Although the majority of worldwide bladder cancer patients presented with disease confined to the superficial layers of the bladder wall, approximately one-quarter of patients will present with or subsequently develop invasive cancer. In Egypt, these invasive stages represent 80 95% of the whole population of bladder cancer patients. Moreover, patients who underwent radical cystectomy of the superficial tumor (P0) represented 0.3% of the 4,541 total patients compared with 20.2% of 1,054 patients in the US.Advanced stages (P2b, P3 and P4) accounted for 81.5% and 94.5% in the studies by Ghoneim et al. and Zaghloul et al. respectively, compared with 49.1% in that of Stein et al. Locally advanced bladder cancer portends a poor prognosis. In Europe, physicians have favored radiation and chemotherapy, whereas in North America, Egypt, and other parts of the world the direction is toward surgical extirpation.
The relative frequency of transitional cell carcinomas (TCC) in cystectomy specimens increased in the National Cancer Institute (NCI), Cairo from 30.5% in the period 1988 1991 to 44.1% in the period 1998 2001, minimizing the differences between bilharzial (schistosomal) and non-bilharzial categories. The differences between bilharzial and non-bilharzial series were mainly the younger age at presentation, late presentation, larger size of the tumor and mucosal inflammation due to bilharzial infestation and deposition of eggs, which may affect the response to therapy and the bladder extension capability.Not much difference was proven in the natural history or in the method of spreading. Radical Cystectomy
The treatment of choice for muscle invasive bladder cancer remained radical cystectomy for decades. This procedure includes removal of the bladder, seminal vesicles, and prostate together with perivesical fat in addition to bilateral endopelvic lymphadenopathy in male patients. In female patients, the same bilateral endopelvic lymphadenopathy together with removal of the bladder, its perivesical fat, and peritoneal covering, urethra, uterus, ovary, and anterior wall of the vagina (anterior pelvic excenteration). Many studies had reported favorable results (higher than 60% five-year survival) for patients with pathologically organ-confined disease. However, the results were significantly worse when reporting upon locally advanced (P3N0, P4aN0 or with pelvic nodal involvement). These worse results were found in both bilharzia-associated and nonassociated bladder cancer when compared stage by stage. Similar results were also reported when comparing the same stage in urothelial (transitional, TCC) and nonurothelial (non-transitional, squamous or adenocarcinoma) tumors (see Table 1). Rogers et al. reported five-year progression-free survival of 60% ± 2% after radical cystectomy for TCC and 55% ± 11% for squamous cell carcinoma (SCC).These results remained statistically significant in patients with organ-confined and non-confined disease both in univariate and multivariate analyses.They reported worse results upon adenocarcinoma and other non transitional, nonsquamous tumors. Most of the publications concerned with primary bladder adenocarcinoma reported upon small numbers of patients with short-term follow up. These were too little to investigate and conclude the proper treatment of such pathologic category. Radical cystectomy with or without adjuvant therapy has been reported by several authors as the treatment of choice in TCC. These published studies reported that five-year disease free survival ranged from 0% to 80%. The relatively small number of patients with non-urothelial bladder cancer in the Western publications precluded the stratification of outcomes by pathological stage for these subtypes. However, two Egyptian publications recently reported on large numbers of patients (185 and 192 patients) and showed that adenocarcinoma treated with radical cystectomy with or without adjuvant postoperative radiotherapy (PORT) had similar five-year disease-free results as TCC and SCC of the bladder. However, a special subcategory of bladder adenocarcinoma, signet-ring, has dismal results. Zaghloul et al. reported upon 14 signet-ring category cases among 192 adenocarcinoma patients. They experienced statistically significant worse results than the other patients. Radical cystectomy results were not affected by patients sex, age, tumor histology (TCC, SCC, or adenocarcinoma), or etiology, but were affected by other prognostic factors.
Prognostic actorsafter Radical Cystectomy
Some authors consider pathological stage as the sole determinant of the patient prognosis after surgery, yet the majority consider it as the most important prognostic factor after radical cystectomy. Pelvic nodal involvement was also identified as a very strong independent prognostic factor. Nodal involvement led to five-year survival rates ranging between 4% and 35%, which was much lower than in patients with uninvolved nodes (see Table 1).
* 10-year all-cause survival.
** 48% of patients received neoadjuvant or adjuvant radiotherapy and/or chemotherapy.
*** 24% of patients received post-operative radiotherapy. TCC = transitional cell carcinoma, SCC = squamous cell carcinoma, Aden = adenocarcinoma.
It was found that the extent of this nodal involvement determines the survival rate, as the five-year survival rate decreases from 44% to 27% and 0% in N1, N2, and N3 patients, respectively. Moreover, it was proven that the proportion of involved out of the dissected nodes determines the survival rate. It was shown in several prospective and retrospective studies that both the extent of lymphadenectomy and number of dissected nodes determine the survival rate even in negative-node patients. Few studies have included tumor size in the analysis of prognostic factors affecting bladder cancer end-results. Cheng et al. showed that tumor size has a significant effect in determining distant metastasis-free, cancer-specific, and all-cause survival both in the univariate and multivariate analyses. However, Pollack et al. found that the size had no influence on distant metastasis. The cut-off size remained logistically and practically as an important point to be determined. The histological grade had a significant prognostic effect in many studies, yet other studies failed to prove its effect. Similarly, lymphovascular invasion (LVI) had a controversial effect as an independent prognostic factor in different studies. On the other hand, Lotan et al. showed that LVI has its prognostic effect restricted to the node-negative patients.Wider controversy was reported for the effect of tumor angiogenesis. Several studies confirmed the ominous prognostic significance of angiogenesis in TCC, squamous cell (SCC), and adenocarcinoma of the bladder. Others reported a better survival with high angiogenic activity or failed to show any effect on survival. Recently, P53 and P21 were shown to be strong predictors of disease outcome in post-operative multivariate models that adjusted for the effects of other cell cycle regulators and standard pathologic features. The absence of heterogenous retinoblastoma (Rb) gene expression was an independent marker of worse survival compared with positive Rb expression. Prognostic Grouping and Nomogram
Many predictive models for different malignant tumors have been previously reported. For bladder cancer there were attempts to identify prognostic models for prediction of distant metastasis and local control rates in patients treated with radical cystectomy, with or without radiation therapy. Rafla et al. suggested these prognostic models depending upon recurrence at one year. Zaghloul could determine the probability of developing distant metastasis using multivariate analysis and depending upon three independent factors. These factors were pelvic lymph nodal involvement, pathological stage, and histologic grade. It was found that this identified prognostic index also determined the level of local control in a statistically significant way. Furthermore, it was found that the effect of this prognostic index was constant in the three treatment groups included in the study (cystectomy alone, preoperative, and PORT). Ghoneim et al. and Khaled et al. reported on a prognostic model and prognostic index for both disease-free and overall survival for patients who underwent radical cystectomy. Though these traditional prognostic groupings have provided useful estimates for recurrence risk and survival outcomes, significant variation within each prognostic group has been observed. The observed variation in outcomes is related to the heterogeneity of tumor biology and patient characteristics within each pathologic subgroup. More importantly these prognostic models were found to be capable of simultaneous evaluation of multiple relevant variables to provide improved estimates of outcome that can be applied to an individual patient.
The international bladder cancer nomogram consortium has collected the data of 9,064 patients from 12 centers worldwide. A nomogram was drawn for bladder cancer patients, both superficial and invasive, who underwent radical cystectomy through combining the data into a relational database formatted within patient characteristics, pathologic details of preand post-cystectomy specimens and recurrence and survival rates.The ultimate goal of this nomogram was to aid clinicians in predicting the probability of progression after radical cystectomy and to identify patients at high risk who are in need of adding adjuvant therapy after surgery. This nomogram uses a simple 100-point scale. It is worth nothing that the institution that contributed the most patients to the model was Mansoura University in Egypt where 1,115 of 2,136 (52%) of the patients had SCC on top of bilharziasis. Moreover, SCC was diagnosed in 1,306 (14.4%) and adenocarcinoma in 320 (3.5%) of the whole population collected in the 12 centers. Individual institutional validation was assessed and verified within the nomogram. None of the 12 centers were different in the cohort of this nomogram.
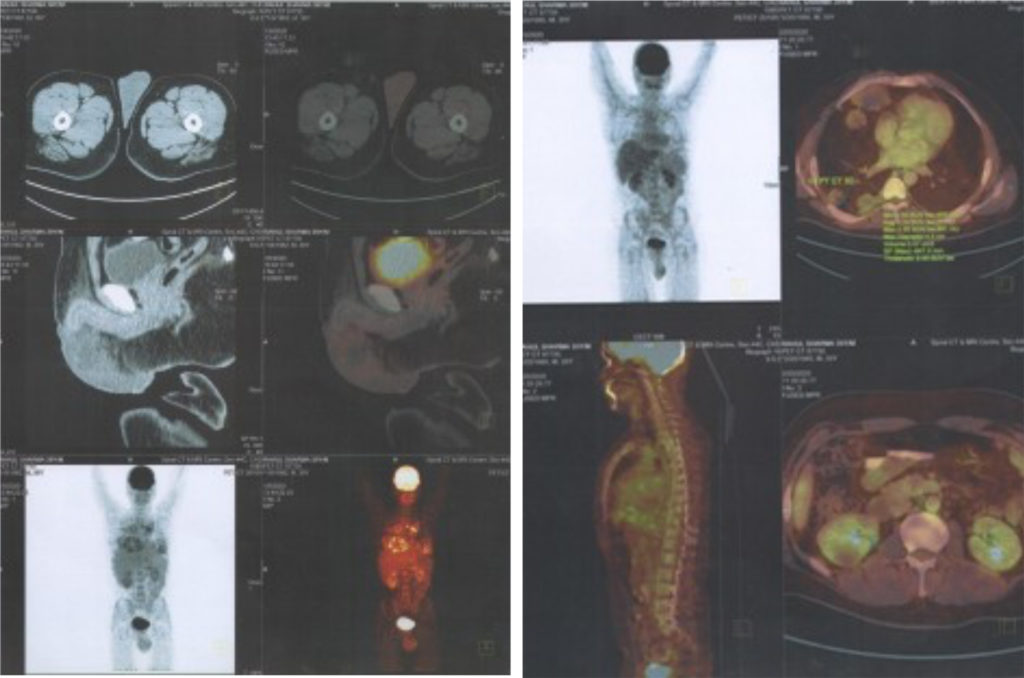
Causes of Treatment Failure After Radical Cystectomy
In modern days, post-operative mortality is limited to the level of 1–4%.The main causes of treatment failure were distant metastasis, local recurrence and other systemic causes. Before the computed tomography (CT) era, local recurrence after radical cystectomy was rarely detected. Furthermore, local recurrence rates were probably under-reported because the finding of distant metastasis decreased the need for intensified local follow-up when local recurrences are asymptomatic. Moreover, many investigators did not report local recurrence except if it was the only site of relapse, probably for the same reason. Recent studies have indicated that local recurrence was much more frequent than previously believed. Recurrence with or without distant metastasis was found in 5–31% of patients treated with radical cystectomy, depending on their clinical and pathological features. In patients with PT3 and PT4 disease, the rate of local recurrence was reported to be around 30%. This five-year local recurrence rate increased with higher stage and it achieved 11%, 23%, and 31% for stages II, III, and IV respectively. In another study, the 10-year local recurrence rate was reported to be 25% for PT3, 51% for PT4, and 49% in node-positive patients. Similar results were reported earlier by the Egyptian (schistosoma-associated) series. Furthermore, local recurrence presented early, mainly within the first year, and located in the pelvis (within the vicinity of pelvic irradiation); there were minimal differences in determining risk factors. These high incidence rates emphasized the need for adjunctive local therapy in trials to deal with this recurrence.
TCC= transitional cell carcinoma, SCC= squamous cell carcinoma, Aden=adenocarcinomas, NM= not mentioned.
Cyst= cystectomy alone, HF= hyperfractionation, CF= conventional fractionation, PORT= post-operative radiotherapy, NM= not mentioned.
Pre-operative Radiotherapy
Pre-operative radiation was tried as early as the 1970s. The rationale for the use of pre-operative radiotherapy is to prevent intra-operative seeding of tumor cells in the operative field and to sterilize microscopic deposits in the perivesical tissues. Many retrospective studies proved the benefit of preoperative radiotherapy in bladder cancer. Whitmore and Batata showed improved survival rate (42% versus 33%) and a marked reduction in the pelvic recurrence rate (20% versus 37%) in patients treated with preoperative radiotherapy compared with historical control treated with cystectomy alone. Parsons and Million concluded that pre-operative radiotherapy resulted in a 15–20% survival advantage in T3 bladder cancer patients after they compiled the data from a number of non-randomized studies. However, only one out of the six randomized trials published in English-language literature showed a significant difference in the two-year disease-free survival as a result of adding pre-operative radiotherapy.This study, undertaken in Egypt, had the advantage of restricting the randomization to T3 categories, while the other five randomized trials, including another Egyptian series, treated either all stages or the T2 category which masked the beneficial effect expected in the advanced stages (see Table 2).
Awwad et al. performed a study on 48 patients randomized into three treatment groups. Radical cystectomy was compared with two pre-operative radiotherapy regimens—conventional 4,000cGy/five weeks or hyperfractionated 4,080cGy/11 days/37 fractions. The two-year disease-free survival rates were 53% ± 9% in patients receiving pre-operative radiotherapy compared with 19% ± 10% for the cystectomy alone group. The same beneficial effect of pre-operative radiotherapy was also noted in the study by Ghoneim et al. in patients with advanced stages and advanced grades. The five-year survival rates for PT3 and PT4 patients were 43% when treated with preoperative radiotherapy (2,000cGy/one week) compared with 19% when the same category of patients were treated with cystectomy alone. On the other hand, there were no differences in the earlier stages (PT1 and PT2) as the five-year survival rates were 54% and 67%, respectively. In the other studies down-staging was associated with improved survival rates. Meta-analysis of these six randomized trials demonstrated a corrected odds ratio of 0.94 (95% confidence interval (CI), 0.57–1.55), indicating no benefit of the studied pre-operative irradiation collectively. Using chemotherapy (cisplatin) as a radiosensitzer given concomitantly with pre-operative 4,000cGy pre-operative radiotherapy was tried in a phase II trial. The two-year overall survival was 75% while the local recurrence was as low as 16%. Distant metastasis was experienced in another 16% of patients.
Post-operative Radiotherapy
PORT has the advantage of dealing with microscopic cells that are easier to sterilize. Better identification of the group of patients that may benefit from this adjuvant therapy is fulfilled with post-operative irradiation. However, it still has two dose-limiting tissues: the early reacting intestinal epithelium and the late responding connective tissues in and around the uretero–intestinal and intestino–intestinal anastamoses. A large prospective randomized trial proved the beneficial effect of PORT in locally advanced bladder cancer patients. The five-year disease-free survival was 49% and 44% for hyperfractionated and conventional PORT, respectively, compared with 25% for cystectomy alone. This effect was consistent in all tumor types, all stages and grades and whenever pelvic lymph nodes were not involved. These results could be replicated in the non-randomized controlled Radiation Therapy Oncology Group (RTOG) trial, Cozzarini et al. trial, and other Egyptian series (for patients having TCC, SCC and adenocarcinoma) (see Table 3). Reisinger et al. treated 78 patients with combined pre-operative 500cGy single treatment on the day of the operation and 4,500cGy/five weeks post-operatively.They restricted PORT to patients proved pathologically to have P2 high grade, P3 and P4a (40 patients). Though this study was a single arm non-randomized trial it reached to the same results as the Zaghloul et al. study when compared stage by stage. The effect of PORT was constant in all pathological stages and whenever pelvic nodes were negative; however, this effect was lacking in node-positive patients (though of better local control).This was explained mainly by the high incidence of distant metastasis. However, PORT in bladder cancer remained unpopular due to the fear of late intestinal complications. Warning results were published by Reisinger et al. as they reported intestinal obstruction in 15 of 40 (37%) patients who received PORT. Nine out of those 15 patients required surgery and three died. On the contrary, Zaghloul et al. found 14 (18%) out of 78 patients treated with conventional PORT and four (5%) out of 75 patients treated with hyperfractionation PORT experience chronic enteritis of different grades. Only three (4%) and four (5%) of conventional and hyperfractionation patients, respectively, progressed to fistulae that necessitated surgery. Similar levels of complication were experienced by adenocarcinoma patients treated with PORT. The difference between the latter two studies and that of Reisinger et al. was probably due to the larger volume of radiation used in the Reisinger et al. study, which led to more-severe late bowel complications though a similar disease-free survival, when compared stage by stage. Adjuvant therapy for bladder cancer succeeded in decreasing the local recurrence to a great extent; however, the other causes of failure emerged as important obstacles for further improvement of survival. Careful attention to radiation planning and delivery, as well as selection of the patients suitable for adjunctive radiotherapy helps to determine the value of these modalities. The use of small radiation dose per fraction decreased the late complication rates significantly. Distant metastasis had been highlighted as an important cause of failure after improvement of local control. This level of distant metastasis differed according to tumor stage, grade, and the status of pelvic nodal involvement.
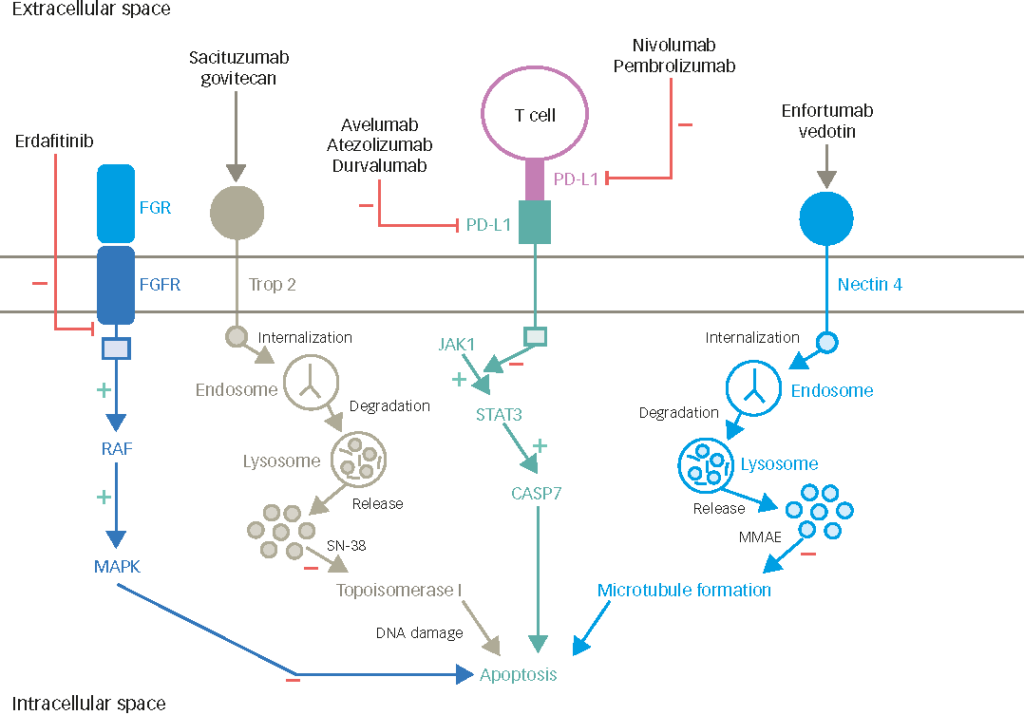
Adjuvant Local and Systemic Therapy
The high incidence of distant metastasis in both bilharzial and non-bilharzial bladder cancer raised the issue of importance of adjuvant systemic treatment.A prospective controlled randomized trial was performed to test the tolerability and efficacy of adding adjuvant chemotherapy (gemcitabine and cisplatinum) to PORT in a phase III study.This regimen, given with hyperfractionated PORT (4,500cGy/three weeks/30 fractions) as an adjuvant combination to surgery, proved to be tolerable and the percentage of grade III and IV toxicities were minimal. A total of 142 high-risk (PT3, PT4, grade 3 and/or positive nodes) bladder cancer patients were randomized. Preliminary results showed improvement of two-year disease-free survival in the adjuvant chemoradiotherapy group though not reaching the level of significance. Patients with one risk factor, lower pathological stage or no nodal involvement seemed to benefit more from the added chemotherapy.