The introduction of human papillomavirus (HPV) testing into cervical screening programmes seems to be inevitable. However, HPV is a highly prevalent virus that is mainly transient. Therefore, it is important to understand HPV dynamics and to identify women at high risk of cervical intraepithelial neoplasia (CIN) or cervical carcinoma to avoid overtreatment. Persistent HPV infection is necessary for the development of high-grade CIN or cervical carcinoma.1,2 Fortunately, in most individuals the immune response eventually leads to clearance of HPV, or to its maintenance in a latent or asymptomatic state in epithelial basal cells. It remains to be elucidated which proportion of HPV infection clears or is maintained in a latent state. Latency implies that the virus may remain within basal epithelial cells, either arrested or very slowly replicating, but barely detectable by current DNA technology. Short-term fluctuations in HPV and fluctuations in HPV throughout the menstrual cycle3,4 raise the following questions:
- When an HPV type is detected, when does a woman have a productive (replicating) infection?
- When is the detected HPV type infectious? (i.e., when is there a high risk of transmission to a sexual partner?)
- When is a newly detected HPV type truly a new infection and when does it represent a re-infection or reactivation?
To answer these questions, we must consider the role of the immune system and the role of the viral load.
Productive Human Papillomavirus Infection
The presence of HPV may indicate a productive (replicating) infection or not. It is important to realise that an infection is more than the detection of the pathogen. Infection is invasion by, and multiplication of, pathogenic microorganisms in bodily tissue, which may produce tissue injury and progress to disease through a variety of cellular or toxic mechanisms.
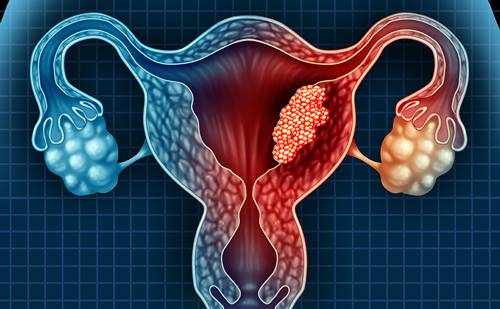
When studying the HPV life-cycle, initial infection requires access of infectious particles to cells in the basal layer through microabrasions. After cell division, one daughter cell migrates and undergoes differentiation. This induces the productive phase, in which expression of E6 and E7 deregulates cell-cycle control, allowing viral genome amplification. On reaching the uppermost layer of the epithelium, the virions are shed.5,6 At this point, depending on the amount of virions shed (i.e., viral load), the virus may be detected and may be transmitted to others. In women who do not successfully resolve their chronic productive HPV infection, CIN may develop and progress to CIN3 and, eventually, to cervical carcinoma (i.e. clinically relevant infection).7,8
Some studies have shown that an increased viral load is associated with an increased risk of clinically relevant cervical lesions.9,10 However, this potential relationship between viral load and disease is not shown for every HPV type. Studies mainly showed that HPV type 16 viral load increases with increasing disease severity.10–12 Snijders et al. showed that viral load was also significantly higher for HPV types 18, 31 and 33 in scrapes of women with ≥CIN2 compared with those of women with normal cytology.9 On the other hand, longitudinal studies showed that baseline viral load did not relate to outcome of CIN2/3 and that only changes in viral load correlated with risk of CIN 2/3 development.13,14 Furthermore, there exists a wide range in viral DNA load levels and a substantial overlap between women with and without CIN3.10,15 Setting a clinically significant viral load cut-off value that is predictive for disease is therefore difficult and viral load is not the preferred tool in clinical practice.
Transmission of Human Papillomavirus
The immune system is important in the natural control of the spread of HPV-associated disease. The immune system may clear the infection or control the virus by keeping it at a low copy number.
Transmission dynamics are dependent on both pathogen and host factors and are defined by three components:
- transmissibility from an infected to an uninfected partner upon exposure;
- the likelihood of exposure between infected and uninfected persons; and
- the time for which a person is infectious.16
When studying genital HPV prevalence, the main factors associated with HPV prevalence are related to sexual behaviour.17 In a simulation model based on likelihood of sexual exposures between infected and uninfected persons and the duration of the infection, the transmissibility of genital HPV from an infected to an uninfected partner upon exposure was estimated to be a median of 40 % per sexual act. The probability of male-to-female transmission would reach virtually 100 % within only 11 acts of sexual intercourse. This estimated high rate of transmission of HPV implies that the potential protective effect of condoms would disappear over multiple acts of sexual intercourse.16 However, condom use does partially prevent HPV transmission and therefore reduces the spread of HPV in a sexually active population. It even may promote HPV clearance and regression of CIN and penile lesions.18,19
Studies analysing HPV transmission in couples showed that HPV concordance is higher in couples with cervical or penile lesions present and that a higher genital viral load increases the transmission rate.20–23 These results on HPV transmission underline the importance of the sexual partner in the viral dynamics of high-risk HPV infection of the genital tract.
Human Papillomavirus – When Is It Newly Acquired, a Re-infection or a Reactivation?
Short-term fluctuations of HPV in an individual suggest that some detected HPV types might be newly acquired whereas others might have been acquired in the past and remained latent, below detection level for a certain period, and then been reactivated.
Reactivation of latent HPV infections was observed in HIV-infected women; however, few reactivation events were identified in HIV-uninfected women.24 The most important factor consistently associated with reactivation in HIV-infected women is a CD4 count less than 200 mm3.24 This suggests that functional immune systems keep HPV infections in a sub-clinical state and that they may be reactivated by immunosuppressive conditions.
Unfortunately, we do not know how frequently latency occurs among immune-competent individuals, how long it may last, what causes reactivation into a detectable state and what fraction of cancer arises after a period of HPV latency. Because of the apparently low rate of reactivation, large studies would be needed to adequately address reactivation in an immune-competent group.24 Studying HPV reactivation in cervical infection is also complicated by the inability to distinguish reactivation of an existing infection from re-infection with the same HPV type through sexual contact with an infected partner. Therefore, knowledge of previous infection, sexual behaviour within the HPV testing interval and testing the sexual partner are required to exclude the possibility of re-infection. Furthermore, it is unclear whether clearance of carcinogenic HPV infections may result in type-specific immunity and whether immunity needs boosting over time.20,25,26 Moreover, only about 50–60 % of women with carcinogenic HPV infection develop detectable serum antibodies.20,21,25,26
Some studies report a relation between viral load and seroconversion of immunoglobulin G (IgG),12–19,24,25 whereas others have identified persistent HPV infection to be a significant factor.21,22 A high viral load may provide an acute and rapid immune response, whereas a persistent infection maintains a slow gradual boosting effect.25 Another factor potentially related to seroconversion of IgG is oral contraceptive use.22,25 Hormones may induce transcription of the integrated viral oncogenes and influence the mucosal immunity in the genital tract.23 The influence of the endogenous and exogenous hormones on the mucosal immune response most likely explains the differences in HPV detection within and between the oral contraceptive cycle and the natural menstrual cycle.3
This variety in data on HPV seroprevalence demonstrates that the host immune response against HPV is only partially understood and that HPV serology is a poor marker of current infections or related lesions.
Human Papillomavirus DNA Detection in Cervical Cancer Screening
To date, HPV DNA testing has been used in most cervical screening programmes as a triage test for women who have abnormal cytology. However, HPV DNA-based primary screening has proved to be more sensitive than cytology in detecting high-grade CIN, but with a lower specificity.27,28 Additionally, HPV DNA-based primary screening may also improve the participation rate, especially when self-sampling is used for specimen collection, thereby increasing the overall effectiveness of the screening programme.29,30 Self-sampling has been proved to have a sufficient sensitivity to screen women otherwise not screened, but further research is necessary before wide implementation in a national screening programme is possible.
To improve the specificity of HPV DNA-based primary screening, HPV dynamics should be taken into account.2 HPV dynamics can indicate whether a detected high-risk HPV type can be considered as:
- a newly acquired infection, or re-infection, or reactivation, that could be a transient infection or potentially persisting and causing CIN within several years;
- an already persistent infection likely to cause/have caused a CIN or cervical carcinoma (i.e., a chronic productive infection); or
- an accidental pick-up of a latent infection.
HPV persistence as a clinical marker may be of value to identify women who are at high risk of cervical cancer. Repeat (genotype-specific) HPV DNA testing at 12 months may therefore be a valuable tool to identify women at increased risk of CIN and cervical cancer.31 HPV genotyping might be used as an additional tool to decide whether to treat or not, because some types are more likely to persist than others.31 Especially for women under 30 years of age, it will be important for clinicians to be conservative and wait for evidence of a persistent (chronic productive) high-risk HPV infection rather than act on the first positive test for high-risk HPV, because these women are more likely to have a transient infection and the lesion (if present) may regress.31–34
Novel biomarkers – immunologic, genetic or viral factors – may be useful for triage in HPV DNA detection-based primary screening to support decision-making on treatment or a ‘wait and see’ policy.35,36 Currently developed biomarkers are E6 and E7 HPV messenger RNA transcripts, methylation of several genes, markers for viral integration and of chromosomal instability, and markers of increased cell proliferation such as Ki-67 and p16.37–39
The high negative predictive value of the HPV DNA test for developing CIN3 means that very few relevant lesions are missed.27,40 However, studies have shown that, in natural HPV dynamics, a sequence of positive high-risk HPV samples may be interrupted by a single high-risk HPV-negative sample.41,42 Within these fluctuations, we may assume either that the viral load is below detection level (depending on the replication rate of the virus, latency or the sensitivity of the HPV DNA test used) or that there may be a sampling error. When a non-productive high-risk HPV infection is ‘missed’, there are most probably no clinical consequences. However, when an active high-risk HPV infection is missed owing to the low sensitivity of an HPV test or sampling error, this leads to inadequate follow-up and treatment. Thus, to safely extend this cervical screening interval in case of a negative test, the sensitivity of the HPV DNA detection test used in primary cervical cancer screening should be sufficiently high to detect CIN3 or a chronic productive high-risk HPV infection likely to produce CIN3 within the screening interval.
Influence of Human Papillomavirus (HPV) Vaccination on HPV Dynamics
As an increasing proportion of the population is vaccinated, the prevalence of cervical abnormalities will decrease. However, given the lag in time between HPV infection and the development of cervical cancer, (universal) vaccination is likely to have only a minimal impact on CIN and cervical cancer rates until 10–20 years from now.43 Additionally, vaccination against HPV cannot provide 100 % protection against cervical carcinoma and its precursor lesions and little is known about the potential long-term benefit of (cross-)type immune response. Therefore, vaccinated women still need to be followed and cervical cancer screening programmes must continue.
The potential impact of HPV vaccination on the epidemiology of HPV and the rate of abnormal cytology depends on the following variables:
- vaccination coverage;
- the duration of vaccine-induced immune protection;
- the target high-risk HPV types of the vaccine;
- the rate of cross-protection; and
- whether HPV type replacement takes place.
In 2009, the UK and Australia used school-based vaccination programmes and achieved a high three-dose completion rate of approximately 80 and 70 %, respectively.44,45 In the Netherlands, however, only 52 % of the girls in the target age group received the HPV vaccine. When vaccination coverage is less than 90 %, herd immunity obtained by only vaccinating women may be insufficient to eradicate the targeted HPV types.46 When considering vaccinating boys to increase herd immunity, the potential gain of a further reduction of cervical cancer must also be carefully weighed against the extra costs. It appears that, when female programmes obtain high (over 75 %) coverage, the vaccination of males provides only a small additional benefit and is not cost-effective.47
In the future, long-term follow-up studies should determine the true efficacy and duration of vaccine-induced immune protection of both vaccines. However, to date there have been no cases of infection or cytohistologic lesions associated with HPV16/18 in 7.3 years of follow-up after vaccination with the bivalent vaccine (HPV-16/18 AS04-adjuvanted: Cervarix®; GlaxoSmithKline, North Carolina, US).48 Vaccination with the quadrivalent vaccine (HPV- 6/11/16/18: Gardasil®; Merck & Co., New Jersey, US) had a high prophylactic efficacy against low-grade cervical and vulvovaginal neoplasia and condylomata associated with the vaccine types through 42 months of follow-up; vaccine efficacy against CIN1 was 96 %.49
The percentage of all cervical cancers attributable to HPV 16/18 in Europe has been estimated at 71 %.50 The percentage of prevented cervical cancer is potentially higher as both vaccines have reported cross-protection against other high-risk HPV types. As summarised by Szarewski,51 the efficacy provided by the bivalent vaccine against CIN2+ lesions was 100 % for HPV-31 or -45, 66.1 % for non-HPV-16 α-9 species and 77.3 % for non-HPV-18 α-7 species;52 the efficacy provided by the quadrivalent vaccine against CIN2+ lesions was 58.7 % for HPV-31 or -45, 35.4 % for non-HPV-16 α-9 species and 47.0 % for non-HPV-18 α-7 species.53 Although these results are encouraging, the duration of cross-protection is unknown.
Currently, the efficacy of a broad-spectrum vaccine (Merck) against nine HPV types, including seven oncogenic HPV types, is being studied in a randomised phase III trial. When a polyvalent vaccine against nine HPV types is implemented, the prevalence of the majority of cervical cancer-associated HPV types will be drastically decreased and the discussion on cross-protection will change.
There is a possibility that the distribution of HPV types may gradually change in vaccinated populations to fill the vacated ecologic niches after the elimination of HPV types 16 and 18.54,55 Type replacement is a viral population dynamics phenomenon and is defined as elimination of some types causing an increase in incidence of other types. This effect can occur only if two conditions apply:
- there exists partial competition among different types during natural infection; and
- the vaccine does not afford cross-protection against types affected by this natural competition.55
Future epidemiologic studies are needed to show whether type replacement occurs.
Challenges to Primary Cervical Cancer Screening After Vaccination
The potential impact of HPV vaccination needs to be taken into account when planning for future screening guidelines. It is estimated that there will be a 50–60 % reduction in colposcopy referrals owing to prevention of HPV 16 and 18 lesions. This will lower the positive predictive value of any screening test for cervical cancer.56 However, HPV testing is automated and therefore more objective, and thus is less likely to be influenced by this effect than cytology.57 Owing to the high costs of vaccination, it is important to restrict the costs of cervical screening programmes and implement an approach based on vaccine implementation.58 However, later and less frequent screening will probably become an acceptable worldwide policy only if vaccination uptake is high across all social and economic strata.59 To help develop new guidelines for cervical cancer screening algorithms in the post-vaccine era, future epidemiologic studies should monitor HPV prevalence, type replacement, the level of protection against HPV 16 and 18, the level of cross-protection, the duration of protection and the population coverage of the vaccination.
In the future, provided there is high vaccination coverage with a polyvalent vaccine or a high level of cross-protection, a long duration of protection or a validated booster vaccination schedule, screening will likely be superfluous. ■