Metastatic cancer is the most common malignant disease of the bone.1 Breast and lung carcinomas account for more than 80% of metastatic bone disease.2 Metastasis to the bone causes significant pain and morbidity to the patient early in the course of the disease.3 It can lead to fractures and reduced mobility, thus reducing performance status and causing depression and anxiety.4–6 Palliative treatment is the mainstay of treatment in these groups of patients. It includes radiotherapy, chemotherapy, analgesics and palliative surgery.7 However, there have been significant advances in the management of patients with bone metastasis. The introduction of minimally invasive techniques and the concept of filling metastatic lesions with acrylic bone cement via minimal access have revolutionised the management of patients. Such techniques are usually performed under conscious sedation, thus reducing the risks of general anaesthesia in this group of patients who are often unfit for major surgery. In this article we present a review of some of the interventional techniques performed by the radiologist.
Percutaneous Vertebroplasty
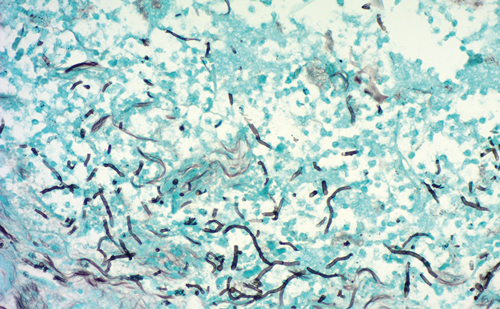
Of the secondary skeletal metastases, the spine is the most frequentsite, accounting for up to 40%, with the breast, prostate and lungs being the most common primaries.8,9 The thoracic spine is the most common site, followed by the lumbar and cervical regions.9,10 Percutaneous vertebroplasty was first described by Galibert et al.11 in 1987. The procedure essentially consists of an injection of lowviscosity bone cement (surgical methyl methacrylate polymer [PMMA]) via a large-bore needle into a vertebral body under image guidance.12 Over the past decade, percutaneous vertebroplasty has been used extensively for pain relief and bone strengthening of weakened vertebral bodies due to disease process.11,13,14 The main aim of vertebroplasty is to provide pain relief by strengthening and stabilising painful vertebral body compression fractures.12 There is no clear consensus on the mechanism of pain relief, but it is thought to be due to immobilisation of the fracture site and support of the innervated cortex. It has also been hypothesised that the heat produced when the PMMA solidifies deadens the sensory nerve fibres. Percutaneous vertebroplasty is commonly performed in the thoracic and lumbar vertebrae, and, rarely, in the cervical vertebrae.
Indications
The main indications for percutaneous vertebroplasty are vertebral body compression fractures due to osteoporosis/osteopenia, myeloma, osteolytic metastasis, Kummell’s disease and aggressive vertebral haemangiomas.12,15 All of these disease processes result in painful vertebral-body collapse, leading to significant morbidity and deterioration of quality of life, mental health and survival.16 Pain associated with vertebral compression fractures often becomes chronic with incomplete healing, ultimately resulting in spinal deformity and kyphosis.16 This shifts the centre of gravity anteriorly, resulting in more pronounced flexion and further deformity and vertebral fractures.16 Vertebroplasty aims to reduce pain and strengthen the vertebral body, thus preventing further deformity.16 Radiotherapy is indicated in the spine when the cause is due to tumour and metastasis, but the effect is often delayed, during which time there is significant risk of instability of the vertebral column and neural compression – hence the role of vertebroplasty in metastatic disease in particular.15
To read full article please click here