Chemotherapy in Metastatic TCC
MVAC
The methotrexate, vinblastine, doxorubicin, and cisplatin (MVAC) regimen, developed at Memorial Sloan-Kettering Cancer Center in the 1980s, represented a major advance in the treatment of metastatic TCC. In the initial report, 24 patients with advanced or unresectable TCC were treated and responses were observed in 71% (95% confidence interval (CI), 53–89%), with complete responses in 50% (95% CI, 30–70%). Subsequent reports in larger patient populations confirmed the activity of this regimen, albeit with slightly lower response rates, and a series of randomized trials conducted during the late 1980s to early 1990s established MVAC as a treatment standard for advanced TCC (see Table 1).
Despite the superiority of MVAC in randomized trials, the limitations of this regimen were readily apparent. Treatment with MVAC was associated with significant toxicities including mucositis, febrile neutropenia, nephrotoxicity, otototoxicity, and neuropathy. As a result, during the past decade, efforts focused on integrating newer chemotherapeutic agents into the treatment of advanced TCC in an attempt to improve upon MVAC in terms of both efficacy and tolerability. Trials evaluating single-agent therapy with gemcitabine, the taxanes, and ifosfamide demonstrated promising activity and led to the development of multiagent regimens, several of which have been compared with MVAC in randomized trials (see Table 1). Gemcitabine Plus Cisplatin and Other Cisplatin-based Doublets and Triplets
A landmark phase III trial randomized 405 patients to gemcitabine plus cisplatin (GC) versus MVAC. This trial was not designed as a non-inferiority trial. Nonetheless, the response rates and median survivals were similar on both arms. Further, MVAC was associated with a greater incidence of neutropenic fever, neutropenic sepsis, grade ?3 mucositis, and treatment-related deaths. Based on this trial, gemcitabine plus cisplatin has become a widely utilized treatment standard for metastatic TCC. Several other cisplatin-based doublets and triplets have also been explored. In a randomized phase III trial, docetaxel plus cisplatin (DC) was compared with MVAC. Although DC was better tolerated, response rates and survival favored treatment with MVAC. Phase II trials exploring the triplet combinations of gemcitabine, cisplatin, plus paclitaxel (GCT) and ifosfamide, cisplatin, plus paclitaxel have shown promising activity.A recently completed randomized phase III study evaluated gemcitabine plus cisplatin ± paclitaxel; the results of this study are eagerly awaited.
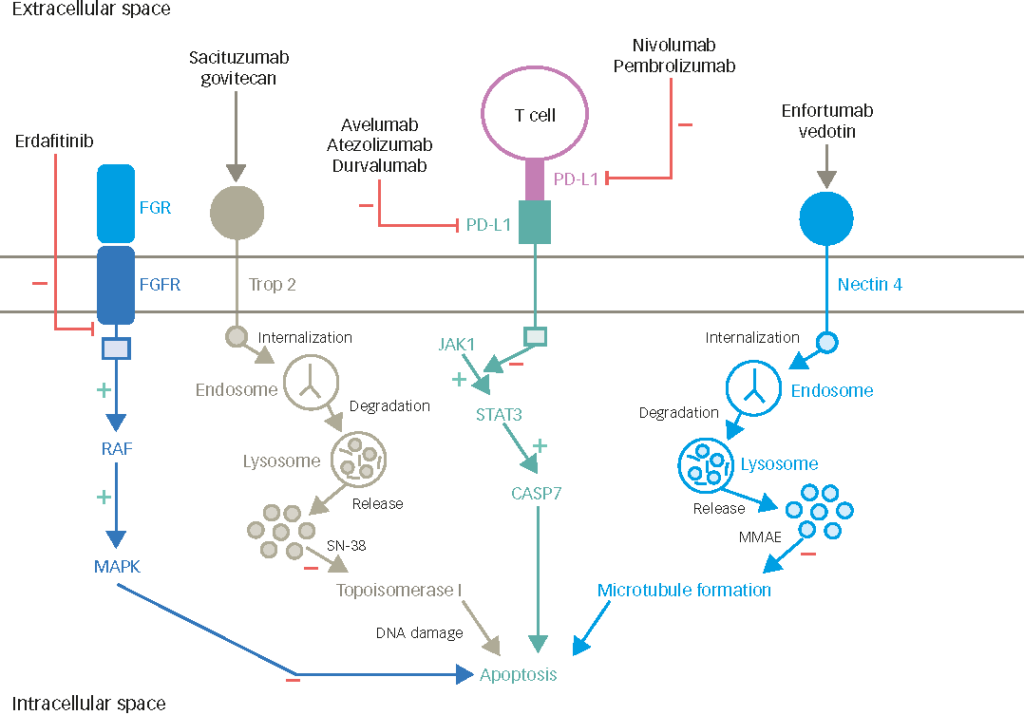
Integration of ‘Targeted’ Agents
Current efforts are focused on integrating agents targeting novel pathways known to be important in the pathogenesis of TCC.A multicenter phase II trial led by Hussain et al. evaluated the monoclonal antibody trastuzumab given in combination with paclitaxel, carboplatin, and gemcitabine. Of the 109 patients registered, 59 were eligible for treatment based on human epidermal growth factor-2 (HER-2) overexpression. There were 32 responses (five complete and 27 partial, overall response rate 72.7%) and the median survival of patients treated was 15.2 months. The contribution of trastuzumab to the efficacy of this triplet cytotoxic regimen is unclear based on the single-arm design of this trial. The combination of gefitinib, cisplatin, and gemcitabine has been explored by the Cancer and Leukemia Group B (CALGB). The preliminary results with this regimen did not suggest a substantial improvement upon historical results with gemcitabine plus cisplatin alone. On-going trials are exploring anti-angiogenic agents and histone deacetylase inhibitors in advanced TCC.
MVAC = methotrexate, vinblastine, doxorubicin, cisplatin; CISCA = cyclophosphamide, cisplatin, doxorubicin; CMV = cisplatin, methotrexate, vinblastine; MV = methotrexate, vinblastine; FAP= 5-fluorouracil, interferon-alpha-2b, cisplatin; HD-MVAC = high-dose MVAC; OR = overall response; CR = complete response. *Trial closed early with only 85 patients.
Cisplatin-ineligible Patients
As many as 40% of patients with TCC are ineligible for cisplatin-based therapy due to impaired renal function. Therefore, carboplatin-based regimens have been extensively explored (see Table 2). There have been no phase III trials designed to specifically address the equivalence of carboplatin and cisplatin in the treatment of TCC. The Eastern Cooperative Oncology Group (ECOG) initiated a phase III trial comparing MVAC with paclitaxel plus carboplatin; however, this study was terminated after 2.5 years due to poor accrual. In randomized phase II studies, higher overall and complete response rates have generally been reported with cisplatin-based regimens compared with carboplatinbased regimens. In patients with contraindications to cisplatin, the doublets of gemcitabine plus carboplatin or paclitaxel plus carboplatin are commonly utilized. An ongoing European Organisation for Research and Treatment of Cancer (EORTC) phase III trial is comparing the regimen of methotrexate, vinblastine, and carboplatin with gemcitabine plus carboplatin in cisplatin-ineligible patients with metastatic TCC.
OR = overall response; CR = complete response; CI = confidence interval; AG →TC = doxorubicin plus gemcitabine followed by paclitaxel plus carboplatin; NR = not reported. *Trial limited to patients ineligible for cisplatin-based therapy.
Second-line Chemotherapy
There have been no completed randomized phase III trials exploring the efficacy of second-line chemotherapy in patients with advanced TCC. Multiple small phase II trials exploring a variety of agents have been performed. Overall, the most active of these agents have shown response rates of approximately 10–30% (see Table 3). Based on promising phase II data, a phase III trial was initiated comparing vinflunine with placebo as secondline therapy in patients with metastatic TCC. Prognostic Factors in Metastatic TCC
Pre-treatment clinical variables have been explored in an attempt to predict the outcomes of patients with advanced TCC treated with chemotherapy. In a retrospective analysis of 203 patients with unresectable/ metastatic TCC treated with MVAC, two factors had prognostic significance: Karnofsky performance status (KPS) ?80% and visceral (lung, liver or bone) metastases. The median survival for patients with no, one, or two risk factors was 33, 13.4, and 9.3 months, respectively (p=0.0001). Consideration of the proportion of patients in these various risk categories is critical when comparing the outcomes of patients treated on independent phase II studies. These baseline prognostic factors should also be used to stratify patients in phase III trials comparing new regimens with standard therapy.
OR = overall response, CI = confidence interval. *90% upper limit 29%.
Post-chemotherapy Surgery in Metastatic TCC
The benefit of post-chemotherapy surgery to resect initially unresectable or metastatic TCC has been explored in several analyses. In a series of 203 patients treated with MVAC, 50 patients underwent postchemotherapy resection of residual disease. No viable tumor was found at the time of surgery in 17 patients. Three patients had unresectable disease at the time of exploration. In the remaining 30 patients, residual disease was completely resected, resulting in a complete response to chemotherapy plus surgery.Ten of these 30 patients (33%) were alive at five years, similar to results attained for patients achieving a complete response to chemotherapy alone. Optimal candidates for postchemotherapy surgery have pre-chemotherapy disease limited to the primary site or lymph nodes and achieve a ‘near’ complete response to chemotherapy. Peri-operative Chemotherapy for TCC
Approximately 50% of patients with muscle-invasive TCC undergoing radical cystectomy will develop metastases and succumb to their disease. Given the chemosensitive nature of TCC, attempts to improve survival in patients with locally advanced disease have focused on administering chemotherapy in the perioperative setting.
Neoadjuvant Chemotherapy
There are several advantages to administering chemotherapy prior to surgery. Chemotherapy is arguably better tolerated in the pre-operative versus post-operative state. Further, the response of the primary bladder tumor to chemotherapy can be assessed, which is of prognostic significance. For example, in one study of neoadjuvant chemotherapy, 91% of patients who responded to chemotherapy (defined as pathologic stage ?T1) were alive at a median follow-up of 25 months compared with 37% of patients who did not respond to chemotherapy.The benefit of neoadjuvant chemotherapy in the treatment of TCC has been explored in several randomized trials (see Table 4). While many of these did not show a benefit, these ‘negative’ trials suffered from inadequate sample size, inferior chemotherapy, early closure, or short follow-up. In the past decade, welldesigned adequately powered trials have shifted the treatment paradigm in muscle-invasive disease toward the standard use of neoadjuvant chemotherapy.
MRC = Medical Research Council, EORTC = European Organization for Research and Treatment, INT = United States Intergroup, GUONE = Gruppo Uro-Oncologico del Nord Est, CUETO = Club Urologico Espagnol de Tratiemneto Oncologico, MGH = Massachussetts General Hospital, RTOG = Radiation Therapy Oncology Group, USC = University of Southern California, M = methotrexate, C = cisplatin,V = vinblastine, A = doxorubicin, E =epirubicin, Cyst = cystectomy, RT = radiation therapy. *Benefit for subset with T3–T4.
In a US intergroup trial, patients with T2–T4a TCC of the bladder were randomized to radical cystectomy alone versus three cycles of MVAC followed by radical cystectomy. Patients randomized to neoadjuvant MVAC experienced a significantly higher rate of complete pathologic response (38% compared with 15%, p <0.001). At a median follow-up of 8.7 years, improvements in median survival (77 compared with 46 months, p=0.06) and five-year survival (57% compared with 43%, p=0.06) favored the neoadjuvant chemotherapy arm. Importantly, neoadjuvant chemotherapy did not adversely impact the ability to proceed with surgery or increase adverse events related to radical cystectomy.
The Medical Research Council (MRC)/EORTC performed a large trial in which 976 patients were randomized to neoadjuvant cisplatin, methotrexate, and vinblastine (CMV) followed by local management of the primary tumor versus local management alone. In this trial, management of the primary tumor was left to the discretion of the treating physician and could include cystectomy, radiation therapy, or both. At a median follow-up of approximately seven years, a statistically significant improvement in survival was observed for patients who received neoadjuvant CMV (p=0.048; hazard ratio (HR), 0.85; 95% CI, 0.72–1.0). A metaanalysis, including data from 2,688 patients treated on 10 randomized trials, has further substantiated the benefit of neoadjuvant chemotherapy. Compared with local treatment alone, neoadjuvant cisplatin-based combination chemotherapy was associated with a significant benefit in overall survival (HR, 0.87; 95% CI, 0.78–0.98; p=0.016), a 13% decrease in the risk of death, and a 5% absolute survival benefit at five years.
Adjuvant Chemotherapy
There are also potential advantages and disadvantages to administering chemotherapy after surgery. The most cited advantage is the ability to make decisions regarding the need for peri-operative systemic therapy based on pathologic staging. Given the inaccuracies in clinical staging, this prevents ‘over-treatment’ of patients estimated to have a favorable outcome from surgery alone.Administration of chemotherapy post-operatively also theoretically avoids a delay in potentially curative surgery during the administration of potentially ineffective systemic therapy. The major disadvantages associated with post-operative chemotherapy are the difficulties of tolerating systemic treatment after major surgery and the lack of prognostic information gained by evaluating the response in the primary tumor. Several randomized trials have evaluated the use of adjuvant chemotherapy following cystectomy for TCC (see Table 4).These trials were generally underpowered, employed heterogeneous chemotherapy regimens, and some included primarily patients with bladderconfined disease. As a consequence of these flaws, the data supporting adjuvant chemotherapy are less compelling than the data supporting neoadjuvant chemotherapy. To definitively address this issue, the EORTC is randomizing patients with pT3–T4 or node-positive disease after cystectomy to immediate cisplatin-based chemotherapy (MVAC or GC) or similar chemotherapy at the time of relapse.
Conclusions
Over the past two decades, several multi-agent chemotherapy regimens with activity in TCC have been introduced. Based on phase III data, GC or MVAC is recommended for patients with metastatic TCC who are candidates for cisplatin-based therapy. Two large randomized trials and a meta-analysis support the use of neoadjuvant cisplatin-based combination chemotherapy prior to radical cystectomy for patients with muscleinvasive bladder cancer. Despite these advances, there is substantial room for improvement in the outcomes of patients with locally advanced and metastatic TCC. Enrollment on a well-designed clinical trial should always be considered for eligible patients.