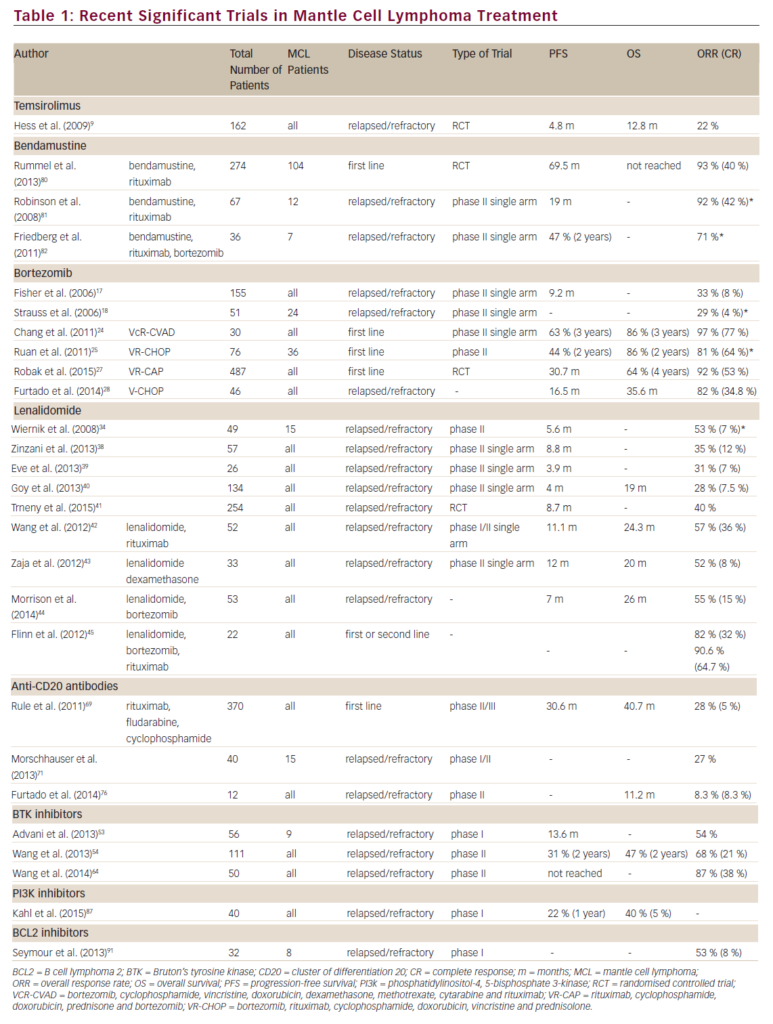
Lenalidomide is commercially available for the treatment of myelodysplastic syndrome and multiple myeloma. There is also an increasing body of evidence to suggest that lenalidomide will be effective in lymphoid malignancies. In a study of 45 patients with CLL, 51% of whom were refractory to fludarabine, the overall response rate with lenalidomide was 47%, with 9% CR.15 Such responses have been replicated in other trials.16 In a phase I trial of lenalidomide in mantle cell lymphoma (MCL), five of six patients treated at the maximal tolerated dose of 20mg on days one to 21 of a 28-day cycle achieved responses, including one CR, one PR, and three minor responses.17 A phase II trial in MCL is now ongoing. In a phase II trial of 50 patients with relapsed/ refractory aggressive B-cell NHL treated with lenalidomide 25mg by mouth during days one to 21 of a 28-day cycle, 14 patients (34%) exhibited an objective response (five uCR and nine PR) and 12 had stable disease (SD) for a tumor-control rate of 63%.18 Finally, in a study of 43 patients (27 evaluable) with relapsed/refractory indolent B-cell NHL, seven patients (26%) exhibited an objective response (two CR, one uCR, and four PR, and nine had SD for a tumor-control rate of 59%).19 The primary toxicity of lenalidomide in these studies has been myelosuppression, although venous thromboembolic events remain a concern. Confirmatory trials of lenalidomide alone or in combination with other agents are being conducted in all of the histologies listed above. T-cell lymphoma comprises a wide variety of diseases, which as a whole account for approximately 10–15% of all cases of NHL. In general, T-cell NHLs are less responsive to chemotherapy and have a poorer prognosis than B-cell NHL. Until recently, there was a paucity of new drug development for T-cell malignancies, but this has slowly yet steadily started to change. One of the most promising emerging agents for the treatment of T-cell NHL is the novel folate antagonist pralatrexate (PXD008). Pralatrexate is a rationally designed drug that is a high-affinity substrate for the reduced folate carrier-1 (RFC-1). It provides effective active transport into many malignant cells, where it is polyglutamated by folylpolyglutamate synthetase (FPGS), with subsequent inhibition of dihydrofolate reductase.20 The drug has been studied quite extensively in lung cancer, but its most impressive activity is in T-cell lymphoma.
A report on the phase I/II experience of the first 24 patients with T-cell lymphoma treated with pralatrexate was presented at the American Society of Hematology (ASH) 2006 meeting.21 Of 24 patients, four were too early to assess and four were removed from trial after only one or two doses due to side effects or concomitant medical concerns. Of the remaining 16 patients who had completed at least two cycles of therapy, 10 patients had major responses, including nine CR and one PR, with an overall response rate of 63%. Even by intent-to-treat analysis the overall response rate was 50%. The authors reported on one patient with relapsed human T-cell lymphotropic virus (HTLV-1)-associated adult T-cell leukemia/lymphoma who has been on the drug and in sustained remission for over 18 months. In general, the toxicity profile is excellent, with thrombocytopenia and grade I–II mucositis being most common. Two life-threatening infections occurred. Unfortunately, the response rate in B-cell malignancies was not as encouraging. Of six patients with Hodgkin’s disease, one case of stable disease was demonstrated. Of 18 patients with B-cell NHL, only one partial response was seen. Currently, the drug is being tested in an international, open-label phase II trial in T-cell NHL, which could lead to regulatory approval if the response and safety data remain promising.
As mentioned above, antibody therapy has become established as a cornerstone of therapy in B-cell NHL. Although such therapy has not been as prevalent in T-cell NHL, there have been several interesting new developments. The humanized anti-CD4 antibody zanolimumab has been tested in two trials of patients with refractory cutaneous T-cell lymphoma.22 Dose ranges were 280, 560, and 980mg, all given weekly for 17 doses. In the lowest dose arm the response rate in mycosis fungoides was only 15%, but at the higher doses the overall response rate was 56%. Toxicity was mild and mostly limited to minor infections of the skin and upper respiratory tract, infusion reactions, and eczematous dermatitis. As predicted, transient depletion of CD4 cells was observed. Currently, a pivotal trial is under way to confirm these findings, but the preliminary data suggest that this agent would be useful in treating cutaneous T-cell lymphoma (CTCL).
Zanolimumab has also been studied in patients with relapsed/refractory peripheral T-cell lymphoma. Of 15 patients treated with zanolimumab 980mg weekly, two patients experienced uCR, two patients PR, and two patients had stable disease.23 Four serious adverse events were attributed to the study drug, including febrile neutropenia, thrombocytopenia (an infusion-related reaction), and hyperthermia with hypotension. The response rate with this agent in heavily pre-treated peripheral T-cell lymphomas is similar to what one would expect with single-agent rituximab in heavily pre-treated B-cell NHL. The results of this trial justify further study of the drug. A combination of zanolimumab with chemotherapy would be a particularly attractive study.
Denileukin diftitox is not a monoclonal antibody, but rather a fusion protein of interleukin (IL)-2 and diphtheria toxin. T-cell lymphomas exhibit increased expressions of intermediate- and high-affinity IL-2 receptor. Therefore, the IL-2 component of denileukin diftitox serves as a homing device, delivering the drug to the lymphoma cell where it is endocytosed and the diphtheria toxin is cleaved from the parent compound. The toxin then inhibits protein synthesis and kills the cell. Although the drug is FDA-approved for the treatment of relapsed CTCL, it is being studied in peripheral T-cell lymphoma at present. An ongoing trial is examining the efficacy of administering denileukin diftitox in combination with CHOP as the initial treatment of peripheral T cell lymphomas. The trial is still accruing patients, but a preliminary report suggests that the combination is well tolerated and has promising efficacy.24
Autologous stem cell transplantation is a cornerstone of therapy in many types of B- and T-cell NHL, particularly in patients who have relapsed. Although current stem cell mobilization strategies are effective, a new drug has the potential to increase the number of patients able to undergo peripheral stem cell mobilization and improve the quality of the product obtained. AMD3100 is an inhibitor of CXCR-4 that blocks the interaction of CD34+ stem cells with stromal cell-derived factor-1 in the bone marrow stroma, resulting in increased numbers of circulating CD34-positive stem cells.25 In a study of 25 patients with NHL and multiple myeloma, patients were sequentially mobilized with AMD3100 plus granulocyte colony-stimulating factor (GCSF) and GCSF alone, with each patient serving as his or her own internal control.26 Some patients were mobilized with GCSF first then AMD3100 plus GCSF, while the sequence was reversed in the remainder of the patients. Patients with multiple myeloma mobilized a median of 3- to 3.5-fold more CD34 cells per day of apheresis with the addition of AMD3100 to GCSF. Similarly, patients with NHL mobilized a median of 4.4-fold more cells per day of apheresis with the addition of AMD3100. These findings are being confirmed in separate randomized trials of GCSF±AMD3100 in patients with NHL and multiple myeloma. The results of both trials should be available soon. The greatest potential advantage of AMD3100 may not be merely to increase the number of patients who can be successfully transplanted or successfully undergo peripheral stem cell collection, but rather to increase stem cell yield and increase the number of patients achieving the ideal stem cell yield of >5×106 CD34+ cells/kg, leading to more rapid engraftment and decreased morbidity from autologous transplantation, including fewer infections, as well as fewer transfusions, hospital days, and apheresis sessions.
This discussion covered only a few of the new agents in development for lymphoid malignancies. The greatest challenge moving forward, in addition to developing new agents, is incorporating the increasing number of effective therapies into a rational treatment regimen. Clearly, administering a multitude of antibodies and chemotherapeutic agents to every patient will not be feasible. Thus, new modalities such as gene expression profiling that help us to predict which tumors will respond to the various therapies will be critical.