Radiotherapy, however, has many advantages in this setting, including the preservation of anatomy and avoidance of surgery, which is particularly useful in elderly patients who may be unsuitable for general anaesthetic or those on anticoagulants. The spectrum of cancers treated by radiotherapy is wide and includes lentigo maligna, lentigo maligna melanomas, Kaposi’s sarcoma, cutaneous T-cell lymphomas and Merkel cell tumours, and sweat gland tumours, in addition to basal cell and squamous cell carcinomas. Most patients are never given the chance of having radiotherapy; they are seen by either a dermatologist or a surgeon, and treated accordingly. At the authors’ institution, there is a joint skin clinic, with plastic surgeons, dermatologists and clinical oncologists.
Features of Kilovoltage X-rays
Kilovoltage X-ray equipment has been used therapeutically for the treatment of skin cancers for more than 100 years. More recently, in some centres, its use has diminished as megavoltage (the use of high energy X-rays delivered using linear accelerators) and electrons (often preferred because their depth of penetration can be accurately prescribed according to the energy used) have replaced it for many clinical applications. Kilovoltage X-rays units have the advantage of being low in cost compared with megavoltage units because of the relative simplicity of design and operation, and the use of simple collimation and beam shaping. The housing of such equipment requires less in the way of radiation protection compared to linear accelerators. (Linear accelerators are often housed in the basements, whereas superficial machines can be placed on the ground floor.) The use of a kilovoltage machine means that departments can optimise the use of their megavoltage machines for treating other non-cutaneous malignancies. X-ray therapy in the kilovoltage range is conventionally divided into four areas:
- Grenz rays of 10–20kv (kilovolts). These are still used in some centres, particularly in Germany.
- Contact therapy using 40–50kv and short sourcesurface distance (SSD). These are used for treatment depths of 1–2mm as they provide very rapid falling depth-doses.
- Superficial therapy using 50–150kv. With typical filtration, beams with half-value layers (HVLs) in the range of 1–8mm Al. The SSD is normally 10–30cm. Beam characteristics are suitable for treatment of lesions up to 5mm deep, delivering 90% of the dose to the surface.
- Orthovoltage therapy (‘deep therapy’) with 150–300kv. Most clinical units operate at 200–300kv. The treatment distance is about 50cm SSD. Ninety per cent of the dose delivered within approximately 2cm of the surface.
Planning Technique
Confirmation of the diagnosis histologically or cytologically is usually recommended so that a rational treatment approach can be made, but sometimes a clinical diagnosis alone is sufficient. An assessment of the depth of the tumour is made. There can be deep penetration of the tumour at sites of embryonic fusion planes such as the nasolabial fold, ala nasi, tragus and post-auricular area, and care should be taken to ensure adequate margins at depth at these sites (see Figure 1).
The gross tumour volume (GTV) is drawn. This is the extent of macroscopic disease visible. The definition of tumour margin is best done with a magnifying glass in a well-illuminated room. A margin around the GTV is then drawn to encompass subclinical extension of disease and to take account of any potential change in position of the patient during fractionated radiotherapy, and also to ensure that the prescribed dose is delivered to the volume. This additional margin is known as the planning target volume (PTV). The size of this is dependent on the tumour size, histology, aggressiveness and evidence of perineural invasion. Small lesions (less than 0.5mm) with welldefined margins require between 5mm and 8mm, whereas larger lesions – particularly squamous cell carcinomas – require 1cm margins. The appropriate beam energy can then be chosen depending on the clinical assessment of depth of the lesion.
Most departments have standard lead ‘cut-outs’ for regular-shaped treatment volumes. Alternatively, in preparation for treatment, patients may attend the ‘mould room’ for a customised lead cut-out to be fashioned to fit the treatment volume of their tumour. The thickness of lead is dependent on the energy of the beam used. For 90–150kv, 1.5mm is sufficient (see Figure 2).
When treating tumours of the eyelid near the inner or outer canthus, an internal lead eye shield is used to protect the conjunctiva, cornea and lens. These are either internal eye shields or spade-shaped.
The patient is positioned appropriately on the treatment couch, with the lead cut-out in place over the lesion. The machine applicator of suitable diameter is then gently positioned over the area to be treated.
The daily dose and fractionation of radiotherapy is largely dependent on the site, size and histology of the lesion, in addition to the age of the patient and their ability to attend for treatment. Many different regimes (the number of daily radiotherapy fractions prescribed) have been shown to be effective, and the chosen regime should have optimum cure rate with least normal tissue damage. The authors’ institution uses most commonly 40.5Gy in nine fractions daily for basal cell carcinomas and 45Gy in 10 fractions daily for squamous cell carcinomas over two weeks. Other fractionation regimes used include 32.5Gy in five daily fractions and occasionally single 18Gy fractions for small basal cell carcinomas where cosmesis is relatively unimportant. The ‘Sambrook Split’ Technique is used for elderly patients. This requires two visits, five weeks apart, giving 12Gy at each visit.
Radiotherapy Reactions and Late Effects
During a course of radiotherapy, patients can expect to see erythema of the skin, as part of an acute radiotherapy reaction characterised by desquamation, oozing, crusting of the lesion and increased skin pigmentation. This is usually at its peak by about four to six weeks after radiotherapy and patients should be consented for this and reassured that this is temporary and reversible. After this time, the appearances improve, leaving healed skin below. Commonly observed late adverse side effects – seen over subsequent months or years – may include skin depigmentation, skin atrophy, telangiectasia and epilation. These effects are variable and acceptable to most patients if consented appropriately.
Lentigo Maligna
This is the in situ phase of lentigo maligna melanoma (LMM). Typically located on the face in older Caucasian women, they are often present for five to 15 years. They are generally large, flat lesions that may be tan or brown coloured. If left untreated, 30–40% of cases may progress to LMM, which is thought to behave as aggressively as any other melanoma. Lentigo maligna itself has low metastatic potential. Conventional surgery, cryosurgery and radiotherapy all have recurrence rates of between 5% and 10% and can be offered to patients. Radiotherapy has the advantage of preserving normal anatomy and function, and provides good cosmesis for lesions on the face. The dose used is 45Gy in 10 fractions over two weeks (see Figures 5 and 6).
Merkel Cell Tumours
These are rare neuroendocrine tumours arising from the mechanoreceptors of the basal epidermis. They are particularly aggressive and have a propensity for head and neck and extremity sites. The tumour has many similarities to small cell carcinoma of the lung, both histologically, with its intrinsic sensitivity to chemo-radiation and metastatic potential. Surgery is the treatment of choice. Post-operative radiotherapy is advocated to reduce local recurrence rates. Generous planning margins are included of between 3cm and 5cm around the scar.
Cutaneous T-cell Lymphoma
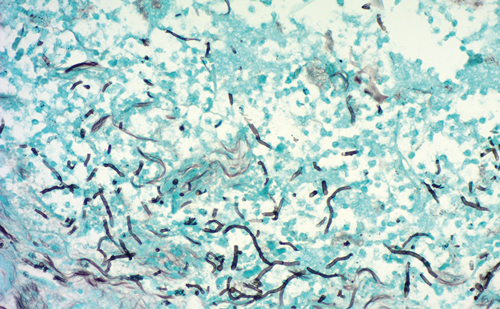
Also known as mycosis fungoides, this rare condition is a malignancy of T-helper cells. The skin lesions are very radiosensitive and superficial radiotherapy can be used for the localised plaque stage or small tumour stage with complete response rates quoted between 60% and 90%. More diffuse plaque disease is an indication for total skin electron beam therapy. Margins of 0.5–1cm are used and lesions treated to a dose of 8Gy in two fractions or 12Gy in three fractions treating daily.
Spectrum of Treatable Disease
The treatment of basal cell carcinoma and squamous cell carcinoma using radiotherapy is well documented and provides excellent local control and cure, equivalent to that of surgery. Superficial radiotherapy also plays an important role in the treatment of other skin tumours, for example lentigo maligna, Merkel cell carcinoma, cutaneous T-cell lymphoma and Kaposi’s sarcoma (see Figures 3 and 4).
Kaposi’s Sarcoma
Classical Kaposi’s Sarcoma (KS) is an unusual vascular sarcoma occurring in the skin of the lower extremities of elderly men of Jewish or Mediterranean descent. It usually follows an indolent course, but can metastasise to the lungs or gastrointestinal tract. Other types of KS exist: African, AIDS-related and in association with immunosuppressant therapy. For localised lesions, superficial radiotherapy is usually the preferred treatment option. Excision, cryotherapy and intralesional chemotherapy have also been described.
Conclusion
Kilovoltage machines have a very important role to play in the delivery of superficial radiation for the treatment of skin tumours. Most skin tumours can be treated with curative intent in those patients where surgery or other treatment modalities may be inappropriate.
Kilovoltage machines have become less popular for this role in certain centres where they have been superceded by electron therapy. It is important that not only this modality is considered for the management of skin tumours, but also that clinical oncology trainees continue to learn the necessary skills required to do so. Managing skin tumours in this way requires a sound, fundamental knowledge of physics, collaboration with radiographers and mould room technicians, and provides excellent opportunities to examine the effects of radiation on normal tissue and most importantly, effect cure in many skin cancers.