The treatment of adult sarcomas stands in sharp contrast to childhood sarcomas. In the 1970s, the introduction of chemotherapy made a big difference in the prognosis of rhabdomyosarcoma, Ewing’s sarcoma and osteosarcoma, raising their cure rate from less than 20% to more than 60%.2 The chemosensitivity of adult STS is too low to have a similar effect on survival. Interestingly, the benefit seen in childhood sarcomas has largely been due to the introduction of chemotherapy itself, mainly based on a few active drugs, since subsequent improvements in chemotherapy have brought limited progress. Cytotoxic chemotherapy has made a prognostic difference in childhood sarcomas because these are chemosensitive, while it has not had any effect on adult STS because these are much less chemosensitive.
Doxorubicin was introduced into the treatment regime for STS in the 1970s, and ifosfamide followed in the 1980s. This led to combination regimens, the antitumour activity of which seemed higher than that of doxorubicin alone or doxorubicin-based combination regimens (e.g. cyclophosphamide, vincristine, doxorubicin and dacarbazine [CYVADIC]).
The benefit of these regimens was clearly shown by well conducted phase II studies;3 however, phase III randomised trials failed to confirm any survival benefits. The response rate for combination therapy was only marginally higher in two trials and equal in another compared with doxorubicin alone.4–6 Many factors may explain these results. The most important is probably the different patient selection criteria of phase II and III studies. The latter need a higher number of patients (thus these are less selected) and involve a higher number of centres. This probably dilutes any advantage of chemotherapy regimens, which would be limited in any case. The main proof of this is the lower response rate of phase III trials compared with phase II studies.
The patient populations enrolled by the two different kinds of study are evidently different. Conceptually, this leaves room for the possibility that there are some patients in advanced stages of the illness who may benefit from intense chemotherapy. Indeed, this is a possibility, although it is difficult to prove. For example, some patients have isolated lung metastases that are amenable to surgery, but also have unfavourable prognostic factors (e.g. a significant number of lesions). They may experience benefits from chemotherapy if an active regimen is administered. This is just a possibility, because there are no clinical trials addressing the issue. Indeed, a recent retrospective analysis does not suggest such a benefit for chemotherapy ‘adjuvant’ to surgery of lung metastases.7 However, there are hints that lung metastases may respond better than lesions to other sites, although this may be just a consequence of the fact that they are more amenable to being measured. With regard to extra-pulmonary metastases, there are patients with significant symptoms of their lesions. Clearly, a higher response rate will be more likely to result in a benefit in terms of quality of life, if not survival. Therefore, the clinical feeling may lead the physician to use a more or a less aggressive regimen from patient to patient in light of the lack of trials settling the issue. One should not forget that a fraction of patients with advanced STS, as small it may be, can become long-term survivors.8 This may be a matter of the natural history of the disease, or simply of tails of probability distributions, but certainly adds to the often good general conditions of advanced sarcoma patients in encouraging the medical oncologist to be relatively ‘aggressive’ in the advanced phase of STS. As a matter of fact, medical oncologists resort more frequently to chemotherapy in treating sarcomas than carcinomas, which are more likely to bring about a systemic deterioration of general conditions in the advanced stages of disease. It is true that such a policy hardly finds a strong background in terms of clinical trials, but on the other hand it is hard to believe that this practice lacks any clinical rationale. The authors believe that as STS are rare tumours, it has been more difficult to demonstrate benefits in advanced STS.
The use of chemotherapy in the adjuvant setting is even more problematic. A high number of randomised clinical trials have been performed over the last few decades. Fourteen randomised clinical trials comparing a doxorubicin-based adjuvant chemotherapy with a no-chemotherapy arm after surgery were pooled in a meta-analysis, published in 1997.9 A total of 1,568 patients were included. An absolute relapse-free advantage in the 10% range was found overall, along with a lower overall survival improvement, which was not statistically significant.
A new meta-analysis has recently been reported, encompassing 1,953 patients enrolled into 18 trials.10 The magnitude of the benefits was the same, but the small difference in survival was statistically significant. Magnitudes of this order justify adjuvant chemotherapy in other tumours so that today a decision in favour of adjuvant chemotherapy has an evidence-based background. However, adjuvant chemotherapy cannot be considered as standard treatment. A large randomised trial that was not included in the meta-analysis recently reported completely negative results, despite an acceptable chemotherapy regimen.11 The selection of patients was somewhat more favourable than in a previous Italian trial, which was positive.12 The conclusion of many but not all clinical researchers and sarcoma clinicians is that adjuvant chemotherapy may give some kind of benefit in a fraction of high-risk patients. The patient should be informed that the expected benefit is relatively small.13
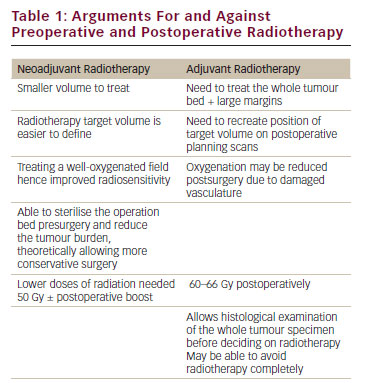
In the localised disease, chemotherapy is sometimes given in a neoadjuvant fashion alone or in combination with radiation therapy. Local control is often an issue in STS, and some cytoreduction following pre-operative therapy often makes surgery easier. This is hard to demonstrate formally in the face of such diversity in clinical presentations, surgical attitudes and histological types. There are data that may suggest a benefit14 along with studies disproving them.15 Combining chemotherapy with radiation therapy is feasible, although there may be serious side effects.16–19 At our institution, it is common practice to liberally resort to chemotherapy, often in combination with radiation therapy when the local presentation suggests a potential benefit. A local advantage is foreseen, while a systemic benefit cannot be ruled out given the high-risk nature of these presentations. It is difficult to say whether this strategy translates into any major survival improvement. However, when guidelines strongly suggest that STS patients are centrally referred, they do so with a view to an integrated approach based on clinical expertise rather than large-scale clinical studies. Again, proof is lacking, and the rarity of STS and their diversity may be the reasons. The above considerations are usually referred to limb and trunk wall sarcomas. Retroperitoneal sarcomas are much rarer and imply a higher risk of relapse even after surgery given the usual extent of these diseases and the lack of any anatomical boundaries preventing the tumour from extending to the entire abdominal cavity. Thus, a phase II study by the Italian Sarcoma Group is currently enrolling patients affected by localised retroperitoneal resectable STS being treated with pre-operative chemotherapy with three cycles of high-dose ifosfamide (14g/m2) administered by a continuous infusion of 14 days, the last two cycles of which are in combination with pre-operative radiation therapy (up to a total dose of 50.4Gy). Sixty-two patients have been recruited so far. Results from this trial concerning the feasibility, safety and activity of treatment are expected next year; however, it is an uncontrolled study.
The employment of regional hyperthermia in combination with chemotherapy has also been advocated in the treatment of sarcomas. Recently, the preliminary results of a multicentre, randomised, controlled clinical trial comparing systemic chemotherapy (four pre-operative and four post-operative cycles of etoposide, adriamicine and ifosfamide) versus systemic chemotherapy plus hyperthermia have been reported. These results showed a benefit for patients in the hyperthermia arm in terms of both local control and survival.20 Therefore, hyperthermia may improve survival through a local effect, being an option for treatment where local control is difficult to achieve and death may be caused by inoperable locoregional disease. Nevertheless, these results need to be confirmed.
The addition of ifosfamide may not have been the only reason for the progress of chemotherapy in the treatment of STS. Currently, the feeling of the sarcoma community is that a histology-driven approach to the selection of chemotherapy may be rewarding. The success story of imatinib in treating gastrointestinal stromal tumours (GISTs), which has been experienced by the same community of clinicians treating STS, has probably been instrumental. Drugs that have been available for years and are known to be ineffective in sarcomas have been now recognised as active in highly selected histological types. This is the case of gemcitabine in the treatment of leiomyosarcomas and angiosarcomas, and taxanes in angiosarcomas. Of note, angiosarcoma is a very rare histological subtype within the sarcoma family. The combination of gemcitabine and docetaxel has been tested in a randomised trial versus gemcitabine alone, and proved to be superior.21 However, a recent trial did not confirm this to be the case in a patient population in which uterine leiomyosarcomas were not represented (which apparently are among the most sensitive to the combination).22 Indeed, it is difficult to identify the histological types that are more likely to respond from the randomised trial. In other words, it is difficult to understand whether leiomyosarcomas and some pleomorphic sarcomas are the only types to take benefit. On the other hand, there is randomised evidence proving that a combination regimen may give more benefit than a single agent.
Recently, a marine-derived drug was approved for the second-line treatment of STS in Europe. Overall, this drug proved to be active in two histological types: leiomyosarcomas and liposarcomas.23–25 Again, this points to a selective antitumour activity. However, the drug also demonstrated impressive activity in metastatic myxoid/round cell liposarcoma,26 a subgroup in the liposarcoma family. A direct effect on the FUS-CHOP translocation that characterises this tumour subtype has been hypothesised. A phase II multicentre, neoadjuvant trial with trabectedine in localised bulky myxoid/round cell liposarcoma is under way. Results are expected next year. Myxoid liposarcomas are a translocation-related sarcoma, along with one-quarter or so of sarcomas, so it will be interesting to know whether selective mechanisms of action are found for the same and other agents in these subtypes. Among the most conventional agents, synovial sarcomas are known to be especially sensitive to ifosfamide, while leiomyosarcomas are apparently rarely sensitive to this drug, at least as a single agent. Dacarbazine may be more active in leiomyosarcoma. All of this points to a selective activity of some agents in selected histological subtypes within the sarcoma family. This poses an important problem. In fact, this is an additional reason for selecting patients for clinical trials. In a rare tumour, this means further difficulties in recruiting patients within a reasonable time interval.
In conclusion, there is a huge need for an improvement in the methodologies of clinical studies in rare tumours, including sarcomas, if we want to demonstrate the therapeutic potential that available drugs have. There is a risk that progress is taking place but cannot be demonstrated. It is very difficult to prove a survival advantage in selected histological types for the very simple reason that well-powered clinical studies are unfeasible, restricting the eligibility criteria to their subjects alone. On the other hand, failing to restrict also prevents studies from proving progress.27
Clearly, selectivity will determine the future role of molecular-targeted agents in STS. The sarcoma community has been deeply involved in the development of imatinib treatment regimes in GIST and all of the new molecular-targeted agents that are currently being tested in mesenchymal tumours of the gastrointestinal wall. The frustration has been not being able to test the same agents in STS. However, the situation is changing.
Imatinib has proved to be effective in a very specific sarcoma, dermatofibrosarcoma protuberans (DFSP).28 The activity and efficacy of imatinib on advanced DFSP was clearly shown in a few cases. The pre-clinical rationale was very strong, since DFSP is marked by a translocation involving chromosomes 17 and 22. The translocation breakpoint generally involves the second exon of the platelet-derived growth factor-B (PDGFB) gene on chromosome 22, which is fused with the collagen 1 alpha 1 (COL1A1) gene on chromosome 17. This results in a transcriptional upregulation of the PDGFB gene through a COL1A1-PDGFB fusion oncogene. As a result, the autocrine and paracrine production of a functional ligand for PDGFRB takes place. Coupled with the demonstration of a clear-cut antitumour activity in a few patients, this highly specific mechanism of action led to the approval of the drug in this entity. Of note, DFSP is essentially a surgical disease, being cured by surgery in most cases. Only rarely does it metastasise or present at such an advanced stage as to require medical therapy. The same agent, imatinib, has antitumour activity in desmoids-type fibromatosis,29 tenosynovial giant cell tumour30 and another group of mesenchymal tumours, chordomas.31
The development of other available molecular-targeting drugs in STS has been slow, but the potential of the sarcoma family has been appreciated, even by the pharmaceutical industry. There are plenty of targets amenable to molecular therapies in the sarcoma family, and one-quarter of them harbour a chromosomal translocation and thereby fusion products, etc., so sarcomas lend themselves to being targeted by new molecular drugs. As of today, there are preliminary reports of activity for vascular endothelial growth factor (VEGF) inhibitors. A clinical study on sorafenib was preliminarily reported, but was essentially negative, with the exception of on angiosarcoma and possibly a leiomyosarcoma.32 Another preliminary study of pazopanib showed more interesting results in terms of antitumour activity.33 A large study on pazopanib is due to begin. Other studies of antivascular agents, whose mechanism of action may be better tailored to advanced lesions, are ongoing. The PI3K–Akt–mammalian target of rapamycin (mTOR) signalling pathway may be abnormally activated in many sarcomas,34 and efforts are under way to target it using agents such as sirolimus and its analogues, deforolimus (AP23573), everolimus (RAD001) and temsirolimus (CCI-779). mTOR inhibitors may lend themselves to be combined with other agents, e.g. anti-IGFR agents may potentially overcome a mechanism of resistance through Akt reactivation.35 One should find the best strategy to exploit the antitumour activity of these drugs. In this regard, a clinical study is ongoing in which an mTOR inhibitor is tested as consolidation of the best response achieved through previous conventional cytotoxic chemotherapy. Anti- IGFR agents are under active study in some sarcoma types, first in the Ewing’s family of tumours.36
The potential of molecular-targeted agents in the advanced phase of solid tumour disease is still unknown. In GISTs, we have learned that tumour resistance is the main limiting factor, and that a high level of heterogeneity may underlie it, so salvage therapy is always a challenge. Furthermore, we have learned that only long-term administration of the drug is able to keep the disease clinically under control, at least until resistance emerges. We have also learned that tumour response may involve major alterations in tumour tissue, but not necessarily size.
Having learnt the ‘GIST lesson’, the sarcoma research community is in a position to fully appreciate the potential of molecular-targeted therapies in STS as long as new agents are actually developed for this family of neoplasms. In GISTs, survival has been effected by molecular-targeted therapy in advanced disease. A cure is unlikely, but the prolongation of survival has been substantial. We are waiting for results in the adjuvant setting, where the cure rate may be affected. In STS, we already have proof-of-concept of major tumour responses to moleculartargeting agents. These have taken place in anecdotal cases or highly selected histological types. Plenty of targets are waiting to be hit, making the sarcoma family a highly ‘druggable’ one. In the meantime, the clinician may be aware that some histological types take benefit from selective, histology-driven chemotherapy, even if it is difficult to demonstrate the survival benefit.