Neoadjuvant chemoradiation therapy has positively altered the natural history of several cancers, especially esophageal and rectal cancer, and many investigators are looking at neoadjuvant therapy in the treatment of pancreatic cancer. I hope to give a brief overview of where we stand in 2006 in terms of neoadjuvant chemoradiation therapy for pancreatic adenocarcinoma.
Chemoradiation therapy prior to pancreatic cancer surgery has a number of potential advantages over postoperative therapy. First, pancreatic cancer can be considered a systemic illness in most cases and neoadjuvant therapy provides systemic treatment within days of diagnosis. Second, patients undergo systemic therapy prior to the huge physiologic insult of a pancreatic resection. They are therefore more likely to complete their therapy and less likely to have complications or delays associated with being in the relatively debilitated postoperative state. Following pancreatic cancer surgery, 25% of patients adjuvant therapy is not received, delayed or truncated due to complications, morbidity or patient refusal.Third, patients whose disease progresses during neoadjuvant therapy selfselect for aggressive tumor biology, never come to surgery and avoid the morbidity of a pancreatic resection during their short time of survival. Fourth, the sterilization of the operative field by neoadjuvant therapy might decrease the risk of disseminating microscopic tumor during resection and also result in fewer positive margins. Fifth, radiation therapy generally is more effective in wellvascularized preoperative tissue compared to relatively hypoxic postoperative tissues. Sixth, bowel in the irradiated field is resected at the time of surgery, decreasing long-term effects of irradiated bowel.
A disadvantage is that these patients usually require greater pretreatment preparation than patients who are expeditiously explored. Prior to neoadjuvant therapy a tissue diagnosis (usually fine-needle aspiration (FNA) via endoscopic ultrasound) is needed and biliary obstruction must be controlled (usually via an endoscopic biliary stent).Many patients also undergo diagnostic laparoscopy to rule out occult metastatic disease. There is also the possibility of making the surgery more difficult because of an irradiated field, however there is evidence that neoadjuvant therapy may actually decrease pancreatic leak complications following surgery. The biggest potential concern is the possibility that a resectable patient may progress to an unresectable patient during the course of therapy, thus missing the window of opportunity for curative resection. In the end, the clinical relevance of these possible advantages and disadvantages can only be determined through wellcontrolled, randomized, prospective trials which determine overall morbidity and survival. Challenges to determining if neoadjuvant therapy is truly advantageous to patients include:
1. lack of agreement among oncologists as to the most appropriate neoadjuvant regimen, particularly given that current adjuvant therapies have modest response rates at best;
2. bias and fear among surgeons, patients and physicians that expeditious exploration and resection whenever possible is the only hope for cure; and
3. difficulty in accurately staging patients prior to therapy, particularly in determining involvement of the SMV/Portal Vein complex.
In evaluating neoadjuvant therapy trials, it is important to distinguish those reports in which locally unresectable cancers were treated, and after a clinical response (downstaging), patients were explored vs patients with radiographically resectable tumors who were treated with chemoradiation prior to planned surgery.
In evaluating neoadjuvant therapy trials, it is important to distinguish those reports in which locally unresectable cancers were treated, and after a clinical response (downstaging), patients were explored vs patients with radiographically resectable tumors who were treated with chemoradiation prior to planned surgery.
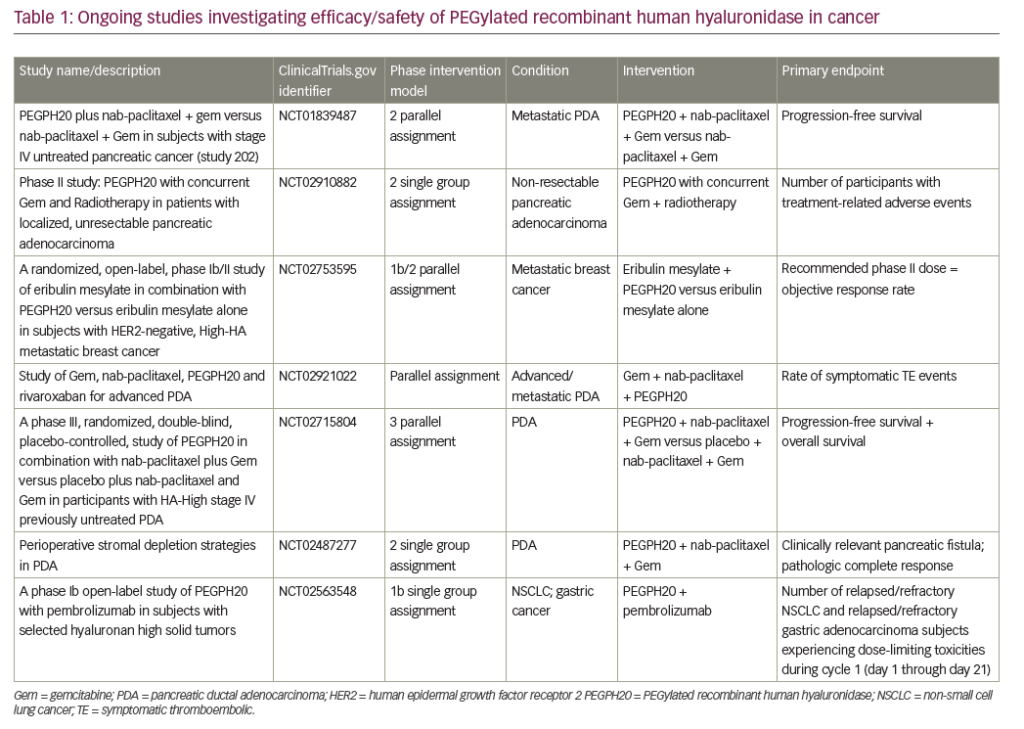
In terms of converting or downstaging locally unresectable tumors into resectable disease, there are many anecdotal reports and small series with a variety of agents. Based on a recent review of available literature, possibly 20% of locally unresectable patients may become resectable, and of these only about 50% will actually have negative margins (see Table 1). An interesting exception is the small series of Wanebo et al. in which nine of 11 patients underwent resection following a regimen of cisplatin, 5-FU and radiation. However, two-thirds of these patients required a major vascular resection and reconstruction (portal vein, superior mesenteric artery (SMA) or both) in order to obtain negative margins, and so these patients were technically not downstaged. Similarly, in a report by Fogelman et al. (Columbia) using a novel neoadjuvant strategy of gemcitabine, capecitabine, taxotere and radiation therapy, 12 of 17 (71%) patients underwent successful resection but 50% of those required vascular reconstruction. Until there is a breakthrough in adjuvant therapy, it is unlikely that more than a handful of patients will have successful downstaging of a locally aggressive cancer following neoadjuvant therapy.
*In some patients capecitabine (Xeloda) was substituted for 5-FU. #Cisplatin was eventually excluded secondary to toxicity. ^ “potentially resectable” ` “locally advanced”
The most important question to be answered is the role for neoadjuvant therapy in patients who appear to be radiographically resectable at the time of presentation.A summary of large series is provided in Table 2. (There are many smaller published series of neoadjuvant therapy for pancreatic cancer from North America and Europe, but I have chosen to focus on the largest of the available series.) Perhaps the earliest center to offer neoadjuvant chemoradiation therapy for localized (radiographically resectable) pancreatic cancer was the Fox Chase Cancer Center. Their 20-year experience demonstrates the safety and practicality of a neoadjuvant approach. Although median survival of those patients treated preoperatively was statistically no better than those patients who had postoperative therapy only, they note that as many as 86% of the neoadjuvant patients were considered “marginally resectable” (as opposed to clearly resectable) at the time of preoperative therapy whereas only 21% of patients without preoperative therapy were “marginally resectable”. This selection bias makes analysis very difficult and may obscure a small survival benefit in preoperatively treated patients.This observation is likely true for the ECOG study published in 1988.
The MD Anderson experience uses strict computed tomography (CT) resectability criteria for study inclusion, categorizing patients as “radiographically resectable” if the SMA and celiac axis are completely tumor free and the SMV/PV complex is patent). Encroachment on SMV/PV, however, was not an exclusion criterion and though their overall resection rate was up to 74% in the gemcitabine group, 43% of patients required vascular resection and reconstruction, suggesting they were actually “marginally resectable”. The Duke experience uses the same CT resectability criteria in categorizing patients as “potentially resectable” versus “locally advanced” and both groups were offered neoadjuvant therapy. As expected, resectability rate was much better in the potentially resectable group, but survival curves were the same through 24 months.
Conclusions that can be drawn from these series are that neoadjuvant therapy is safe. Patients who begin with radiologically resectable disease do better than patients who begin with locally advanced disease.There is a slight trend that gemcitabine may be more effective than 5-FU based therapy in terms of achieving a successful resection which is consistent with widespread belief that gemcitabine is advantageous over 5-FU in pancreatic cancer patients.