Tumour markers are substances that can be measured in blood, tumour tissue or other body fluid and that aid cancer detection and/or management. Tumour markers are potentially useful in screening for early cancer (e.g. prostatespecific antigen (PSA) in prostate cancer), aiding diagnosis (tumour markers almost never replace histopathology for the primary diagnosis of cancer), determining prognosis, predicting likely response or resistance to therapy, post-operative surveillance and monitoring therapy in patients with advanced cancer.
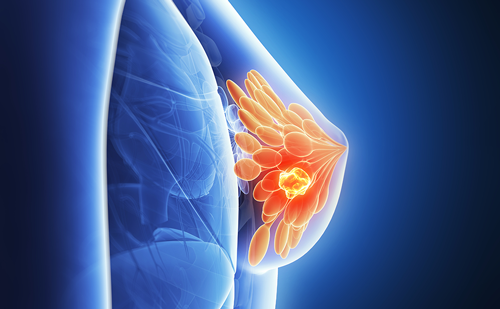
For breast cancer, the existing markers are of little value for screening or aiding early diagnosis. In contrast, markers are available for determining prognosis, predicting likely response to therapy, post-operative follow-up and monitoring therapy in metastatic disease. Prognostic and predictive marker use is usually determined on tumour tissue whereas surveillance and monitoring markers are measured in blood. The aim of this article is to review the role of both tissue and serum markers in the care of patients with breast cancer.
Tissue Markers
Hormone Receptors
Hormone receptors (i.e. oestrogen and progesterone receptors) are carried out in order to determine endocrine-sensitivity of newly diagnosed breast cancers. For hormone receptor-positive patients, endocrine therapy should be administered, i.e. tamoxifen and/or an aromatase inhibitor for postmenopausal patients and tamoxifen and/or ovarian suppression/ablation for premenopausal patients. Hormone receptor-negative tumours should not be treated with endocrine therapy but are candidates for treatment with adjuvant chemotherapy. It is generally recommended that both oestrogen and progesterone receptors be measured together as patients derive maximum benefit from hormone therapy when both receptors are present. While the primary use of hormone receptors is for selecting for endocrine sensitivity, oestrogen receptors may also be used to determine prognosis. Generally, for the first five years following diagnosis, receptor-positive patients have a better outcome than receptor-negative patients. However, as a prognostic factor, the impact of oestrogen receptor is relatively weak, especially in patients with lymph node-negative disease. Furthermore, the favourable prognostic impact of hormone receptors disappears after about five years of follow-up.
Human Epidermal Growth Factor Receptor-2
Human epidermal growth factor receptor-2 (HER- 2) is primarily measured in order to select patients for treatment with Herceptin (trastuzumab). Herceptin is a therapeutic monoclonal antibody directed against the HER-2 oncoprotein. When administered with chemotherapy to HER-2- positive patients, Herceptin significantly improved both progression-free and overall survival in patients with advanced breast cancer. When given either with or after chemotherapy to patients with HER- 2-positive early breast cancer, Herceptin reduced the risk of recurrence by approximately 50%.
As well as predicting response to Herceptin, HER- 2 may be used for determining prognosis in patients with breast cancer. Generally, patients with HER- 2-positive tumours have a worse outcome than those with HER-2-negative cancers. Indeed, in the 2005 St Gallen Consensus statement, assay of HER-2 was recommended for classifying risk in newly diagnosed breast cancer patients.
uPA and PAI-1
uPA and PAI-1 are two proteins that promote cancer invasion and metastasis. More than 20 independent studies have shown that high levels of uPA or PAI-1 in breast cancer are associated with aggressive disease and poor outcome. Most importantly, the prognostic value of these proteins has been validated in the highest available level evidence studies, i.e. in level I evidence studies. These high-level evidence studies included a multicentre randomised prospective trial carried out in 14 centres in Germany and a pooled analysis involving data from 18 different centres across Europe.
Currently, the main clinical use of uPA and PAI-1 is for selecting lymph node-negative breast cancer patients that may not need to undergo treatment with adjuvant chemotherapy, i.e. lymph nodenegative breast cancer patients with low levels of uPA and PAI-1 have such a good prognosis that the benefit of chemotherapy would be sufficiently small that they could avoid the toxic side effects and high costs of this therapy. On the other hand, patients with high levels of uPA and/or PAI-1 have a poor prognosis (similar to that of patients with three positive lymph nodes) and thus should be treated with adjuvant chemotherapy.
Serum Markers
The most useful serum markers in breast cancer are CA 15-3 (BR 27.29) and carcinoembryonic antigens (CEAs). As mentioned above, serum markers are mainly used in surveillance following surgical resection of the primary cancer and monitoring therapy when patients develop recurrent or metastatic disease. For both these applications, serial determinations of marker(s) are necessary.
Postoperative Surveillance
Approximately 25% of patients with surgically outcome. Indeed, studies carried out over 10 years ago concluded that intensive follow-up of breast cancer patients did not benefit them compared with minimal follow-up. These old studies had a number of limitations, including:
- use of older and less sensitive biochemical tests, such as alkaline phosphatase, aspartate transaminase, gamma glutamyl transferase, bilirubin, calcium and creatinne, rather than the newer tumour markers such as CA 15-3 and CEA;
- use of older radiological procedures rather than newer procedures such as computed tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography (PET) scanning; and
- most of the reports comparing outcome in control and intensively followed-up patients predate the availability of new treatments for recurrent/metastatic breast cancer such as the taxanes, the new generation of aromatase inhibitors and Herceptin.
The relevance of these older studies to the modern management of breast cancer is thus unclear.
According to the European Group on Tumour Marker (EGTM) Guidelines, serial CA15-3 and CEA determinations are recommended for the early detection of recurrence in asymptomatic patients who had undergone curative surgery for primary breast cancer, if the detection of recurrent or metastatic disease would alter clinical management. Other expert panels such as the American Society of Clinical Oncology (ASCO), however, do not recommend routine use of tumour markers in the post-operative surveillance of newly diagnosed breast cancer patients.
Monitoring Therapy in Advanced Disease
Following the commencement of therapy for advanced disease, it is important to know as quickly as possible if the patient is responding to the treatment. If the patient is benefiting, clearly, treatment should be continued. If, on the other hand, treatment is not effective, an alternative therapy might be given. If an alternative therapy is unavailable, these patients could be willing to participate in clinical trials or they could decide to avoid further therapy.A convenient and relatively inexpensive approach for helping to establish response is by measuring markers such as CA 15-3 or CEA. Generally, decreasing marker levels correlate with tumour response, while increasing markers levels correlate with tumour regression. According to the EGTM guidelines, markers should be measured prior to every chemotherapy course and at least at three-monthly intervals for patients receiving hormone therapy. The EGTM defines an increase in marker concentration of at least 25% to be significant. It is recommended that such an increase be confirmed with a second specimen obtained within a month. If the increase is confirmed, this provides evidence of progressive disease. Similarly, a confirmed decrease in serum levels of more than 50% was stated to be consistent with tumour regression.
In contrast to the EGTM recommendations, the ASCO guidelines state that neither CA 15-3 nor CEA should be routinely used for monitoring therapy in patients with advanced breast cancer.
Also, according to these guidelines:
Conclusion
It is clear from the above that tumour markers play a key role in the care of patients with breast cancer. Tissue markers such as hormone receptors and HER- 2 are now mandatory in determining prognosis and therapy planning. For post-operative surveillance, serum markers such as CA 15-3 and CEA can be used to detect recurrent or metastatic disease at an early stage. These serum makers can also aid the monitoring of therapy in patients undergoing treatment for advanced disease. Markers are particularly important in monitoring disease that cannot be evaluated by standard radiological criteria (e.g. those with irradiated lesions, pleural effusion, ascites, lytic bone disease and sclerotic bone disease).