Uterine sarcomas in general are rare: they account for 4% of all uterine malignancies.1–4 Endometrial sarcomas account for 10–15% of all uterine sarcomas. They make up fewer than 1% of all gynaecological malignancies.1,2,5,6 The reported incidence is approximately one to two cases per million women in the US.6,7 Women often present with an enlarged uterus or have complaints of heavy menstrual bleeding. Occasionally, the diagnosis is established by endometrial biopsy or diagnostic curettage. Most often, however, the diagnosis is not recognised until the time of hysterectomy. Generally, these women are pre- or peri-menopausal at the time of diagnosis.5
Endometrial stromal tumours are composed of cells that resemble the stromal cells of proliferating endometrium.1 Previously, endometrial sarcomas were divided into low-grade endometrial stromal sarcomas (LGESS) and high-grade endometrial stromal sarcomas, as originally described by Norris and Taylor.2 Current terminology substitutes the term undifferentiated endometrial sarcoma for high-grade endometrial sarcoma because of the pleomorphic nature of the tumour and the lack of endometrial stromal differentiation histologically. The World Health Organization (WHO) classifies endometrial sarcomas as LGESS and undifferentiated endometrial sarcoma.5
Endometrial stromal nodule, a benign tumour and LGESS recapitulate the endometrial stroma of proliferative endometrium. How they differ is based on the growth pattern: endometrial stromal nodules are circumscribed; LGESS are characterised by infiltrative tongues of tissue, generally low mitotic activity (<10 mitotic figures/10hpf), mild cytological atypia and a generally indolent behaviour. Undifferentiated endometrial sarcomas have a pleomorphic appearance, marked cytological atypia and high mitotic activity (>10 mitotic figures/10hpf) with atypical mitotic figures.8–11 They tend to grow rapidly and metastasise early, and are generally fatal. Disease-free survival and prognosis are substantially better for low-grade versus undifferentiated sarcomas.2,7,8,12 When LGESS recur, local/regional sites are more common than distant sites.8The standard of care and primary treatment for LGESS is surgery, which is the only potentially curative procedure. When surgery is performed, it is customary to perform a total hysterectomy. Bilateral salpingo-oophorectomy is often performed since the ovaries are a common site of metastases and also a source of oestrogens. However, there are conflicting reports to support this practice; some authors report that the recurrence rates are the same in patients who have their ovaries compared with those without.8 Post-operatively, various treatment strategies have been reported, utilising radiation therapy, chemotherapy or hormonal therapy. However, for patients with localised disease, studies demonstrate no difference in survival comparing patients who receive adjuvant therapy versus those who do not.5,13 Various chemotherapy regimens have been reported in the adjuvant setting, but to date there are no convincing data to support routine use. Radiation therapy has been shown to prevent local recurrence but not distant metastases.5,9,14
Recent studies have examined hormone therapy based on the observation that LGESS express oestrogen (OR) and progesterone receptors (PRs), making this a potential target for treatment. Studies have shown success with the use of high-dose progestin therapy. Furthermore, the use of hormonal therapy has expanded to the use of other agents such as gonadotropin-releasing hormone (GnRH) analogues and aromatase inhibitors.7 This article will review current recommendations and recent studies investigating the role of hormones in treating metastatic LGESS.
Discussion
Under standard conditions, the cycling of endometrium is controlled and regulated by the steroid hormones oestrogen and progesterone. These hormones bind to their respective receptors, which are expressed in various isoforms. Progesterone has isoforms alpha and beta, which are primarily expressed in normal endometrium. Primary LGESS express both isoforms, but alpha is the dominant isoform. In recurrent LGESS, alpha levels are reduced and the beta becomes increased. Generally, 80% of LGESS express oestrogen alpha receptors and the beta is not detected.5 This is the basis and evidence for the fact that LGESS arise in the setting of oestrogen stimulation.
Clinicians have noticed that recurrences occur more frequently in patients who are on exogenous forms of oestrogen such as tamoxifen.6,7 Therefore, it is often recommended that the ovaries be removed at the time of surgery and progestins or aromatase inhibitors be utilised to decrease oestrogen levels. This is only applicable to LGESS, as undifferentiated endometrial sarcomas tend to lose expression of OR and PR, raising the possibility of a different pathway or pathogenesis compared with LGESS.5 In a study performed by Ioffe et al., OR and PR were expressed in 76% of their cases of LGESS and all undifferentiated endometrial sarcomas showed no expression.3
Surgery
Endometrial sarcomas are initially treated with surgery. The recommended surgical therapy is total hysterectomy with bilateral salpingo-oophorectomy.9 Surgery is also advocated for debulking of recurrence and for residual tumours after pelvic radiation and chemotherapy.2,8–10,12 Oophorectomy serves the purpose of removing the trophic production of oestrogen in pre-menopausal patients. In one study, there was 100% recurrence in patients who retained their ovaries versus 43% in those who had them removed.9 Nonetheless, there are studies that challenge the effectiveness of oophorectomy in preventing the recurrence of LGESS.15 The role of regional lymph-node dissection in LGESS also remains controversial. Lymph-node dissection is generally not recommended for stage I LGESS.16 Although there are data indicating that the rate of lymph-node involvement may be higher than previously thought, this remains controversial. In one retrospective study, lymph-node metastases were seen in five of 15 patients with LGESS, while another study showed no metastasis in seven patients.2 Negative margins for a surgically resected tumour are important, as shown in studies by Nordal et al., but there are other important prognostic factors, such as tumour grade, tumour diameter and menopausal status.9
Radiation
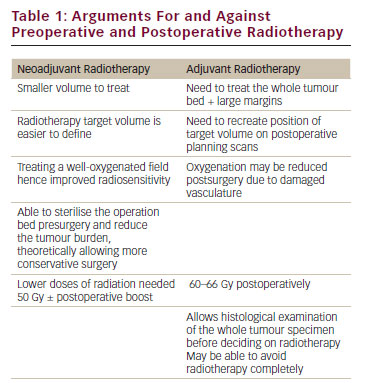
LGESS recur in up to 50% of patients as reported in the literature; tumours are most likely to recur in the pelvis, abdomen and lungs.5,6,8 The benefits of radiation therapy are still unclear. There are a number of studies suggesting a survival advantage and improved local control.2 Studies in the early 1990s by Berchuck et al. showed a 57 and 40% response rate to chemotherapy and radiation therapy, respectively.10 Adjuvant radiation prevents local recurrence in the pelvis but clearly does not prevent recurrences at distant sites.5 There is no significant difference in overall survival or in disease-free survival comparing those who undergo post-operative pelvic radiation and those who do not.9 Various recommendations have been made in terms of the use of radiation therapy in the adjuvant setting. The National Cancer Institute (NCI) recommends adjuvant radiotherapy for stage I–III but not for stage IV, which is treated with systemic chemotherapy. The National Comprehensive Cancer Network (NCCN), however, recommends radiotherapy for all resected uterine sarcomas stage I–II, except for LGESS.2 One study reported on 21 women with LGESS; 15 received radiotherapy following surgery, with an overall local control rate of 93.8%. The authors conclude that the combination of surgery and radiotherapy may be the most effective strategy.17 Nonetheless, it is difficult to interpret these data given the small number of patients, the indolent behaviour of these tumours and the retrospective nature of these studies. The available data seem to indicate that adjunctive radiation does not confer any significant survival benefit for early-stage LGESS.Chemotherapy
The role of chemotherapy in the treatment of LGESS remains unclear. There is discordance in the literature pertaining to chemotherapy treatment of LGESS. Most studies report on patients with advanced-stage disease, often combining undifferentiated endometrial sarcomas with LGESS. In one study, 21 patients with advanced, recurrent or metastatic endometrial sarcomas were treated with ifosfamide and there was an overall response rate of 33.3%.18 There are various case reports and retrospective studies with small patient populations quoting successful treatments utilising chemotherapy. The chemotherapy regimens vary, generally including platinum drugs, taxanes, ifosfamide and doxorubicin. Berchuck et al. published a study showing a 50% response rate to doxorubicin in their patient population.10 Of all the data on chemotherapy agents, most indicate a favourable response to regimens that include doxorubicin. In spite of this demonstrated response to chemotherapy, most studies show no advantage in progression-free survival or overall survival.2 At this time, the data do not support the use of radiation or chemotherapy in the adjuvant setting; as summarised by Haberal et al., there appears to be no difference in recurrence rates between those who receive and those who do not receive adjuvant therapy.9
Hormonal Therapy
As with other neoplasms of the female genital tract, LGESS often express OR and PR, which serve as potential targets for therapy. Instead of using chemotherapy or radiation therapy, which often have deleterious side effects, hormonal agents have a more favourable therapeutic index. Many anecdotal reports in the literature appear to support this approach. Although some reports question the effectiveness of hormonal treatment,19 the majority of studies demonstrate a measurable benefit. In general, LGESS express OR and PR more than undifferentiated endometrial sarcomas, but not all tumours express OR and PR. Therefore, it is recommended that all endometrial sarcomas be evaluated for OR and PR expression.20
Endometrial sarcomas often lose OR and PR expression in metastases and can also switch to different isoforms, making tumours unresponsive to hormonal therapy, resulting in treatment failure.5 There are no prospective studies examining the use of hormonal therapy in the treatment of LGESS due to the rarity of the tumour; however, a number of retrospective studies have been published attesting to the effectiveness of hormonal therapy in the treatment of LGESS. In a study completed by the current authors, 13 patients with LGESS were identified and six had metastatic or recurrent disease. All but one patient underwent surgical resection and all six patients with metastases had tumours that tested positive for OR and PR. All six were treated with megestrol acetate initially for a period of one to four years. Two patients were then changed to maintenance with medroxyprogesterone acetate; one patient was lost to follow-up. Three patients with persistent disease were changed to aromatase inhibitors: one to letrozole and two to anastrazole. One of these patients has had a complete response and two have stable disease. Five-year actuarial survival was 65%, with no difference in survival between patients presenting with metastases and patients without metastases.21 Researchers at Sloan-Kettering Memorial Center reported that recurrent endometrial sarcomas treated with hormonal therapy had a 50% response rate and prolonged survival.10 One of the larger studies involved 20 LGESS patients; one patient received progestins after surgical resection and did not recur. Five patients who did not receive any adjuvant therapy recurred; two patients subsequently treated with progestins and chemotherapy survived versus three who were treated with radiation and died. Four patients in this series with stage III and IV LGESS received progestins and subsequently remained disease-free.8
Pink et al. reported on 10 patients with metastatic LGESS. Of the 10 patients, five were on oestrogen replacement therapy and three were on tamoxifen at the time of recurrence, again demonstrating the trophic effect of oestrogen on these tumours. Three patients were removed from oestrogen stimulation and remained stable, while two of three patients responded to progestins.7
Chu et al. reported on 22 patients with LGESS. Out of 22 patients, 10 patients recurred; of these 10, four had been on progestins and six had not. Subsequently, eight patients were put on progestins and seven of the eight responded to treatment.6 Another study looked at the treatment of 11 cases of metastatic or recurrent endometrial sarcomas with hormonal therapy: 10 of 11 responded or remained stable.13 These retrospective studies have consistently demonstrated a benefit to treatment of metastatic LGESS with hormone therapy. The most widely used agents in hormonal therapy are progestins, primarily medroxyprogesterone acetate and megestrol acetate, which function by downregulating ERs, increasing oestrogen metabolism, and inhibiting oestrogen-induced growth factors.5 LGESS that recur have been shown to regress or stabilise under progestin treatment and may undergo complete remission.7,10 Studies have also shown that progestins can prevent recurrences.5,6 High-dose progestin therapy may be associated with side effects, including weight gain, depression and thromboembolic episodes. To avoid the side effects associated with high-dose progestin treatment, other, newer drugs have been explored.
Aromatase inhibitors commonly used in breast cancer treatment have been applied to the treatment of LGESS. They reduce oestrogen by inhibiting oestrogen synthesis at peripheral sites. The early-generation aromatase inhibitors had many side effects, but third-generation drugs such as exemestane and letrozole and the steroidal aromatase inhibitor anastrazole have minimal toxicity. The dosages used for breast cancer treatment have been applied to off-label use in endometrial sarcomas.5 To highlight the effectiveness of these hormone treatments, it has been reported that two patients with lung metastases had complete remissions after treatment.22 Aromatase inhibitors are clearly effective and may be utilised primarily or as a potential second-line agent.3,5Tamoxifen is contraindicated as it has an actual agonist effect on endometrial stromal cells. Studies have repeatedly shown that patients who receive oestrogen replacement therapy or tamoxifen have a higher risk of recurrence. Also, endometrial sarcomas have been reported as a consequence of tamoxifen use in breast cancer treatment.5,7
Leuprolide is an example of the GnRH analogues that have been used in the treatment of pre-menopausal patients with endometriosis and those with breast cancer. These drugs reduce and suppress ovarian oestrogen production.5 Studies have shown successful reduction of stage I sarcomas with treatment.23 All of these studies provide positive data to support the use of hormonal therapy for the treatment and prevention of recurrences. Although there are no guidelines developed for the optimal drug, dose and time-frame for usage, it may be reasonable to use hormone therapy for all surgically resected receptor-positive LGESS, as commonly applied in breast carcinoma.
Conclusion
Endometrial stromal sarcomas are interesting and uncommon tumours of the uterus. Guidelines in terms of recommended treatment remain problematic, given the paucity of cases. It is advisable to test all tumours for OR and PR since this forms the basis for hormonal treatment. Patients with advanced-stage or metastatic LGESS should be treated post-operatively with hormonal treatment. Choices include progestins or aromatase inhibitors. If progression occurs, patients can be crossed over to another agent. At this time it is unclear whether patients with stage I tumours benefit from adjuvant treatment; lowdose progestins or close observation both seem to be reasonable options. Follow-up should be continued indefinitely, as recurrences often occur many years later. ■