We present a 21-year-old Somalian male, who grew up in the UK, who presented initially to the urology department at a London university hospital with a 4-month history of two penile lesions. These lesions were located in the glans penis and had gradually enlarged, with concomitant bleeding and purulent discharge. In addition, the patient mentioned a 1-year history of intermittent night sweats. His past medical history included a circumcision at birth and hay fever. He denied any previous sexual activity. The family history was negative in terms of other malignancies. On examination there was a 1 cm diameter polypoid nodule on the right hand side of his urethral meatus and a 5 mm subcutaneous nodule on the left hand side of his glans penis. These lesions were non-tender and there was no palpable lymphadenopathy. Blood tests including full blood count, electrolytes, bone profile, myeloma screen, human immunodeficiency virus (HIV) antigen, serum human herpes virus 8 (HHV8) DNA and syphilis screen were negative. Hepatitis B and C virus were not detected. Immunoglobulin (Ig)A was raised polyclonally with marginally low IgM levels (0.3). Urinary Bence Jones proteins were normal. CD4/8 testing was not performed as the patient was HIV negative, had normal lymphocyte count at presentation and following local laboratory policy. He underwent local excision of the two lesions. Histopathology revealed spindle cell lesions (see Figures 1a and 1b) with tumour cells expressing CD34 and HHV8 (Figure 1c) on immunohistochemical (IHC) staining. They were Desmin negative. These findings were consistent with a diagnosis of Kaposi’s sarcoma (KS). The diagnosis was made at the National Lead Department for Penile Pathology in the UK. As the lesions extended to the deep margins, further wide local excision was performed confirming clear margins. At routine follow-up at 11 months, polyclonally raised IgA with low IgM (0.2) remained the only abnormalities on blood tests. The patient has remained in complete clinical remission for the last 18 months.
KS is a neoplastic vascular lesion first described in 1872 by Moritz Kaposi. Lesions can be subdivided into four distinct forms: classic, endemic, iatrogenic and AIDS-associated.1,2 The classic form commonly presents in elderly men of Mediterranean decent and Ashkenazi Jews.3 HHV8 is endemic in sub-Saharan Africa but Somalia is not part of the sub- Saharan KS belt.4 KS often presents as cutaneous nodules, commonly on the legs and feet.3 Initial presentation on the penis is rare, especially in HIV-negative, immunocompetent patients.5 Primary penile involvement in a HIV-negative patient was first described in 19025 and occurs at a median age of 57 years.6 The median age of appearance of typical classic KS is 64 years.7 Table 1 displays documented cases of primary penile KS in HIV-negative patients. In HIV-positive patients, presentation on the penis exhibits aggressive behaviour1 and in about 3 % of cases is a primary penile lesion.6 Lebari et al. recently reported on a primary penile KS case in a HIV-positive patient who was well controlled on highly active antiretroviral therapy (HAART)8 and also documented that in the last 10 years this presentation appears more common in immunocompetent patients. KS lesions are often painless and few in number. Multiple lesions have been reported.2 Lesions may be skin-coloured, erythematous, violaceous nodules, papules or plaques.9,10 When the penis is involved, common areas affected are the glans penis, foreskin, frenulum and urethral meatus.10 The urethral shaft involvement is rare.6 In cases with extensive penile involvement, lymphatic oedema has been reported.3 The differential diagnosis may include: condyloma acuminate, molluscum contagiosum, pyogenic granuloma and glomus tumour.10
Biopsy is diagnostic and histology reveals sinous vascular spaces, pleomorphic spindle cells with mitoses, extravasated erythrocytes and haemosidrin-laden macrophages. A cellular infiltrate of lymphocytes and plasma cells may be present.3,11 Cells that line small blood vessels display abnormal proliferation by extending in an outward direction from the vessel, penetrating surrounding collagen bundles resulting in ‘stellate’ blood vessels.12 IHC staining for CD34 antibodies is often positive in the endothelial lining of the slit-like spaces and in spindle cells.1
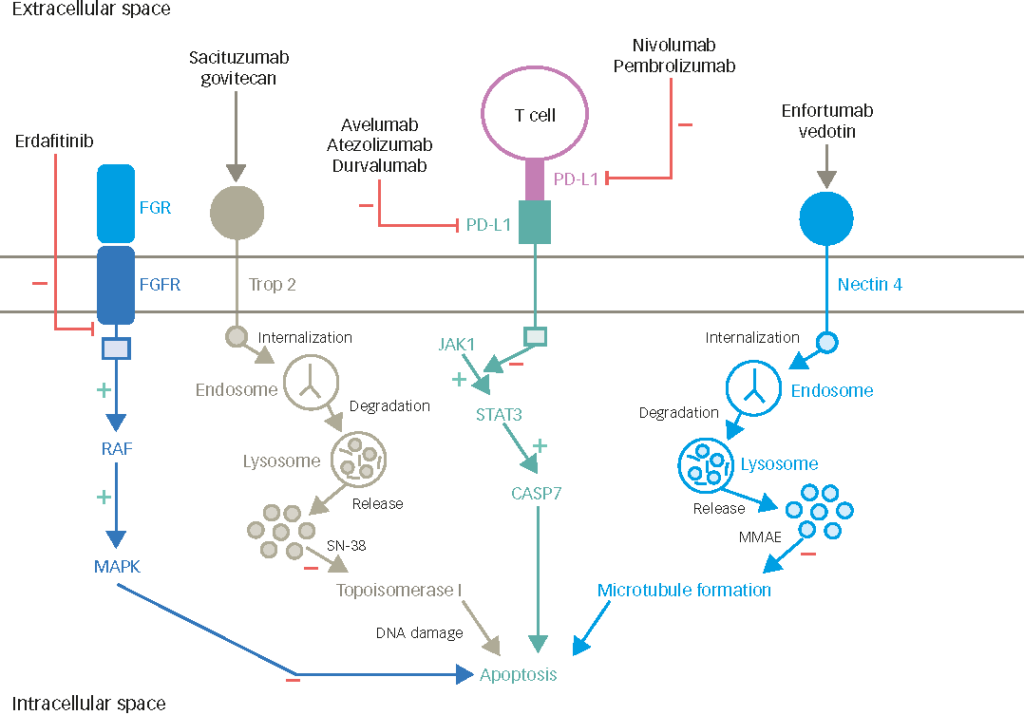
Although the pathogenesis of KS is unknown, it is thought to occur due to vascular hyperplasia and a link with HHV8 has been well documented in all subtypes of KS.10 HHV8 can be transmitted by sexual and nonsexual contact. It has been postulated that HHV8 may be spread by saliva in the general population.11 HHV8 is thought to be an important but not necessary factor in the pathogenesis of KS. Immunosupression is thought to be the most important cofactor.13 HHV8 is thought to contain cellular gene homologues that may encourage cell proliferation, inflammation and angiogenesis while inhibiting apoptosis.14 Tumour growth may further be encouraged by host immune response and cytokines released by cells infected with HHV8 (e.g. fibroblast growth factor).13 HHV8 genome has been shown to be present in at least 90 % of HIV-positive patients with KS.2
There is no standard treatment for primary penile KS lesions, although local surgery is recommended, especially for isolated lesions.4 Other treatments may include cryotherapy, electrosurgery, radiotherapy, chemotherapy, intralesional alpha- and beta-interferon, photodynamic therapy or topical agents e.g. imiquimod, nitrogen.15 Recurrence is very rare if lesions are completely excised.4
In summary, our patient was the first HIV-negative Somalian male diagnosed with a primary penile KS. He also is the first teenage and young adult (TYA) patient diagnosed with a primary penile Karposi’s sarcoma. HHV8 was detected in tumour cells by IHC. This case supports the theory that HHV8 may be spread non-sexually and that other factors than immunosuppression may be implicated in the development of primary penile KS. To our knowledge, this is the youngest reported case of primary penile KS in a HIV-negative patient. Although primary penile KS is extremely rare, it should be considered as a differential diagnosis of non-specific lesions in this area, regardless of the HIV status or age of the patient.