For high-risk soft-tissue sarcomas (HR-STS) in adults, new treatment strategies are needed to improve outcome with regard to local control and overall survival. Systemic chemotherapy has been integrated either after (adjuvant) or before (neoadjuvant) optimal local treatment by surgery and radiotherapy in HR-STS. This short article summarises the results of this combination with regional hyperthermia (RHT) as a targeted treatment strategy.
For high-risk soft-tissue sarcomas (HR-STS) in adults, new treatment strategies are needed to improve outcome with regard to local control and overall survival. Systemic chemotherapy has been integrated either after (adjuvant) or before (neoadjuvant) optimal local treatment by surgery and radiotherapy in HR-STS. This short article summarises the results of this combination with regional hyperthermia (RHT) as a targeted treatment strategy.
The optimal treatment for HR-STS in adults remains a challenge for the multidisciplinary approach in modern oncology. Patients with large primary or recurrent STS (>5cm in diameter, grade 2–3) remain at increased risk of distant metastases and tumour-related mortality. Nearly all deaths are due to metastatic disease (e.g. lung, liver). The tendency for early haematogenous spread of STS may explain why distant metastases still occur in these patients despite optimal local treatment. Also, the invasiveness or anatomical location of locally advanced tumours often prevents resection with adequate margins, and the toxicity of radiotherapy limits the use of potentially therapeutic doses with a negative impact on local control.
Innovative Treatment Strategy
With regard to prognostic factors, it can be concluded that for each histologically distinct sarcoma the tendency for metastatic spread depends on high-risk factors such as the grade, size and depth of the tumour.1,2 Therefore, treatment of STS is almost always multidisciplinary and should involve a team approach in order to optimise interaction between disciplines. Among the treatment modalities, surgery combined with radiation is of key importance, at least for local control. Although small, superficial and low-grade STS tumours may be managed by surgery alone, the vast majority of sarcoma patients do not have such tumours. For example, most of the localised deep trunk or retroperitoneal sarcomas present with large tumour size and invasive growth behaviour; therefore, adequate resection is often difficult or cannot be achieved with tumour-free margins. In addition, most patients with primary large and extracompartmental extremity HR-STS require multimodal treatment strategies to avoid amputation or mutilative surgery. Therefore, current clinical research goals include pre-operative treatment to control systemic microscopic disease and to ‘downsize’ the initial tumour mass in order to avoid amputation. In general, patients who can be rendered free of gross disease by one or multiple disciplines have an improved prognosis. Besides surgery, radiation and chemotherapy, new advanced technical developments such as RHT are of great interest and are already showing clinical potential in terms of treatment outcome based on results of recent trials. Another advantage compared with adjuvant post-operative treatment is the presence of an evaluable tumour, the clinical and pathohistological behaviour of which can provide valuable information about chemosensitivity during neoadjuvant treatment. In addition, before surgery or radiotherapy, drug delivery may be improved because the vascular supply of the tumour is undisturbed.
A recent article from Memorial-Sloan Kettering Cancer Center and the Dana Faber Cancer Institute compared patients with HR-STS tumours ≥5cm in diameter treated with only local therapy with those given neoadjuvant chemotherapy in addition to local therapy. In the subset of patients with tumours ≥10cm in diameter, three-year diseasespecific survival was 0.62 (95% confidence interval (CI) 0.53–0.71) for patients not receiving neoadjuvant chemotherapy and 0.83 (95% CI 0.72–0.95) for patients receiving neoadjuvant chemotherapy. In patients with tumours between 5 and 10cm in diameter, there was no difference in outcome.3
A programme of aggressive chemotherapy interdigitated with radiotherapy for patients with large, high-grade extremity sarcomas used as neoadjuvant chemotherapy mesna–doxorubicin–ifosfamide– dacarbazine (MAID) with split-course radiotherapy followed by resection and post-operative adjuvant MAID chemotherapy.4 On the basis of these data, the Radiation Therapy Oncology Group (RTOG) initiated a phase II trial to evaluate the efficacy and toxicity of a modified MAID regimen in similar patients in a multi-institutional setting. Efficacy results showed three-year rates for disease-free and overall survival of 56.5, 64.5 and 75.1%, respectively, but 83% of patients experienced grade 4 toxicities and another 5% fatal grade 5 toxicities.5
The only randomised trial of neoadjuvant chemotherapy for patients with resectable, high-risk sarcoma was performed by the European Organisation for Research and Treatment of Cancer (EORTC), but this trial was stopped because of low recruitment. Neoadjuvant treatment showed an objective response rate of 29%, but after a median follow-up of 7.3 years there was no statistically significant advantage in disease-free survival due to the lack of statistical power.6
Regional Hyperthermia Combined with Chemotherapy
The application of hyperthermia has been integrated into multimodal treatment strategies over the past 10–20 years. However, more recently designed applicators for controlled, superficial and deep heating under clinical conditions now allow clinicians to use hyperthermia combined with systemic chemotherapy or local radiotherapy as a matter of routine.7 The rationale for the combination of cytotoxic drugs with RHT (increase of tumour temperature in the range of 40–44°C) in the treatment of STS is based on experimental and clinical evidence suggesting that heat increases killing of tumour cells by direct thermal toxicity, as well as evidence of thermal enhancement of drug efficacy. In addition, pre-clinical results indicate that hyperthermia might be useful in modulating the immune system by inducing the expression and release of heat-shock proteins.8
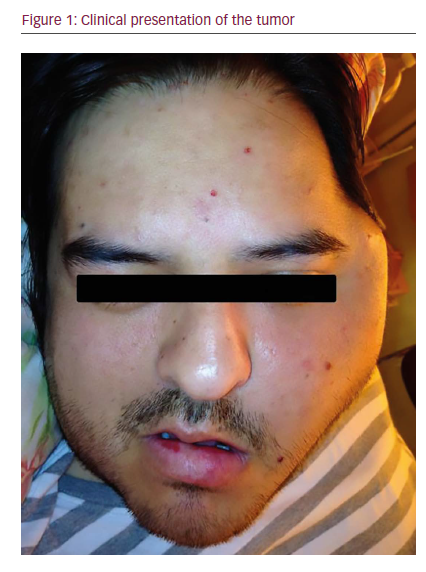
The sarcoma group at the Klinikum Grosshadern Medical Center (KGMC) has focused its interest on the use of RHT as a new treatment modality for locally advanced HR-STS. The first results were obtained from a phase II study in 38 adult patients, mainly with STS.9 These patients had relapsed after prior surgery and radiation and had not responded to previous chemotherapy alone. The local response rate was 37%. A drug combination of ifosfamide and etoposide (VP16) was used, combined with RHT as a second-line treatment. In addition to long-term tumour control in a subgroup of patients, the analysis of tumour temperatures (e.g. T20, T50, T90) achieved using an electromagnetic deep regional heating device (BSD Medical Corporation system; see Figure 1)10 showed significantly higher temperature parameters in responders compared with non-responders.
Two additional consecutive phase II studies have been performed including extremity and non-extremity HR-STS (chemo-naïve patients). In the first study (RHT-91 protocol), 59 patients received four cycles of etoposide–ifosfamide–doxorubicin (EIA) combined with concurrent hyperthermia. The aim was to achieve a maximum tumour temperature of 42°C or higher for a period of 60 minutes. After this treatment, those patients whose tumour was judged to be resectable underwent surgery. If the tumour showed signs of response, four additional cycles of combined chemotherapy and RHT were given. All patients not previously irradiated also received external-beam radiotherapy. Treatment-related toxicity was acceptable. The median survival was 52 months and the fiveyear survival rate was 49% (95% CI 36–61%) – values that are quite impressive in this group of patients. The data are in favour of patients responding to EIA combined with hyperthermia.11
In the second study (RHT-95), a similar high-risk patient group (54 patients) received the same treatment as in the RHT-91 protocol, with the exception that the patients did not receive post-operative hyperthermia but were administered with systemic chemotherapy alone after surgery. This study showed an inferior local failure-free survival rate compared with the RHT-91 protocol, but no difference was found in overall survival.12 Thus, post-surgical hyperthermia combined with chemotherapy was revealed to be critical for local control. In another retrospective analysis for retroperitoneal and visceral STS recruited to both studies, the RHT-91 and RHT-95 protocols demonstrated that the initial response to chemotherapy combined with RHT was predictive of long-term survival.13
Most recently, under the auspices of the EORTC and the European Society of Hyperthermic Oncology (ESHO), we were able to complete a randomised intergroup phase III trial (EORTC 62961/ESHO RHT-95) of multimodal treatment in patients with primary (S1 group) and recurrent (S2 group) disease or after inadequate surgery (S3 group: resections with positive margins or macroscopic residual tumour) in HR-STS (tumour size ≤5cm in diameter + histological grade of 2 or 3 + deep location + extracompartmental extension). In this trial, all patients with HR-STS to extremity and non-extremity received neoadjuvant systemic chemotherapy (four cycles of the EIA regimen) and were randomised to one of two arms – chemotherapy alone or combined with RHT – followed by definitive surgery and radiotherapy. Thereafter, in addition, four cycles of the EIA regimen were administered with or without RHT, according to the initial randomisation (see Figure 2). The first interim report showed promising results in terms of overall outcome for extremity and nonextremity STS.14
We also analysed the risk of early progression for the three-month duration of pre-operative therapy after recruitment of more than 250 patients. Delay of surgical resection due to this period of initial management is of major concern. A total of 213 patients were eligible for assessment of early progression. Fifteen of 213 patients (7%) progressed within the first three cycles of EIA with or without RHT. At the time of response evaluation after completion of four cycles of EIA ± RHT, an additional 18 of 213 patients (8%) showed progressive disease. One hundred and eighty of 213 patients (85%) showedstable disease or clinical objective response (four complete response, 33 partial response).15
After completion of the phase III trial with a total of 341 randomised patients, the first analysis in terms of objective response rate, local progression-free survival and disease-free survival was presented at the American Society of Clinical Oncology (ASCO) Meeting in June 2007.16 Nearly 90% of patients in the combined treatment group finished four cycles of chemotherapy, and 82% of patients assigned to the chemotherapy-alone group completed four cycles. Median followup was 24 months. Fourteen patients who received chemotherapy alone had a partial or complete tumour response compared with 40 in the experimental group (p<0.001). The median local progression-free survival rate was 37.7 months for patients receiving combination therapy and 26.2 months for patients in the single-modality arm (p<0.02). Disease-free survival was also in favour of the hyperthermia arm (p<0.01).
Conclusions
During the past decade, considerable progress has been made in the use of combined-modality treatment strategies. For example, preoperative radiochemotherapy in HR-STS has shown promising results in pilot studies in terms of local control or local progression-free survival, but is hampered by significant toxicity. Among others, the approach described here using RHT as targeted therapy combined with systemic chemotherapy within a pre- or post-operative strategy is a new effective treatment option associated with low toxicity. With this concept, in addition to the potential of RHT to increase the chemotherapeutic effect, surgery is still embedded as cornerstone treatment followed by radiotherapy for local tumour control. The results of the completed phase III intergroup study (EORTC 62961/ESHO RHT-95) have shown that the addition of RHT to this treatment strategy significantly improves outcome in patients with HR-STS. ■