Even with the many recent advances in cytoreductive surgery and combination chemotherapy, ovarian cancer is still associated with poor survival prognosis and remains a significant threat to women all over the world. Ovarian cancer is the fourth most common cancer of the female reproductive system and represents the highest mortality of all malignancies of the female reproductive system, with 204,000 new cases of ovarian cancer and 125,000 related deaths worldwide each year.1
Even with the many recent advances in cytoreductive surgery and combination chemotherapy, ovarian cancer is still associated with poor survival prognosis and remains a significant threat to women all over the world. Ovarian cancer is the fourth most common cancer of the female reproductive system and represents the highest mortality of all malignancies of the female reproductive system, with 204,000 new cases of ovarian cancer and 125,000 related deaths worldwide each year.1
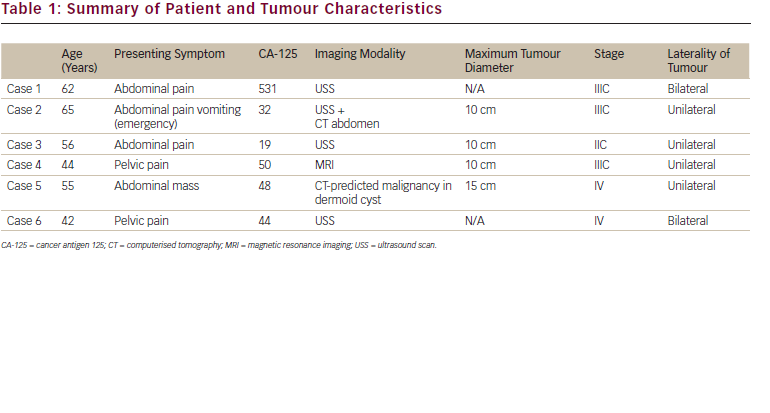
Ovarian cancer typically presents vague and non-specific symptoms such as abdominal pain or bloating, urinary symptoms or gastrointestinal symptoms similar to those of irritable bowel syndrome.2 Approximately 75% of women are diagnosed when the cancer has already progressed to advanced stages, spreading beyond the pelvis (International Federation of Gynecology and Obstetrics [FIGO] stages III and IV). By stage III, the outlook is already bleak, with an estimated five-year survival rate of 15–35%. Disease progression to stage IV reduces this expectancy to a grim 5–15%. The main problems with diagnosing the cancer are the lack of early symptoms and the limitations of screening tests. To address this problem, there are ongoing efforts to establish a working strategy for ovarian cancer screening for early detection of the disease.
The exact cause of ovarian cancer remains unknown, although the risk of developing the disease appears to be influenced by many factors, including age, body mass, family history of breast and ovarian cancer and genetic predispositions to other cancers. The risk of ovarian cancer has been shown to be reduced through pregnancy,3,4 with each birth reducing the risk by about 12%.5 The oral contraceptive pill has shown convincing evidence as well,6 with an estimated risk reduction of 7% for each year of use.7 Tubal ligations have also been associated with reduced risk of ovarian cancer.8
Treatment
Radical cytoreductive surgery and combination chemotherapy with platinum-based compounds and paclitaxel are now recognised as the international standard of care in the first-line setting. Cytoreductive surgery aims to remove as much of the tumour as possible (tumour debulking).9 It has also been suggested that median survival can be increased by 5.5% for each 10% increase in maximal cytoreduction.10
Although initial response rates to cytoreductive surgery and combination chemotherapy are high, the majority of patients will subsequently relapse within three years of diagnosis, and continued disease progression will ultimately lead to death within five years.11 The value of therapy is often determined using a six-month threshold: if relapse occurs beyond six months, treatment is continued. However, early relapses occurring within six months of initiating therapy are usually unresponsive to re-introduction of platinum-based compounds. Of special interest for clinical researchers is how to optimise the therapeutic index of cancer agents for patients with recurrent ovarian cancer.
Topotecan, a topoisomerase-I inhibitor, has been extensively studied in both platinum-resistant and -sensitive relapsed ovarian cancer. Topotecan is one of the most active agents in recurrent ovarian cancer and is a standard therapy for platinum-resistant ovarian cancer patients in many western countries. Topotecan and paclitaxel have been shown to have similar activity in terms of response rates, progression-free survival (PFS) and overall survival (OS), with a demonstrated lack of cross-resistance.12 However, the severe haematological toxicities associated with topotecan occur at a significantly increased incidence compared with paclitaxel.13 Conventionally, topotecan is administered following a five-day schedule over a 21-day cycle, but this has been associated with increased bone marrow toxicity, limiting the practicality of using the drug in older patients with low performance status.
In a North-Eastern German Society of Gynaecological Oncology (NOGGO) phase III study, women with recurrent ovarian cancer after primary surgery and platinum therapy were randomised to receive topotecan 1.25mg/m2/d (TM), topotecan 1.0mg/m2/d plus oral etoposide 50mg/d (TE) on days six to 12 or topotecan 0.5mg/m2/d plus gemcitabine (TG) 800mg/m2/d1 and 600mg/m2/d8 every three weeks.14 Between September 1999 and November 2004, 3,036 courses were administered to 505 patients (mean age 60.4 [SD 11.3] years), 208 of whom had a treatment-free interval (TFI) <12 months. Median OS after TM, TE and TG was 17.8, 17.8 and 15.3 months, respectively. Setting TM as the reference, hazard ratios (HRs) for OS with TE and TG were 1.13 (95% confidence interval [CI] 0.87–1.47) and 1.07 (95% CI 0.80–1.43), respectively (p=0.590). HRs for PFS with TE and TG versus TM were calculated at 0.84 (95% CI 0.66–1.07) each. This large randomised controlled trial does not provide evidence that combined treatment performs generally better than topotecan monotherapy in recurrent ovarian cancer. Accordingly, topotecan monotherapy remains the standard regimen. Because the main toxicity of topotecan is haematological, researchers have investigated the possibility of using this agent in weekly regimens instead to reduce the frequency of exposure.
Weekly Dosing Schedules
Topotecan given in a weekly schedule is effective in various solid tumours, including cervical, lung and ovarian cancer. Studies have shown that this weekly dosage is better tolerated than the conventional five-day regimen.15–18 Similar conclusions were drawn in two retrospective analyses of patients treated with weekly topotecan: comparisons against previously published data for the five-day regimen showed that the weekly administration was just as effective, but had the advantage of presenting with considerably less haematological toxicity.19,20 The fact that topotecan is an S-phase-specific agent supports the idea that repeated exposure and dosing can lead to a greater reduction of tumour cells, and suggests that the drug may have schedule-dependent efficacy.
Furthermore, it is known that levels of the targeted topoisomerase-I decrease with prolonged drug exposure, but return to baseline levels in seven days.21 A weekly regimen might therefore be able to target cells when they are most vulnerable to topotecan. Until recently, there had been no randomised trials that directly compared the weekly topotecan regimen with the five-day therapy. A previous attempt to perform such a comparison in platinum-sensitive patients by the American Gynecologic Oncology Group (GOG) for platinum failed due to slow recruitment, and was prematurely terminated.
The North-Eastern German Society of Gynaecological Oncology – TOWER Study
The ‘Topotecan weekly versus routine five-day schedule in patients with platinum-resistant ovarian cancer’ (TOWER) study is a randomised, openlabel, two-stage phase II investigation conducted by NOGGO. Preliminary results from a planned interim analysis were recently presented at the 2007 American Society of Clinical Oncology (ASCO) Annual Meeting.22
Patients and Methods
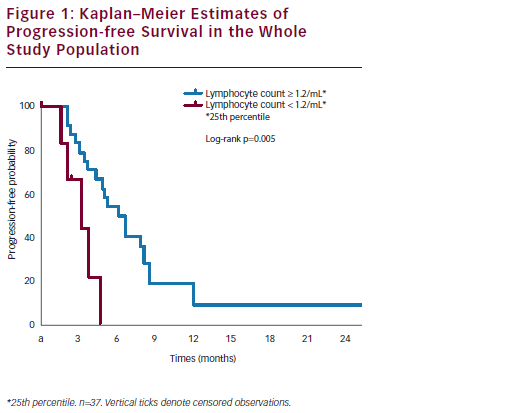
Patients with ovarian and fallopian tube cancers or primary peritoneal carcinoma having failed prior initial therapy with platinum/paclitaxel combination chemotherapy or with response duration less than six months were eligible for the study. Measurable or assessable disease (GCIG-CA-125 response criteria) was required. Patients were randomised to receive topotecan either weekly (d1,8,15/q28d, 4mg/m2) or under the five-day regimen (d1–5/q21d, 1.25mg/m2). The primary end-point was designated as the overall response rate (complete and partial response), with secondary objectives of PFS, OS and quality of life.
Results
In the interim analysis, the median age of the patients was 61 years (range 36–82 years). Patient characteristics – including disease stage, histology, grade and age – were well-balanced. Toxicity analysis was performed following 230 cycles of chemotherapy, and 28 and 21 patients in the weekly and conventional arms, respectively, were evaluated for response. Overall response was not statistically different (HR 0.30%, 95% CI 0.06–1.40, Fisher’s exact test p=0.122). There were also no significant differences between the groups in terms of the risk of early termination of treatment due to tumour progression (HR 1.39, 95% CI 0.75–2.56) or haematological (HR 0.2, 95% CI 0.01–3.97) or nonhaematological toxicities (HR 1.96, 95% CI 0.18–20.83). Interestingly, patients in the five-day protocol were more likely to demand premature cessation of therapy than those in the weekly arm. At the time of writing, there are currently 183 of 194 patients enrolled in this trial.
Conclusion
The limitations in the armamentarium against ovarian cancer are obvious, as patients diagnosed with ovarian cancer have poor survival prognosis in spite of the many advances and developments in treatment. Until newer improved compounds are introduced, it is necessary to optimise the efficacy of the drugs that are currently available. Consistent with previously published studies, the preliminary results from the TOWER study show that the weekly dosage of topotecan is an active and well-tolerated regimen.
Furthermore, the interim analysis found no significant difference in efficacy between the two arms of the trial. Not only can this weekly regime of topotecan therefore reduce toxicity without compromising antitumour activity, but patients can also benefit from more convenient dosing and ameliorated quality of life. Because of the comparable efficacy and markedly reduced haematological toxicity, there is potential for weekly topotecan dosing to replace the five-day regimen as the standard schedule of administration, but further evaluations are still necessary. Following the presentation of the interim analysis, we have since entered the second stage of the TOWER study and expect the remaining patients to be enrolled by February 2008, with the final results of the study planned for 2009. ■