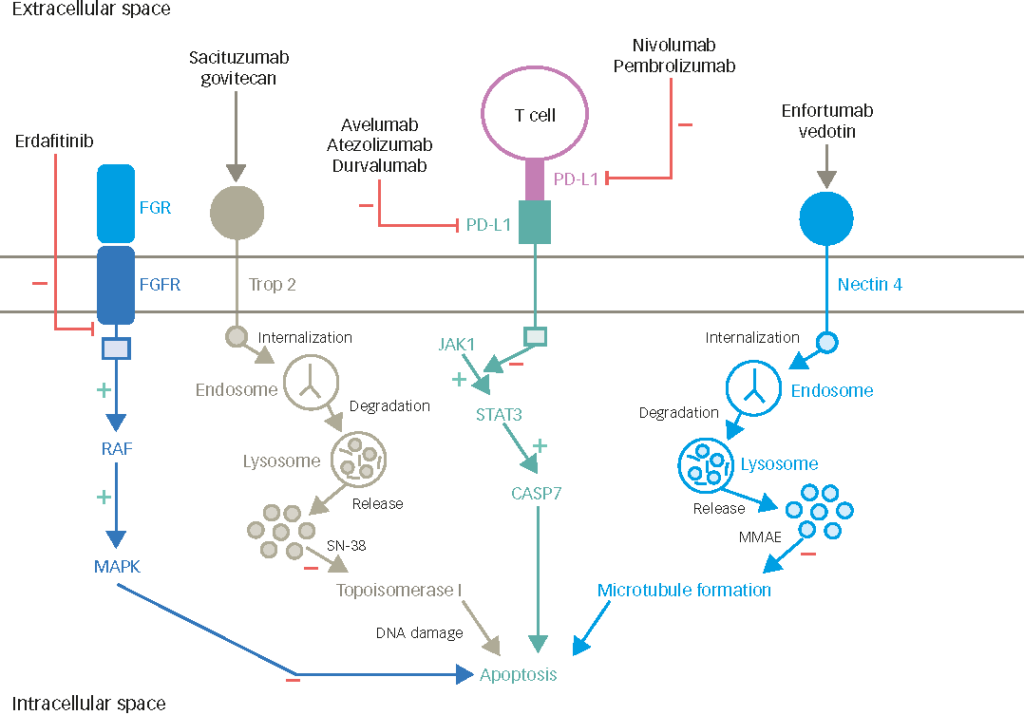
An overview of evidence on use and development of cytotoxic and targeted agents in the second-line setting after failure of a platinum-based regimen will be presented below. Additional considerations on the possible role of immunotherapy in bladder cancer are also discussed. Combinations of vinflunine with therapeutic agents that are already in use in bladder cancer are known to have potential additive and synergistic effects, which may affect both efficacy or tolerability. Possible combinations of vinflunine include combinations with ‘classic’ cytotoxic agents, vascular endothelial growth factor (VEGF) inhibitors, tyrosine kinase inhibitors (TKI) and mammalian target of rapamycin (mTOR) inhibitors. Checkpoint modulation of T-cell differentiation and vaccination strategies are at a much more theoretical and experimental stage, but also worthy of mention, due to the immunological nature of bladder cancer.1
Classic Cytotoxics
Vinflunine combined with classic cytotoxic agents, such as gemcitabine or carboplatin, is associated with haematotoxicity (leukopenia, neutropenia, thrombocytopenia and anaemia) and stomatitis. Vinca alcaloid class effects include cardiotoxicity and neurotoxicity, which may be a concern in combination with taxanes. Limited data are available on the potential drug interactions and toxicities that may occur if vinflunine is combined with other agents.
Pemetrexed was a promising drug for second-line bladder cancer treatment, but conflicting results led to it falling out of the bladder cancer field. It remains an active drug considered to be an option in bladder cancer, which functions like an improved version of methotrexate. It is approved in the second-line treatment of non-small cell lung cancer (NSCLC). The planned Scandinavian NUCOG2 randomised phase II trial will evaluate vinflunine plus pemetrexed versus vinflunine alone in the second-line setting.
Tyrosine Kinase Inhibitors, Vascular Endothelial Growth Factor Inhibitors and Mammalian Target of Rapamycin Inhibitors
Several elements from preclinical studies suggest that TKI and mTOR inhibitors may have a role in bladder cancer. Activation of the PI3K/Akt/mTOR pathway has been shown to correlate with tumour progression and reduced survival in patients with urothelial carcinoma of the bladder.2 There is evidence for PTEN-independent Akt activation and Akt-independent p27Kip1 expression in advanced bladder cancer, thus supporting further investigation of protein profiling and targeted therapy in bladder cancer.3 An ongoing phase II trial is exploring the activity and safety of everolimus with or without paclitaxel as first-line therapy for cisplatin-ineligible patients with advanced urothelial carcinoma (NCT01215136).
Sorafenib was tested in a prospective, randomised, double-blind phase II trial that compared GC plus placebo versus GC plus sorafenib in 85 patients with locally advanced or metastatic urothelial carcinoma in the first-line setting.4 The trial resulted in a negative outcome, with no significant benefit in progression-free survival (PFS) or overall survival (OS) upon addition of sorafenib (PFS 6.3 months in the GC arm versus 7.2 months with added sorafenib; OS 10.5 months in the GC arm versus 11.3 months in the sorafenib arm). Investigation of sorafenib as a monotherapy also resulted in a negative outcome following a small preliminary phase II trial in 27 patients with advanced urothelial carcinoma in the second-line setting.5 The trial observed no objective responses. The 4-month PFS rate was 9.5 % and median OS was 6.8 months. Despite the disappointing outcomes, these studies were nevertheless interesting in terms of planning for future possible combinations. There may be some potential in combining sorafenib with vinflunine.
The planned NUCOG3 phase I dose finding, single arm trial will test vinflunine plus sorafenib in the second-line setting. Fixed doses of vinflunine will be administered in two starting dose groups, at 280 mg/m2 or 320 mg/m2 on day 1, followed on day 2 by three dose steps of 400, 600 and 800 mg sorafenib over 21 days.
Sunitinib was tested in a phase II study in 77 pre-treated patients with metastatic urothelial carcinoma in the second-line setting did not show promising results.6 A 50 mg daily sunitinib dose failed to show significant prolongation of PFS and OS. However, partial responses were observed in some patients, identifying antiangiogenesis-targeted therapy as a viable approach for bladder cancer treatment. Other data evaluating sunitinib efficacy as part of combination chemotherapy regimens support this notion. In a preclinical model, sunitinib was active against human urothelial carcinoma and enhanced the activity of cisplatin.7
Of note, in vivo data in transitional cell carcinoma cell lines have shown that sunitinib can enhance Bacillus Calmette–Guérin (BCG)-mediated cytotoxicity through the apoptosis pathway.8 Similarly, sunitinib synergistically potentiated the anti-tumour effect of gemcitabine in human bladder cancer cells.9 These proposed therapeutic combination models may have potential future clinical applications in bladder cancer treatment. Of note is the possibility to combine a systemic drug such as sunitinib or maybe vinflunine with topical application of BCG (immunoinstillation), mitomycin or gemcitabine (chemoinstillation; see below) and thereby achieve a dual method of application synergistic effect. Nevertheless, haematotoxicity profile of sunitinib as well as the fibrosis of the bladder wall should be considered for any such combination therapy.
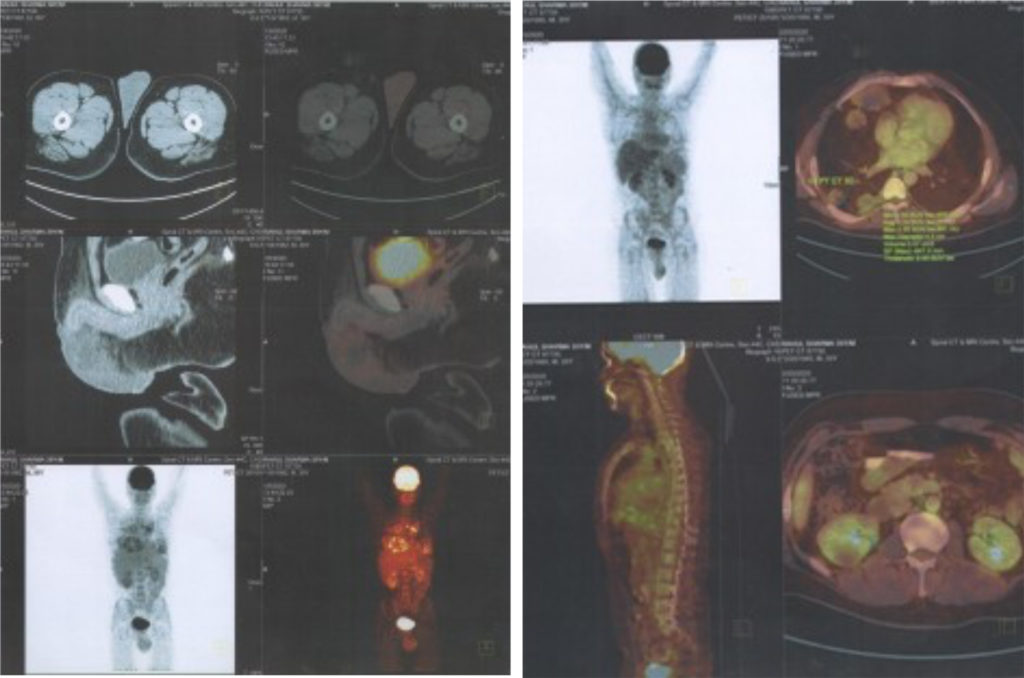
Pazopanib monotherapy was investigated in a phase II study in patients with relapsed or refractory urothelial carcinoma in the second-line setting.10 The study demonstrated potential anti-tumour activity of pazopanib. Patients underwent computed tomography (CT) and fludeoxyglucose-positron emission tomography (FDG-PET)/CT scans at baseline and every 4 weeks thereafter. Among 30 evaluable patients, four had a confirmed RECIST-defined partial response (PR), and 20 had stable disease. Although the response assessed by RECIST was modest, responses were observed in CT and PET scans, highlighting the need for new criteria to assess response of angiogenesis inhibitors, similar to the data that used a lower RECIST ‘response’ threshold described by Krajewski et al. in patients with TCCU treated with second-line vinflunine.11
There is some controversy on the efficacy of pazopanib, due to conflicting data reported by the Mayo clinic in 19 metastatic urothelial carcinoma patients in a phase II trial.12 Of 18 patients evaluable for toxicity, seven experienced adverse events that were at least possibly related to treatment. Toxicities included anaemia, thrombocytopenia, leucopenia and fatigue. None of the 16 patients evaluable for efficacy responded according to RECIST criteria during the first four 4-week cycles of treatment, and median PFS was 1.9 months. The trial was stopped due to these poor outcomes. Translational data measuring VEGF levels are expected. Another ongoing phase II trial is investigating pazopanib monotherapy also as second-line therapy in patients progressing after platinum-based chemotherapy (NCT01031875).
A Different Angle of Attack – Immunomodulation
The potential of specific immune therapy with cyclophosphamide in uro-oncology (renal cell cancer [RCC]) is being explored, in an attempt to attack tumours on a different front line.13 Of note, regulatory T-cell (Treg) survival in bladder cancer is induced by the PKB pathway in patients after radiotherapy, and Tregs show increased Akt levels.14 A single low dose of cyclophosphamide reduced Tregs and immunotolerance in preclinical cell line models. Hypothetically, upon addition of another drug (e.g. sunitinib, which also has modest activity on Treg levels),15 a synergistic effect may be observed, not only in terms of chemotoxicity, but also an immunomodulatory effect.
Urothelial carcinoma is an immunological tumour. The effects of intravesical BCG in non-muscle invasive tumours are well known. BCG is believed to work by triggering the body’s immune system to destroy cancer cells, thus providing evidence that immune modulation in bladder cancer is an effective approach. It is conceivable that immune modulation could be conferred by vinflunine, although it is currently not known whether vinflunine has an immunomodulatory effect. If it were possible to produce an immunomodulatory effect with vaccination, survival could not only be prolonged, but future treatment regimens could be made more effective.
Potential Role of Vinflunine in Non-muscle Invasive Bladder Cancer In the setting of non-muscle invasive bladder cancer, a phase I study prior to cystectomy to examine whether an immunomodulatory effect conferred by vinflunine can be observed would also be interesting.
Gemcitabine is being used intravesically in some trials. The concerns are: how much will the agent penetrate into the bladder wall, and, secondly, how much inflammation will be caused by this form of treatment. Fibrosis and bladder shrinkage can be a severe problem. It would be unacceptable to have to perform cystectomies in patients because of these side effects. Vinflunine is an irritant intravesically but most probably will not cross the barrier of the bladder’s epithelial wall. To the best of our knowledge, there are no data on this aspect. If there are lesions in the bladder, e.g. from a previous resection, it may be risky to administer vinflunine. But such an approach may be considered in the upper urinary tract. There may be potential in directing treatment to the upper urinary tract with a ureteral catheter and then performing a drip instillation. This would be less of a risk, because these cancers often lead to nephrectomy, so pyelonephritis could be tolerated if kidney preservation is the objective.
Vinflunine may augment an immunomodulatory effect in the bladder wall because with BCG, the duration of this effect is limited, as the disease eventually returns and the majority of patients are unable to tolerate BCG after 2 years. There is a risk of accumulating so many side effects that treatment creates a tumour-free, but heavily scarred, non-compliant irreversibly damaged bladder. BCG tolerance and failure is an area of unmet medical need, which offers the possibility to test new treatments. Thus, carrying out a phase I study before cystectomy would be of interest, to know appropriate doses, measure levels in the bladder, and to see how much vinflunine penetrates. A similar approach to that used by Dalbagni et al. in a phase I trial could be explored with vinflunine. In this trial, intravesical gemcitabine was administered in patients with refractory superficial bladder cancer or who were intolerant to intravesical BCG therapy, and who were unwilling to undergo cystectomy.16,17 Naturally, in order to avoid ethical concerns, this needs to be initially explored in preclinical models, e.g. comparing primary cell lines from normal urothelium and from tumour cells.
Importantly, there is a niche opportunity for exploring the use of vinflunine in these patients. In terms of numbers, three quarters of tumours are non-muscle invasive, and one-quarter are muscle invasive. Of those, more than half will eventually need some form of instillation therapy, resulting in large prospective numbers of patients requiring therapy.18
Ideally, it would be interesting to consider testing whether vinflunine has an immunomodulatory effect by affecting the levels of Tregs. If some activity is measured, then vinflunine could either be combined with a drug that also affects Tregs and/or administered with a specific peptide vaccination that would need defining. This approach is an open field that aims to combine two toxic drugs that have distinct mechanisms of action and attack tumours from a different front. In addition to low-dose cyclophosphamide, another antiangiogenic effect may be conferred by the regimen explored by Pietras and Hanahan in a mouse model, in which low-dose metronomic chemotherapy plus an antiangiogenic compound were administered.19