Malignant melanoma is an aggressive form of skin cancer and has demonstrated an increasing mortality among men in the last quarter century.1 The 5-year survival rate is approximately 15–20 % for stage IV melanoma.2 Surgical management of primary melanoma remains wide excision with or without the addition of sentinel lymph node biopsy. While 5-year survival for stage I and II melanomas is good, outcome for stage IV melanoma remains bleak. Recently, a number of directed therapies have been developed for treatment of metastatic malignant melanoma. Many of these are predicated on the presence of specific mutations sensitizing the malignant cells to specific chemotherapeutic agents. Molecular techniques are required to document the specific mutations, thus tissue from metastatic sites is needed to guide selection of specific therapies. Given that specific therapies with efficacy against metastatic disease now exist, the early recognition of distant metastases by imaging modalities and their biopsy have become important in the management of stage III and IV melanoma patients. Herein, we review blood marker testing, imaging methods and indications, biopsy techniques, and ancillary testing for directed therapies in patients with metastatic malignant melanoma. The current review is limited to cutaneous melanoma and its metastases.
Clinical History and Initial Physical Examination
Following the identification of a clinically suspicious pigmented lesion, the patient should have a focused medical history taken documenting the presence of any family history of melanoma or other skin cancer as well as whether or not there is a family history of multiple, irregular, or prominent moles. The history should also include documentation of the presence or absence of pancreatic ductal carcinoma or astrocytoma within the family. The patient should be specifically questioned about a history of prior personal melanomas. A history of significant prior sun exposure should be documented. The patient should be asked about changes they have noted in other moles specifically regarding alterations in size, color, shape, or the presence of bleeding or ulceration. A personal history or family history of multiple nevus syndrome should be queried.
Physical examination should include a total body skin examination with photography of nevi and other suspicious cutaneous lesions. This total body skin examination is performed to assess the number of nevi present and to distinguish between typical and atypical lesions.
Biopsy of Primary Lesion and Histologic Examination
The index atypical pigmented lesion should be excised in total if possible. Shave biopsies are suboptimal specimens as they may preclude accurate evaluation of depth of invasion and assessment of architectural features that are important for diagnosis. Excisional biopsies are recommended because they allow the evaluation of junctional activity at the edges of the lesion and the deep margin. Such assessment also aids in the diagnosis of melanoma because it allows evaluation of lesional symmetry.
Histopathologic evaluation is performed and expert consultation is desirable for difficult lesions. The College of American Pathologists synoptic report should be addended to the diagnostic report. This synoptic checklist should include a statement as to the type of melanoma (superficial spreading, lentigo maligna melanoma, acral lentiginous, nodular, or other types) present. Clark’s level of invasion and Breslow thickness should be given. The thickness should be measured with the aid of a micrometer. The checklist should also include a statement on the lymphoid host response at the base of the lesion being designated as none/minimal, mild (nonbrisk), marked (brisk), or other. Associated lesions should be documented. The presence or absence of ulceration should be documented as well as the mitotic index (rate). Angiolymphatic invasion should be documented as present or absent. The presence of regression should be described as well as satellitosis, if present. Operative margins need to be evaluated. The presence or absence of involvement of peripheral margins should be documented and the distance between the melanoma and margin stated for uninvolved peripheral margins. Similarly, the status of the deep margin should be documented and when negative, the distance between the melanoma and the deep margin stated.
Both Clark’s level and Breslow thickness have prognostic value.3–5 Many experts in dermatopathology believe that both should be reported. Determination of Breslow thickness requires a micrometer while Clark’s level does not and may be the easier measurement to determine. Tables 1 and 2 describe Clark’s level and Breslow thickness cutpoints.
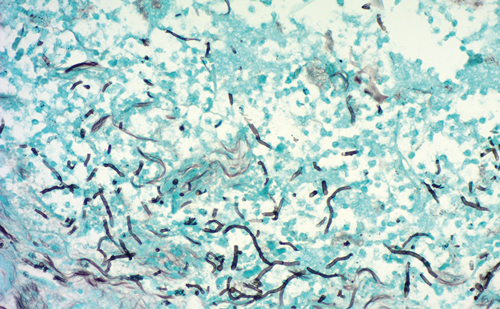
Following a histopathologic diagnosis of melanoma, re-excision should generally be performed. Elective lymph node dissection for patients with clinically enlarged lymph nodes should be undertaken. When lymph nodes are clinically within normal limits, sentinel lymph node biopsy is often performed for staging purposes.6–8 Dynamic lymphoscintigraphy is used for localization of sentinel lymph nodes.9,10 Sentinel lymph nodes histopathologic examination may include either microscopic examination of multiple hematoxylin and eosin stain (H&E) stained levels or the use of immunohistochemistry for s100 protein, melanin-A, and, perhaps, HMB- 45.11,12 Subsequent therapy is based upon status of the sentinel lymph nodes and the thickness of the primary melanoma.
Histopathologic Staging
Histopathologic staging involves assessment of Clark’s level and Breslow thickness as defined in Tables 1 and 2. The American Joint Committee on Cancer (AJCC) has proposed a TNM system for staging melanoma.13 T classification is based on thickness and the presence of ulceration as shown in Table 3.
Imaging Techniques and Indications
Traditionally, imaging studies are performed in patients with recently diagnosed melanoma. While low-cost studies such as chest radiographs are useful in establishing a baseline, more-expensive imaging techniques may not be cost-effective.14 Few guidelines exist that define appropriate testing protocols for initial evaluation and follow-up of patients with melanoma.15 Malignant melanoma has a propensity to metastasize widely with common sites for deposits of melanoma being skin, lymph nodes, liver, bone, lung, gastrointestinal tract, and brain. Multi-institutional studies have shown that ultrasound (US) is the superior technique for documentation of metastases to sentinel lymph nodes while positron emission tomography (PET) and computed tomography (CT) appear to be the best methods for identifying metastases at other sites.16 Current American Academy of Dermatology guidelines do not recommend baseline testing in asymptomatic patients with stage 1a–2c cutaneous melanoma.17 Similarly, guidelines proposed by the National Comprehensive Cancer Network (NCCN) indicate that no laboratory testing or baseline imaging studies should be obtained in asymptomatic patients with stage IA, IB, or IIA melanomas. Chest radiographs are optional for stage IIB and IIC patients.18 The NCCN guidelines support the concept that most melanoma recurrences are initially recognized clinically. Imaging studies are indicated for confirmation of clinically suspected metastatic disease and potentially in patients with stage IIB to IV disease.18 Scheduling of followup imaging studies for patients with thick melanomas or after treatment for metastatic disease is controversial and definitive guidelines do not exist. Patients with positive sentinel lymph nodes often undergo extensive imaging studies either before or after completion lymphadenectomy or when being considered for further therapy.15 Despite the widespread use of such testing in patients with only a positive sentinel lymph node, the yield of such studies is small bringing into question their utility.19–21 Patients with stage III disease with locoregional melanoma should have further imaging studies including CT, magnetic resonance imaging (MRI), or PET due to their relatively high (50 %) risk for systemic disease. CT examination should include the chest and abdomen/pelvis.22–24 PET-CT is the dominate imaging technique for evaluation of patients with highstage disease.25 PET-CT has considerable advantages including: 1) higher sensitivity in comparison to CT and 2) gives whole-body coverage in one examination possibly eliminating the need for other tests. Patients with known stage IV disease should undergo comprehensive imaging evaluation to detect additional sites of involvement.15
Laboratory Studies
Surveillance laboratory studies appear unnecessary for low-stage disease (stages IA, IB, and IIA). Serum lactate dehydrogenase (LDH) levels have been recommended as part of follow-up for patients with distant metastatic disease. Elevated LDH levels may indicate a worse prognosis.18
Biopsy of Suspected Metastatic Disease
Biopsy of suspected metastatic disease is performed for two reasons. First, biopsy may be obtained to confirm the clinical and/or imaging impression of metastatic disease. Second, when targeted therapies are being considered, mutational analysis for the presence of BRAF and CKIT mutations is often performed and requires lesional tissue. Biopsy specimens suitable for mutational analysis include core needle biopsies, fine needle aspirates (cell block preparations), and material from incisional and excisional biopsies. Formalin-fixed paraffin embedded tissue is currently the most widely used specimen type.
Diagnostic biopsies may be performed for evaluation of regional lymphadenopathy or for the confirmation of the presence of distant metastatic disease. Currently, evaluation of sentinel lymph nodes is considered standard of care. Traditionally, this evaluation has been performed by excisional biopsy but some investigators have evaluated the use of fine needle aspiration (FNA) in this setting. The low-cost, rapid turnaround time and very low morbidity of FNA in comparison to excisional biopsy makes FNA a desirable alternative for the evaluation of sentinel lymph nodes. Several investigators have studied the utility of FNA for the evaluation of sentinel lymph nodes.26–30 Detection rates for melanoma in sentinel lymph nodes by FNA have been reported to be 24.3 %,28 33.8 %,30 and 65 %.29 Thus, FNA is not reliable. Current data indicate that FNA is not a replacement for excisional biopsy in the evaluation of sentinel lymph nodes.28–30 FNA has been used successfully for the evaluation of clinically suspicious regional lymphadenopathy.31
Biopsy of newly discovered lymphadenopathy or a mass lesion in a patient without a known primary or in a patient with multiple primaries requires histologic and often immunohistochemical evaluation to determine the primary site for the metastatic lesion. Malignant melanoma is known to display many morphologic appearances and simple H&E morphologic evaluation may be insufficient. A number of antibodies exist that are useful in the differential diagnosis. Site of the deposit under investigation aids in selection of the antibody panel utilized. Antibody panels directed against all members of the differential diagnosis are most helpful and should include both antigens expected to be present as well as absent in the important members of the differential diagnosis. When melanoma is suspected, the most useful markers for the establishment of a diagnosis of malignant melanoma are s-100 protein, HMB-45, tyrosinase (MAT-1), and MART-1 (melan-A). These markers when used in combination with markers for other epitheloid (AE1,3, epithelial membrane antigen, CEA, and CAM 5.2) or spindle cell (desmin, actin, and caldesmon) lesions are extremely helpful in establishing a diagnosis of melanoma. The combined use of immunohistochemistry for HMB-45, S-100 protein, and MART-1 has a sensitivity of over 95 %.32–33 MART-1 staining has a better sensitivity than HMB-45 and superior specificity than S-100 protein staining.34 Since less than 3 % of melanomas stain for keratin, immunohistochemical staining for keratins (AE1,3 and CAM5.2) is of limited diagnostic value.
At the present time, molecular diagnostic techniques are helpful as predictive markers for targeted therapy, but do not play a significant role in the diagnosis of primary or metastatic cutaneous malignant melanoma. As a final point, both primary and metastatic malignant melanoma may show mutational and immunohistochemical heterogenity.35 BRAF mutations have been shown to demonstrate heterogeneity between metastases with therapeutic implications.36 Immunohistochemical heterogeneity has been shown to exist for BRAF (V600E) in primary and metastatic melanoma.37 Similar heterogeneity is seen for promoter hypermethylation.38
The selection of a biopsy technique for a clinically or imaging suspicious lesion is not a trivial decision. Selection of the optimal technique should consider lesion location, size of lesion, proximity to vital structures, health of the patient, cost, and diagnostic accuracy of the biopsy method. FNA can sample lesions at a wide variety of body sites and is minimally invasive and unlikely to contaminate the tumor bed or needle track. While a few needle track implantations have been documented, most have occurred after biopsy with larger gauge needles.39–43 Complications associated with FNA are few and mostly related to local hemorrhage or pneumorthorax (lung metastases). The major questions regarding sampling by FNA involve diagnostic accuracy and whether or not sufficient tissue can be obtained for ancillary studies.
Diagnostic accuracy of FNA for melanoma has been well studied.31 Over 970 studies have investigated the diagnostic accuracy of FNA for the diagnosis of metastatic melanoma.31 In pooled data, the sensitivity is 0.97 and the specificity is 0.99. These results compare favorably with those obtained by core biopsy and are not significantly inferior to those achievable by open biopsy. From these data it appears that FNA should be the first-line option in a patient clinically suspected of having metastatic melanoma.31
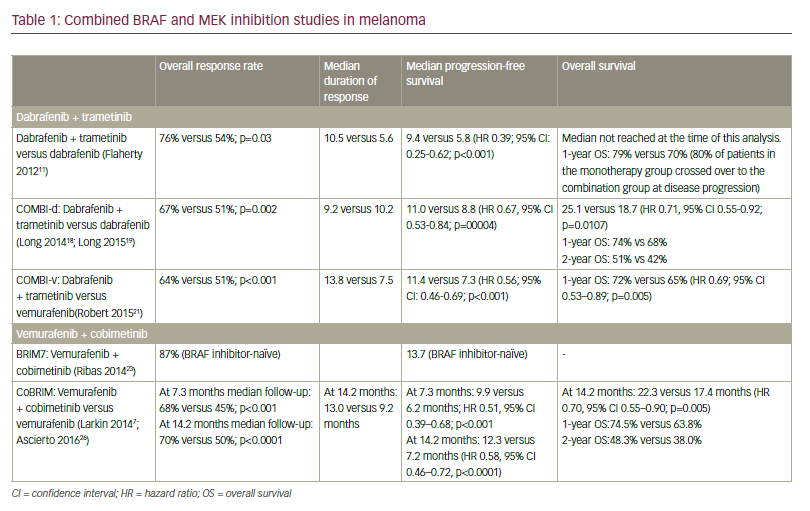
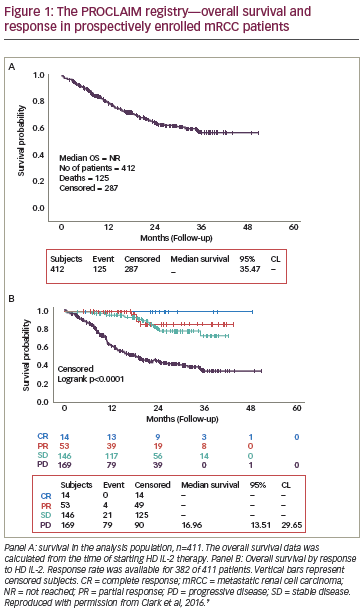
Treatment options for stage IV melanoma are limited. Recently, targeted therapies have been developed that appear to improve prognosis for patients with high-stage melanoma. Specific therapeutic agents have been developed for treatment of melanomas harboring BRAF or KIT mutations.44–48 The efficacy of these targeted therapies appears to be determined by the presence of specific gene mutations. Most treatment protocols utilizing these agents require tissue confirmation of the presence of the sensitizing mutation. Few studies have been performed documenting the effectiveness of FNA for obtaining sufficient tissue, but in the author’s experience FNA has been a successful technique in obtaining sufficient tissue for those ancillary molecular tests. Techniques obtaining larger specimens are also highly successful in procuring adequate tissue.