Introduction
Bladder cancer is the fourth most common type of cancer among men and the eighth most common among women. Each year more than 50,000 and 24,000 new bladder cancers are diagnosed in the US and in Germany, respectively.1,2 Patients with bladder cancer are treated for painless microhaematuria or gross haematuria in the absence of urinary tract infection (UTI) and/or irritative voiding symptoms.
Introduction
Bladder cancer is the fourth most common type of cancer among men and the eighth most common among women. Each year more than 50,000 and 24,000 new bladder cancers are diagnosed in the US and in Germany, respectively.1,2 Patients with bladder cancer are treated for painless microhaematuria or gross haematuria in the absence of urinary tract infection (UTI) and/or irritative voiding symptoms.
The gold standard for detecting bladder cancer is cystoscopy. Cystoscopy is a reliable investigation that identifies nearly all papillary and sessile lesions. It is an invasive procedure causing some discomfort for patients. At initial diagnosis, 65% to 70% of bladder cancers are confined to the urothelium (Ta, Tis) or invade the lamina propria (T1) and can be managed with endoscopic resection and intravesical therapy. Thirty per cent to 35% of newly diagnosed bladder cancers have invaded the detrusor muscle (T2–T4).3–5 Ta, grade 1 and grade 2 tumours recur in 30% to 70% and progress to muscle-invasive disease in less than 7% of patients. In contrast, high-grade stage T1 tumours have a progression rate of 30% to 50%.3–5 The high recurrence rate and the risk of progression necessitate follow-up care after treatment for bladder cancer at regular intervals. Follow-up protocols include cystoscopy every three months for one to two years, every six months for an additional two to three years and then annually.
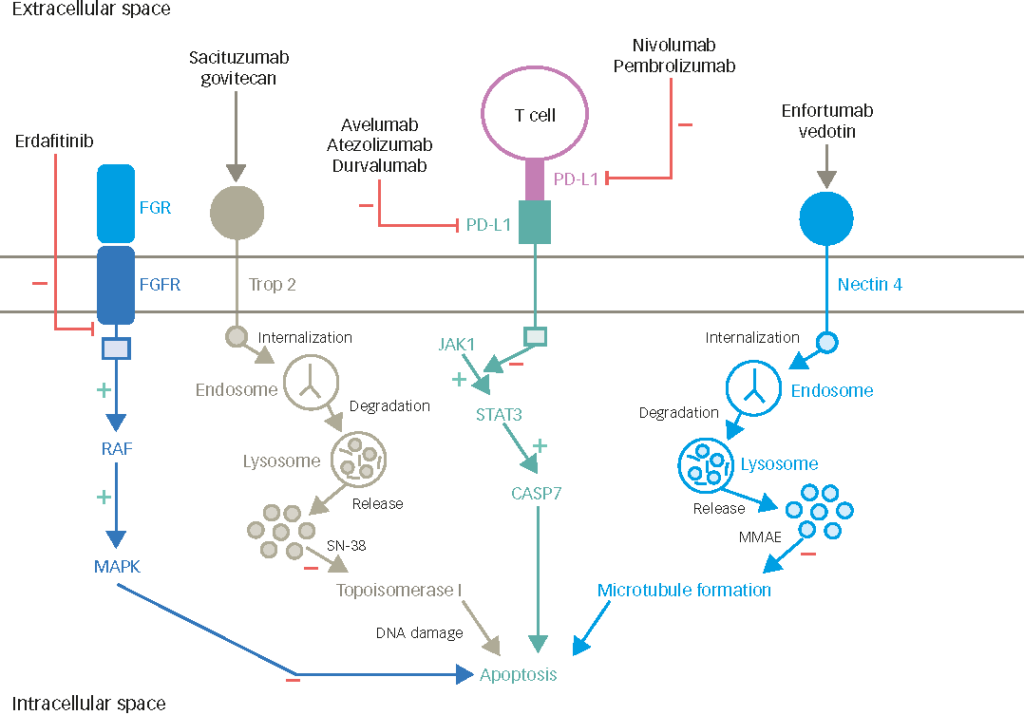
To improve early detection of bladder cancer, as well as to monitor treatment response and tumour recurrence, bladder tumour markers are critical. An ideal bladder cancer test would be non-invasive, highly sensitive and specific, inexpensive, easy to perform and yield highly reproducible results.6 The validity of a tumour marker test can be expressed as sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV). Sensitivity and specificity are terms in statistics for the probability of the identification of those with or without the condition (bladder cancer). PPV and NPV are terms for the probability of the usefulness of a test in identifying true positives or true negatives. Definitions of these are shown in Figure 1. An accurate tumour marker also would have the potential to replace or delay cystoscopy in the follow-up of bladder cancer patients. If the test for a bladder cancer marker accomplished these criteria, this would improve the quality of life of patients and decrease the cost of surveillance by substituting a less expensive test for a more expensive procedure.7 In recent years several non-invasive tests for tumour markers have been approved by the US Food and Drug Administration (FDA). In this article, literature on the commercially available tests for the diagnosis of bladder cancer – ImmunoCyt/uCyt+, BTA TRAK®, BTA stat®, NMP22®, NMP22 Bladder- Chek®, and UroVysion™ – are summarised.
Bladder Tumour Markers
Urine Cytology
Currently, urine cytology is the standard non-invasive marker. In a recent literature review, specificity of cytology ranged from 83% to 99.7% with a mean ± standard deviation (SD) of 99% and sensitivity ranged from 20% to 53% with a mean ± SD of 34%.8 The poor sensitivity of 15% both in Ta and G1 bladder cancers and of 46% in T1 tumours is unfavourable. Other reviews of published studies have shown similar results with an overall sensitivity of 35% to 49% and a specificity of 90% to 95%.7,9 Due to the poor diagnostic sensitivity for superficial and low-grade bladder cancers, cytology cannot replace cystoscopy. Furthermore, cytology is subjective and requires highly trained cytopathologists.
ImmunoCyt/uCyt+ test
The ImmunoCyt/uCyt+ assay (Diagnocure Inc., Québec, Canada) is an immunocytologic fluorescence assay in combination with voided urine cytology. Its evaluation requires an experienced cytopathologist. The assay identifies two different mucins and a high-molecular- weight glycosylated carcinoembryonic antigen (CEA) present in tumour cells originating from transitional epithelium. The mucins and CEA are tagged to the two monoclonal anti-mucin antibodies M344 and LDQ10 (14) and the monoclonal anti-CEA antibody 19A21110,11, which are labelled with fluorescein isothiocyanate (FITC) and Texas Red (TR), respectively. The ImmunoCyt/uCyt+ assay promises a higher diagnostic sensitivity than urine cytology. ImmunoCyt/uCyt+ has been demonstrated to have an overall sensitivity of 73% (range 39% to 100%) and an overall specificity of 80% (range 69% to 95%) (see Table 1).12–20 The PPV and NPV were 52% (range 39% to 63%) and 89% (range 81% to 97%), respectively (see Table 7).12,13,17,19 In the first study by Fradet et al.20 involving 198 patients with bladder cancer, ImmunoCyt/uCyt+ had an overall sensitivity of 90%, while overall sensitivity of urine cytology was 44%. Combined evaluation of ImmunoCyt/uCyt+ and cytology indicated 95% sensitivity. Specificity of ImmunoCyt/uCyt+ alone and in combination with cytology in 102 asymptomatic volunteers was 77%, whereas cytology alone had 100% specificity. These data were confirmed by the study pursued by Mian et al.,19 who diagnosed 264 consecutive patients including 79 with transitional cell carcinoma of the urinary tract. ImmunoCyt/uCyt+, urine cytology and both tests combined had an overall sensitivity of 86%, 47% and 90%, respectively. Specificity of ImmunoCyt/uCyt+ alone and combined with cytology amounted to 79%. Cytology alone was 98% specific. In the series of 121 patients, including 11 pTaG1–2, eight pT1G2–3 and seven pT2G2–3 carcinoma, 39% sensitivity for ImmunoCyt/uCyt+ and 35% for cytology was found. The combined sensitivity was 54%. Specificity of ImmunoCyt/uCyt+ and cytology was 84% and 92%; respectively. The combination of both tests revealed 82% specificity.15 These studies have shown a higher sensitivity for ImmunoCyt/uCyt+ compared with urine cytology. ImmunoCyt/uCyt+ cannot replace cystoscopy, but it may prove useful as an adjunct to cytology in the management of bladder cancer.
BTA TRAK Assay and BTA Stat Test
BTA TRAK and BTA Stat tests (Bard Diagnostic Sciences Inc., Redmond, WA) are enzyme immunoassays intended for the measurement of human complement factor H related protein (hCFHrp) in urine using the two monoclonal antibodies X13.2 and X52.1.21,22 Bladder tumour cells shed hCFHrp into urine, presumably to protect themselves from being destroyed by the complement system.23 BTA TRAK is a quantitative assay, whereas BTA Stat is a quantitative test.
In various studies24–31 overall sensitivity of the BTA TRAK test was reported to be 64% (range 56% to 72%) and overall specificity to be 71% (51% to 95%) (see Table 2). The mean sensitivity for the BTA stat test (see Table 3) was 72% (range 57% to 100%) and the mean specificity was 74% (range 64% to 93%).32–41 The diagnostic PPVs and NPVs of the BTA assays (see Table 7) ranged from 35% to 68% and 70% to 95%, respectively.26,32,36,40 Sarosdy et al.41 evaluated the BTA stat test in the detection of recurrent bladder cancer and achieved 67% sensitivity (147/220). For those patients with previous cytologic results available, cytology had a sensitivity of 23% and the BTA stat test of 58% for detection of recurrent cancer (p<0.001). Ellis et al.31 found an overall sensitivity of 72% (151/216) with the BTA TRAK assay in patients with recurrent bladder cancer. In comparison with urine cytology BTA TRAK and BTA stat had higher sensitivities but lower specificities.35,37,39,41 For low-grade and low-stage tumours the sensitivity is comparable with published sensitivities of urine cytology.33 The specificity of the BTA tests was found to be lower in patients with another genitourinary cancer or benign genitourinary disease such as haematuria, urinary tract inflammation, or renal calculi than in healthy volunteers.36,37 Furthermore, intravesical bacillus Calmette-Guerin (BCG) treatment may result in up to 28% decreased specificity.39 The BTA tests are superior to voided urine cytology in diagnosis of bladder cancer and detection of recurrent bladder cancer. Due to low specificity, BTA should not be used without first ruling out benign or malignant genitourinary disease, other than bladder cancer.
NMP22 and NMP22 BladderChek Test
NMP22 and NMP22 BladderChek (Matritech Inc., Newton, MA, US) are tests intended for the measurement of nuclear matrix protein 22, which is highly released into patients’ urine by apoptotic tumour cells. NMP22 is a quantitative immunoassay, while NMP22 BladderChek is a quantitative point-of- care test that can be performed in the office before or at the time of cystoscopy visit. Several studies35,40–51 have shown an overall sensitivity and specificity of 66% (range 47% to 89%) and of 75% (range 60% to 84%), respectively, for the NMP22 assay (see Table 4). There was an increase in sensitivity with increase in tumour stage and tumour grade.43,49 Soloway et al.51 monitored disease status after endoscopic tumour resection and found 70% (23/33) of the recurrences. When urinary NMP22 and voided urine cytology were compared, NMP22 showed higher sensitivity in patients with urothelial cancer.43,47,50 NMP22 is superior to cytology for detection of low-grade tumours, but with a limited specificity. Awareness and exclusion of benign lesions can increase the specificity, as Ponsky et al.45 demonstrated. After exclusion of false-positive results in 608 patients, they found an overall sensitivity and specificity of 89% and 84%. NMP22 is approved by the FDA for screening for bladder cancer and it may be useful for diagnosing symptomatic patients or people with occupational exposure to known carcinogens like aromatic amines, polycyclic aromatic hydrocarbons, or chlorinated solvents. Only preliminary data on sensitivity and specificity (see Table 5) are available for NMP22 BladderChek.52–55 Tomera et al.55 identified 61% (11/18) transitional cell carcinoma including one ureteral carcinoma in high-risk patients. NMP22 BladderChek was more valuable than cytology with 18% sensitivity. Specificity of NMP22 BladderChek and cytology in patients determined not to have bladder cancer was 89% and 99%, respectively. Oehr53 excluded patients with urocystitis, stones, urinary tract infections (UTIs) and incorporated catheters and achieved a sensitivity and specificity of 82% and 98% in the haematuria group and of 61% and 98% in the follow-up group, respectively. Overall, for the NMP22 BladderChek test a lower rate of false-positive results was reported than for the NMP22 assay yielding higher PPVs and NPVs (see Table 7).40,42,44,45,47,48,51,53,54 The accuracy of NMP22 and NMP22 BladderChek, for the reliable diagnosis of patients at risk from bladder cancer has to be evaluated in a prospective multicentre study.
UroVysion Test
UroVysion (Abbott Laboratories Inc., Downers Grove, IL, US) is a multi-probe fluorescence in situ hybridisation (FISH) technique to detect aneuploidy for chromosomes 3, 7, 17 and loss (deletion) of the 9p21 locus via fluorescence in situ hybridisation (FISH) in exfoliated bladder tumour cells. Table 6 lists studies of the UroVysion test published by various groups.56–60 Overall, UroVysion improves the sensitivity rates reported for urine cytology in detection of all tumour stages and grades with a similar specificity. Grade 1 and 2 bladder cancer was detected in 36% to 83% and in 76% to 83%, respectively. Placer et al.57 reported a lower sensitivity for cytology with 64% overall, 25% for grade 1, 67% for grade 2 and 95% for grade 3 tumours compared with FISH – 80%, 53%, 83% and 100%. Skacel et al.56 tested urine samples from patients with suspicious, atypical and negative cytology compared with biopsy data. The sensitivity was 100%, 89% and 60%. Nine patients with atypical cytology had positive FISH in the setting of a negative concurrent bladder biopsy. All had biopsy proven carcinoma, no later than 15 months following the date when the sample tested by FISH was obtained. The results achieved with UroVysion emphasise an important role of this assay in the management of bladder cancer. UroVysion provides high sensitivity and specificity to detect transitional cell carcinoma in cytologically equivocal and negative urine samples. UroVysion appears to be a promising tumour marker for the early detection of recurrent bladder cancer and may be useful for screening persons at risk for bladder cancer.
Conclusions
Recent developments in the field of bladder tumour marker tests are either qualitative or quantitative measurements of urinary proteins or detection of antigens or chromosomal aberrations in urine cytology samples. These tumour marker tests demonstrated improved sensitivity for the diagnosis of urothelial cancer compared with urine cytology. Overall, the mean sensitivity and mean specificity was 64% to 80% and 71% to 95% and the mean PPVs and NPVs to detect malignancy were 49% to 84% and 79% to 95% (see Table 7). Sensitivity for Ta grade 1 bladder cancer was poor in tests detecting proteins released into urine by tumour cells. BTA TRAK, BTA stat, NMP22 and NMP22 BladderChek assays are limited by false-positive results in patients with benign urological disease such as haematuria, urocystitis, renal calculi, or UTIs, as well as in patients with incorporated catheters or intravesical manipulation in the last weeks. Due to low specificity BTA TRAK, BTA stat, NMP22 and NMP22 BladderChek should not be used without first ruling out benign or malignant genitourinary disease other than bladder cancer. Insufficient sensitivity along with limited specificity does not allow replacing cystoscopy in diagnosis of bladder cancer or treatment decisions based on a positive test result. With the exception of UroVysion, achieving 80% sensitivity and 94% specificity, none of these non-invasive tests revealed a high sensitivity and specificity at the same time, which would be a main criterion of an ideal tumour marker. Furthermore, UroVysion is not limited by exclusion criteria. ■