First-line Treatment of Unfit Bladder Cancer Patients – An Overview
In the first-line setting treatment of unfit bladder cancer patients, a long list of small phase I, II and III trials investigating various combinations of chemotherapy regimens is available (see Table 1). Most data are on gemcitabine-based combinations, such as GCa, which is probably the best currently available regimen in unfit patients, despite its flaws. For instance, in the European Organisation for Research and Treatment of Cancer (EORTC) phase III 30986 trial, it became apparent from phase II onwards that GCa was superior to carboplatin, methotrexate and vinblastine (M-CAVI).1,2 Other combination regimens have been tested, including paclitaxel combined with carboplatin or gemcitabine, with or without platinum salts. It remains difficult to say with certainty which regimen should be the reference in unfit patients. At best, overall response rate (ORR) values are approximately 30–40 %, with median overall survival (OS) rarely exceeding 10 months (see Table 1).3–10 In addition, sequential regimens have been explored in phase II trials (see Table 2). Treatment with doxorubicin plus gemcitabine followed by paclitaxel plus carboplatin was studied by Galsky et al.,11 and a recent trial has explored whether bevacizumab, a monoclonal antibody against vascular endothelial growth factor (VEGF), could be safely added to GCa and improve outcomes.12 It is, however, not known whether anti-angiogenic agents have a role in bladder cancer. The available data for bevacizumab are always on top of other chemotherapy regimens, so it is difficult to single out the specific contribution of these drugs (see Table 2).
In terms of the use of single agents in first-line unfit patients ineligible for cisplatin, both gemcitabine and sunitinib have been tested, with modest response rates and survival outcomes (see Table 3).10,13
Only one phase III study in unfit bladder cancer patients has been conducted, evaluating GCa versus M-CAVI (the EORTC 30986 trial)1 as discussed. Briefly, in OS or progression-free survival (PFS) the trial showed no significant differences. The only significant difference in efficacy favouring GCa was observed with ORR. Nevertheless, safety clearly favoured GCa versus M-CAVI. The interpretation is that GCa should be favoured in this setting as a reference regimen, although it is not firmly established whether carboplatin has a true role on top of gemcitabine for these unfit patients in the first-line setting.
European Guideline Recommendations
The European Society for Medical Oncology (ESMO) guideline recommendations for first-line treatment in cisplatin-unfit patients14 highlight that about 50% of patients are unfit for cisplatin-containing chemotherapy due to a poor performance status (PS), impaired renal function or comorbidity. These patients may be palliated with a carboplatin-based regimen or single-agent taxane or gemcitabine. Based on the EORTC 30986 study, severe acute toxicity was slightly higher on M-CAVI, which makes CGa the preferred and reference treatment in unfit patients. Patients with PS 2 and impaired renal function and unfit patients in Bajorin prognostic group 2 have limited benefit from combination chemotherapy, and new strategies are needed.14 The European Association of Urology (EAU) guideline recommendations for first-line treatment in patients ineligible or unfit for cisplatin15 are to use carboplatin-based chemotherapy (preferably GCa), or a single-agent regimen (see Table 4).
Depending on the number of adverse factors to qualify patients for the unfit group, the EAU guidelines have devised a treatment algorithm for the management of metastatic urothelial cancer. In patients with PS 2 and impaired renal function (glomerular filtration rate [GFR] <60 ml/minute), combination chemotherapy is said to provide limited benefit.15 As a reminder, the proposed consensus definition of unfit patients by Galsky et al. for eligibility in clinical trials included at least one of the following: WHO or Eastern Cooperative Oncology Group (ECOG) PS 2 or Karnofsky performance score (KPS) of 60–70 %, creatinine clearance (CrCl) <60 ml/minute, CTCAE v4 grade audiometric hearing loss of ≥2, peripheral neuropathy of ≥ grade 2 and congestive heart failure (CHF) grade ≥3.16
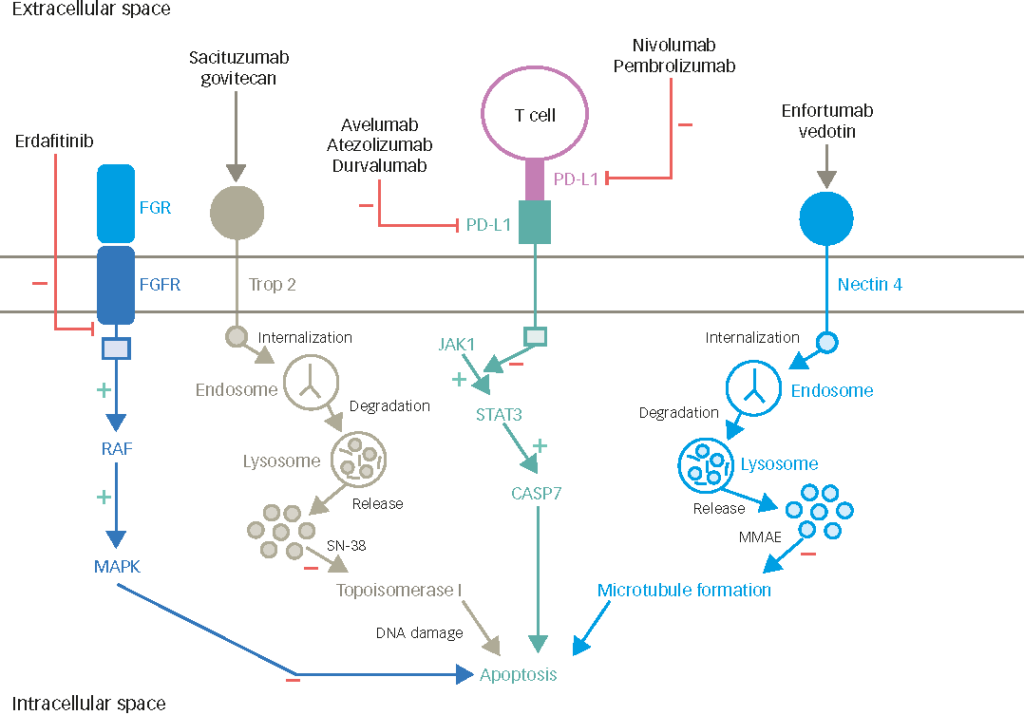
Integration of Targeted Agents – Angiogenesis Inhibitors in First-line Unfit Patients
There is a rationale for investigating angiogenesis inhibitors in bladder cancer. VEGF overexpression has been shown to correlate with poor prognosis, whereas microvessel density predicts N+ and survival.17 The first trial that reported a regimen in combination with angiogenesis inhibitors in first-line chemotherapy observed a very high response rate, but also very elevated toxicity. Randomised data are required to draw firm conclusions on whether or not these agents have a role in bladder cancer treatment. Several other agents are being evaluated in ongoing phase I/II trials, including everolimus and eribulin, as part of non-platinum-containing regimens being developed in the first-line treatment of patients ineligible to receive cisplatin (see Table 6).
Vinflunine Data and Perspectives
Phase I study data evaluating the combination of vinflunine with gemcitabine, carboplatin, doxorubicin, or methotrexate in non-small cell lung cancer (NSCLC), metastatic breast cancer or metastatic squamous cell carcinoma of the head and neck are ongoing or planned.
As discussed earlier in combination with cisplatin,18 the vinflunine plus gemcitabine or carboplatin combinations appear feasible, at least in NSCLC, with both drugs being used at full doses in each combination. As expected, haematological toxicity was the main toxicity with gemcitabine. No febrile neutropenia was reported with gemcitabine,19 but one case was observed with carboplatin (Pierre Fabre, internal data). If these data for vinflunine combination with gemcitabine or carboplatin are confirmed in bladder cancer, the combinations might be an option in unfit patients, specifically those with impaired renal function. More information will become available from the randomised JASINT phase II trial evaluating vinflunine plus gemcitabine versus vinflunine plus carboplatin in unfit bladder cancer patients with CrCl <60 ml/min or New York Heart Association (NYHA) II–III CHF (PS 0–1). In metastatic breast cancer, doxorubicin was explored in combination with vinflunine. As doxorubicin is an active drug in the bladder, this combination could also be a new alternative option. As expected for the two drugs, the most frequently reported grade 3/4 toxicities included neutropenia, nausea, constipation and stomatitis.20 Another option for combination with vinflunine in first-line unfit patients could be with methotrexate, which has also proven activity in bladder cancer. The rationale being that methotrexate is a component of the standard MVAC combination regimen in first-line, it is well tolerated and has been successfully combined with vinca alkaloids for the treatment of a variety of solid tumours including bladder cancer.21 It is a potentially attractive combination that could be easily managed.
There are so far no data on methotrexate in combination with vinflunine, but a phase I study in metastatic squamous cell carcinoma of the head and neck previously treated with platinum-based chemotherapy is planned.
Conclusions and Discussion
There are potential options for vinflunine use in the first-line setting for unfit patients. Vinflunine may be further developed and explored as a monotherapy. It could also confer benefit as part of a combination regimen: a series of possible promising combinations with carboplatin, split-dose cisplatin, metothrexate, doxorubicin or gemcitabine is being investigated in ongoing or planned trials. The patient profiles that would benefit the most need to be described in more detail.
The decision of which combination regimen to further develop in unfit patients (assuming that the objective is to demonstrate improved survival), depends on whether patients are mildly unfit, truly unfit or frail. In unfit patients, split-dose cisplatin could be considered combined with vinflunine. The most likely and appropriate comparator treatment in this case would be GCa. A retrospective study of split-dose cisplatin showed that OS was similar to GCa, but these data require confirmation. The problems with this potential treatment option is that there are no phase I data in combination with cisplatin in bladder cancer, or with split-dose cisplatin. Another limitation is that it is difficult to say how far to go with split-dose cisplatin in patients who have low CrCl. If split-dose cisplatin is not adopted, results from ongoing randomised phase II trials will hopefully address which would be the preferred regimen in terms of efficacy and tolerability. There is a good chance for gemcitabine plus vinflunine to be an attractive combination regimen. Other combinations with e.g. doxorubicin could be used, with some reservations, because unfit patients usually do not tolerate long-term chemotherapy, especially if the chosen regimen is associated with haematological toxicity. Regarding the proposed combination of methotrexate and vinflunine, because there is a clear synergistic effect between vinca alkaloids and methotrexate, perhaps a small phase II trial in bladder cancer could be tested in the second-line setting, or in unfit patients in the first-line setting.
In the discussion of future potential phase III development, improved OS is going to be a tall order in the first-line setting in unfit patients. Economic considerations for cancer drugs are becoming a concern in Europe, especially if no clear benefit in OS can be demonstrated. This should be borne in mind when planning phase III development. An alternative way of moving forwards would be to provide a chemotherapy regimen that would be easy to use, non-toxic and cheap. Gemcitabine requires a second infusion, and some patients experience haematological toxicity requiring transfusion. Thus, a study demonstrating that regimen every 3 weeks incorporating vinflunine in the outpatient clinic is cost-effective compared with, for example, GCa may be a different way of approaching the concern, providing a different line of argumentation that potentially incorporates cost-effectiveness and patient quality of life.