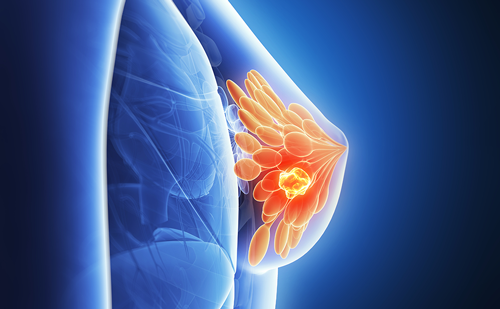
The type I family of tyrosine kinase receptors (TKRs) plays an important role in the pathogenesis of a subset of breast cancers.This family consists of four receptors known as the epidermal growth factor receptor (EGFR) and human EGFRs 2 (HER-2), 3, and 4.
Slamon et al.2 showed that HER-2 overexpression was associated with poor disease-free survival in women with node-positive breast cancer.The role of HER-2 as a predictive marker of response to hormone therapy and chemotherapy is controversial. However, HER-2 is considered one of the best therapeutic targets in patients with breast cancer. The HER-2 status of a tumor can be determined by using IHC or fluorescence in situ hybridization.
Trastuzumab (Herceptin®) is a monoclonal antibody directed against the HER-2 oncoprotein. Clinical trials have shown that trastuzumab is effective against metastatic breast cancer when administered as a single agent and that its efficacy is improved when combined with chemotherapy.3 In the pivotal clinical trials, patients were initially selected for therapy with trastuzumab if their tumors were found to be HER- 2-positive by using IHC. On a scale of 0–3, tumors were considered HER-2-positive if their HER-2 expression level was scored as 2 or 3 and HER-2- negative if their HER-2 expression level was scored as 0 or 1. Subsequent retrospective studies showed that such patients were more likely to benefit from receiving trastuzumab if their tumors expressed the HER-2 protein at high levels (IHC score, 3+) or have HER-2 gene amplification (fluorescence in situ hybridization positive).4 Based on the success of trastuzumab use, numerous molecules targeting the epidermal growth factor family of growth factor receptors and their ligands are in clinical development. These molecules include antibodies, small molecules, and vaccines.5 Other tumor markers that have been studied as potential prognostic and/or predictive markers include Targeting the Tumor—Translating Genetic and Molecular Profiling into Clinical Reality
Esteva.qxp 15/12/05 2:35 pm Page 76 the urokinase-type plasminogen activator and its inhibitors, molecules associated with angiogenesis (e.g. vascular endothelial growth factor (VEGF)), and markers of programmed cell death (also known as apoptosis). In addition to these tumor markers, hundreds of other molecules have been evaluated for their potential as prognostic factors.6 However, breast cancer is a complex heterogeneous disease, and evaluation of a handful of genes and/or proteins is likely to provide limited prognostic information.
High-throughput gene expression profiling with the use of microarray technology is a promising new technique that has been applied to classification of, prognosis for, and prediction of, response to treatment of breast cancers. Briefly, reference and tumor RNA are labeled by reverse transcription with different fluorescent dyes (green for the reference cells and red for the tumor cells) and hybridized to a complementary DNA (cDNA) microarray containing robotically printed cDNA clones. Slides containing labeled RNA are scanned with a confocal laser scanning microscope, and color images are generated for each hybridization with RNA from the tumor and reference cells. Genes upregulated in the tumor cells appear red, whereas downregulated genes appear green. Genes with a similar level of expression in the two samples appear yellow. Genes of interest are selected based on differences in the level of expression by tumor class (e.g. ER-positive and -negative tumors). Statistical analysis determines whether these differences in gene expression profile are greater than those expected by chance.
Using microarray technology with unsupervised hierarchical clustering analysis, Perou et al.7 classified invasive breast carcinoma into five subtypes based on their distinct gene expression profiles. This genomically based classification consisted of a luminal epithelial cell phenotype (subtypes A and B), a basal epithelial cell phenotype, an HER-2-positive pheno- type, and a group of cancers with a ‘normal-like’ gene profile. Patients with basal epithelial cell or HER-2- positive tumors had the worst survival rates, whereas those with luminal epithelial type tumors had a better prognosis.Although initially the luminal epithelial cell subtype correlated with ER positivity, ER levels were not uniform in tumors classified as luminal or basal epithelial cell tumors. Classification of tumors into specific molecular subtypes may improve diagnosis and risk assessment. Another potential application of molecular profiling is identification of the organ of origin in patients with poorly differentiated carcinomas of unknown primary.
van’t Veer et al.8 used expression microarrays and unsupervised hierarchical clustering analysis to identify a ‘poor prognosis signature’ that included 70 genes involved in regulation of the cell cycle, invasion, metastasis, and angiogenesis. They validated the 70- gene prognostic profile in 295 consecutive patients with primary breast cancer. Of these patients, 180 had a poor-prognosis signature, whereas 115 had a good- prognosis signature; the mean 10-year overall survival rate was 54.6% and 94.5%, respectively.At 10 years, the probability of remaining free of distant metastases was 50.6% in the group with a poor-prognosis signature and 85.2% in the group with a good-prognosis signature. In addition, the estimated hazards ratio for distant metastasis in the group with a poor-prognosis signature compared with that in the group with the good-prognosis signature was 5.1 (95% confidence interval (CI) 2.9–9.0; p<0.001). This ratio remained significant when the two groups of patients were analyzed according to lymph node (LN) status. This prognostic signature had strong independent value in multivariate analysis.
Molecular profiling with the use of microarrays is also under investigation as a tool to identify novel predictive markers of response to therapy. Identification of a group of genes that predict response to a given therapy generally requires supervised clustering analysis. Firstly, a group of genes is identified in patients with a known response to therapy (training set). Next, the molecular signature must be validated in an independent group of patients (validation set). Clinical trials designed to identify markers of response to pre-operative chemotherapy in patients with early-stage breast cancer with the use of microarray technology are on-going.
After giving their informed consent, patients undergo a core or fine-needle aspiration (FNA) biopsy for genomic analysis at the time of diagnosis. Patients then receive pre-operative chemotherapy, and the baseline gene profile is correlated with their pathologic response to the chemotherapy.10 Using this approach, identifying patients who are likely to have a response to specific types of chemotherapy (i.e. anthracyclines and taxanes), Targeting the Tumor—Translating Genetic and Molecular Profiling into Clinical Reality hormone therapy (i.e. anti-estrogens, aromatase inhibitors), or targeted biologic therapy (e.g. trastuzumab) may be feasible. Most genomic studies have used fresh frozen tissue specimens. On-going studies are evaluating the feasibility of transcriptional profiling with RNA extracted from formalin-fixed, paraffin-embedded tissue specimens.
Transcriptional profiling remains an investigational tool; further research is therefore needed before any profile can be used for clinical decision-making. One of the major limitations of transcriptional profiling is the lack of standardization and validation of gene sets across platforms. For example, when Sorlie et al.9 tested the prognostic impact of the 231 markers published by van’t Veer et al.,8 the positive predictive value (PPV) for disease-free survival was only 47%.This may have been due in part to the different patient cohorts and treatments.In fact,the differences in outcome across the studies resulted from the subsets of genes analyzed and a limited number of genes the studies had in common.
Pusztai et al. obtained gene expression profiles based on two different platforms and compared the ability of the two platforms to predict response to neoadjuvant chemotherapy. Both an oligonucleotide-based method and a cDNA-based method identified a gene set with high predictive accuracy. However, the genes included in the two gene sets were only partially overlapping, indicating that gene sets developed on one platform could not be readily exported to another.
Realtime reverse transcriptase-polymerase chain reaction (RT-PCR) facilitates analysis of RNA expression in paraffin-embedded tissue specimens.
Oncotype DX™ is a multigene RT-PCR assay designed to stratify patients with breast cancer based on their risk of relapse. This assay uses a mathematical algorithm to generate a recurrence score by using the level of expression of 16 cancer-related genes and five reference genes.The recurrence score was validated by the National Surgical Adjuvant Breast and Bowel Project (NSABP) in patients who had a history of node-negative, ER-positive breast cancer, and received tamoxifen in the adjuvant setting.The 10-year distant recurrence rate was 6.8%, 14.3%, and 30.5% in patients with a low, intermediate, and high recurrence score, respectively. Studies performed to establish the prognostic and predictive role of this assay in clinical management of breast cancer are on-going.
There are several outstanding questions regarding Oncotype DX concerning, for example, what its prognostic value is in patients who have not received any adjuvant systemic therapy or what its predictive role is in patients who receive hormone therapy or chemotherapy alone, or combined adjuvant systemic therapy. Primary breast tumor tissue specimens obtained from patients who participate in prospective randomized clinical trials designed to determine the role of adjuvant systemic therapy for early-stage breast cancer are an important resource to determine the clinical utility of this assay. Future studies should evaluate the predictive role of Oncotype DX and other novel assays in patients who undergo modern hormone therapy (i.e. aromatase inhibitors), and chemotherapy (e.g. taxanes).
Proteomics is another technology with great potential in identifying therapeutic targets in patients with breast cancer. Proteomics can be defined as the identification, characterization, and quantification of all proteins in a particular tissue, organ, or organism to provide accurate, comprehensive data about them. One of the methods most commonly used to study differences in protein expression between two specimens (e.g. cancer and normal tissue) is two-dimensional (2-D) gel electro- phoresis. Highly sensitive mass spectrometry methods are also currently being used to identify a greater number of lower abundance proteins that are differentially expressed in defined cell populations.
Matrix-assisted and surface-enhanced laser desorption/ ionization time-of-flight analyses enable high- throughput characterization of lysates from even a small number of tumor cells and may be best suited for clinical biomarker studies. Novel technologies still in development will enable identification of validated therapeutic targets in small biopsy specimens, including high-density protein, antibody, and lysate arrays.To date, no proteomics-based assays for assessment of prognosis in patients with breast cancer have been developed.
In summary, expression of ER, progesterone receptor (PR), and HER-2 in breast cancers helps guide therapy and should be assessed in all patients.
Prognostic indices that integrate clinical, histologic, and molecular parameters must be developed and validated in conjunction with novel bioinformatic methodologies (i.e. artificial intelligence) to aid clinical decision-making. High-throughput cDNA microarray and proteomic technologies allow analysis of the expression of literally thousands of genes and proteins at one time.Validation of these technologies in adequately powered prospective clinical trials will allow the integration of multiple molecular factors in risk assessment and management in individual patients with breast cancer. ■