Until recently, treatment options for metastatic colorectal cancer (CRC) have been limited to a cytotoxic chemotherapy with or without an anti-epithelial growth-factor receptor (EGFR) monoclonal antibody, namely cetuximab and panitumumab, or an anti-angiogenic agent such as bevacizumab, aflibercept or ramucirumab. For subsequent lines of treatment, the tyrosine kinase inhibitor regorafenib is an important part of the therapeutic armamentarium.1 Targeted treatment in metastatic CRC has traditionally been limited to the use of anti-EGFR agents in association with chemotherapy in rat sarcoma virus (RAS) wild-type tumours.
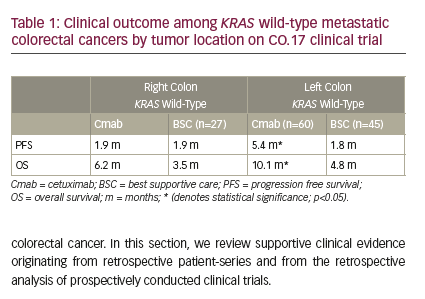
Despite their target being located on the cell surface, the clinical activity of anti-EGFR antibodies does not correlate with EGFR membrane expression; instead, alterations in its downstream signalling pathway, most notably in the RAS genes, can bypass EGFR inhibition and negate the therapeutic benefit.2,3 For this reason, confirmation of pan-RAS wild-type status is required before starting treatment with an anti-EGFR agent. Tumour sidedness also appears to play a pivotal role, with right-sided tumours reporting scarce benefit from anti-EGFR agents, despite wild-type RAS status.4
Recent studies have enhanced knowledge of the molecular complexity of CRC, possibly improving the stratification and clinical management of patients with CRC. Guinney et al. reported a consensus molecular classification for CRC based on gene-expression profiling, identifying four main subtypes: microsatellite-instability (MSI) immune, canonical, metabolic and mesenchymal.5 Interestingly, right-sided tumours are more frequently classified as MSI immune or metabolic subtypes. While these consensus molecular subtypes are not currently evaluated in clinical practice, nor routinely employed to guide treatment choice, the identification of specific molecular alterations have started to pave the way to future possibilities for personalized treatment. In particular, personalized treatment strategies are being explored in clinical trials for a variety of molecular alterations: HER2 amplification (HERACLES-A, MyPathway), KRAS G12C mutation (CodeBreaK100, KRYSTAL-1), NTRK gene fusions (NAVIGATE), MSI (KEYNOTE-177) and, relevant to the scope of our review, BRAF V600E mutation (BEACON CRC, ANCHOR CRC, BREAKWATER, MODUL).6–15
The purpose of this review is to better delineate the novel treatment options in BRAF-mutant metastatic CRC.
BRAF mutations in colorectal cancer
The rapidly accelerated fibrosarcoma (RAF) protein family comprises three main isoforms (ARAF, BRAF and CRAF), with BRAF being the most frequently mutated.16 Moreover, BRAF is involved in the RAS/RAF/MEK/extracellular signal-regulated kinases (ERK) signalling pathway, also known as the mitogen-activated protein kinase (MAPK) cascade, driving cell survival, proliferation and differentiation.16 Mutations in BRAF are present in approximately 10% of patients with metastatic CRC, and are associated with right-sided tumours, age (>60 years), gender (female), high grade of anaplasia, and the presence of lymph nodal and peritoneal metastases.17 The most frequent alteration observed is the V600E kinase-activating mutation, representing approximately 90% of cases.18 Generally, BRAF mutations are associated with a worse prognosis in CRC, as shown by Venderbosch et al. in a pooled analysis of data from the CAIRO, CAIRO2, COIN and FOCUS studies.19 Other less frequent mutations, such as BRAF D594G or G596N, are known to be prognostically favourable in CRC, resulting in reduced kinase activity.20 BRAF mutations are also closely associated with sporadic MSI and can be detected in 40–60% of MSI-high CRC cases; this overlap can be explained by prevalence of the CpG island methylator phenotype (CIMP) in BRAF-mutant cancers, leading to hypermethylation of the MLH1 promoter, and thus to a microsatellite-unstable phenotype.21 On the other hand, no BRAF-mutated cases have been reported with MSI associated with Lynch syndrome.17
Interestingly, the unfavourable prognostic effect of BRAF mutations appears to be mitigated, not deleted, by MSI, as shown by Manthravadi et al. in a recent meta-analysis that concentrated on the non-metastatic setting.22
BRAF mutations have been reported as mutually exclusive with RAS mutations, and this could be suggestive of a similarly detrimental effect on the efficacy of EGFR-directed therapies through downstream activation of the pathway. It has, however, been suggested that mutations other than V600E may not show the same activation behaviour, but no robust data have been provided to confirm this issue.23,24
Current treatment landscape for
BRAF V600E-mutant colorectal cancer
In 2016, the TRIBE study confirmed FOLFOXIRI (fluorouracil, leucovorin, oxaliplatin and irinotecan) + bevacizumab as an highly effective first line treatment first-line treatment of metastatic CRC, based on a median overall survival (OS) benefit (median OS 19.0 months with FOLFOXIRI + bevacizumab versus 10.7 months with FOLFIRI [folinic acid, fluorouracil and irinotecan] + bevacizumab).25 However, in the same trial, a subgroup analysis failed to identify benefits in the BRAF-mutation subgroup of patients. An individual patient data meta-analysis appeared to confirm that the greatest advantage from the triplet + bevacizumab combination was observed in patients with the KRAS mutation (who are ineligible for EGFR-directed therapies), while those carrying the BRAF mutation did not present significant benefits.26
The aim of the phase II FIRE-4.5 study was to determine if cetuximab or bevacizumab were the best drugs to be combined with FOLFOXIRI in patients with BRAF V600E-mutated tumours, a population in which first-line prospective data were lacking.27 Based on a review of the literature, the use of EGFR-directed therapies in this population is controversial, and the trial officially turned out negative, only detecting a statistically significant progression-free survival (PFS) advantage with bevacizumab versus cetuximab.27 Thus, conventional chemotherapy associated with biologic agents appears to be globally unsatisfactory for this subgroup of patients.
Attempts to improve the dismal prognosis of patients with BRAF-mutated metastatic CRC were then concentrated on precision oncology. The development of BRAF inhibitors specifically targeted at the V600E mutation appeared to identify a strategy to target the MAPK cascade in these patients. Nevertheless, BRAF inhibition alone was observed to remove inhibitory feedback on EGFR expression, thus leading to increased EGFR density on the cell surface. Thus, shunted signal transduction through CRAF or other associated signalling pathways deleted the effect of the blockade.28,29 For these reasons, a rationale for multiple inhibition emerged. For instance, the phosphatidylinositol-3-kinase (PI3K)/mammalian target of rapamycin (mTOR) signalling pathway is known to be constitutively activated in a significant portion of patients with CRC (30%) and also, specifically, in BRAF-mutant CRC, thus emerging as a possible resistance mechanism to BRAF-directed monotherapy.30,31 Based on these notions, Coffee et al. explored the efficacy of combined BRAF and PI3K/mTOR inhibition in genetically engineered mouse models, with interesting signals of activity.31 Similarly, preclinical data reported by Prahallad et al. have shown that a combination of BRAF and EGFR inhibitors seems to produce a synergistic effect in CRC xenografts.29
Clinical data on triple targeting of PI3K, BRAF and EGFR come from van Geel et al., who tested the combination of encorafenib and cetuximab with or without the PI3K catalytic subunit a (PI3KCA) inhibitor alpelisib in the setting of a phase Ib dose-escalation study for metastatic BRAF mutant CRC, with or without PIK3CA alterations.33 Results showed promising clinical activity with an overall response rate (ORR) of 18% and 19% and a median PFS of 3.7 months and 4.2 months, with the doublet and triplet combination, respectively, and an acceptable toxicity.33
In a subsequent phase II trial, 102 patients were randomized to either encorafenib + cetuximab or encorafenib + cetuximab + alpelisib, evaluating PFS as the primary endpoint.34 While the addition of alpelisib appeared to increase toxicity, the clinical activity was promising, with a mean PFS of 4.2 months with the doublet and 5.4 months with the triplet. OS was evaluated as a secondary endpoint in an interim analysis, resulting in a median OS of 15.2 months with the triplet versus not reached with the doublet.34 More data are required on this treatment approach.
Likewise, the combined inhibition of BRAF and MEK has a solid preclinical rationale, as evaluated by Corcoran et al.35 For this reason, chemotherapy-free doublet or triplet regimens associating a BRAF inhibitor with a MEK inhibitor, an anti-EGFR antibody or both were investigated. Hyman et al. evaluated this approach in a phase II basket trial, where 37 heavily pre-treated patients with CRC received the BRAF inhibitor vemurafenib either alone or in association with cetuximab, resulting in an ORR of 0% and 4%, and disease stability in 50% and 69%, respectively; median PFS in the combination group was 3.7 months and median OS was 7.1 months.36 Similarly, a pilot trial by Yaeger et al. in 15 patients tested the combination of vemurafenib and panitumumab in pre-treated metastatic CRC, with an acceptable safety profile and modest clinical activity; tumour regression was observed in 10 out of 12 patients, but a formal partial response was only defined in two patients, with two more patients obtaining disease stability lasting more than 6 months.37
Doublet therapy with the BRAF inhibitor dabrafenib and the MEK inhibitor trametinib was tested by Corcoran et al. in 43 patients with BRAF-mutant CRC, obtaining interesting signals of activity, with an ORR of 12%, including one complete response, and disease stability in 56% of the study population.38
Based on these data, a new trial explored BRAF and EGFR inhibition with the doublet of dabrafenib + panitumumab, the triplet of dabrafenib + trametinib + panitumumab, or an alternating doublet of trametinib + panitumumab, in 142 patients with BRAF V600E-mutant CRC.39 The ORR was 0% for trametinib + panitumumab, 10% for dabrafenib + panitumumab and 21% for the triplet, although this greater activity was also associated with increased toxicity. Median PFS was 2.6 months (95% confidence interval [CI], 1.4–2.8 months) with trametinib + panitumumab, 3.5 months (95% CI, 2.8–5.8 months) with dabrafenib + panitumumab, and 4.2 months (95% CI, 4.0–5.6 months) with the triplet.39
The BEACON CRC phase III trial assessed the encorafenib + binimetinib + cetuximab triplet regimen and the encorafenib + cetuximab doublet regimen versus the investigators’ choice of irinotecan + cetuximab or FOLFIRI + cetuximab, in 665 patients with BRAF V600E-mutated metastatic CRC progressing after first- or second-line treatment and who had not received anti-EGFR, anti-BRAF or anti-MEK agents.12 Primary endpoints were OS and ORR in the triplet group versus the control group. The secondary endpoint of OS in the doublet group versus the control group was also observed. The median OS was 9.3 months (95% CI, 8.2–10.8 months) for the triplet group and 5.9 months (95% CI, 5.1–7.1) for the control group (hazard ratio [HR] versus control, 0.60 [95% CI, 0.47–0.75]). Median OS for the doublet group was 9.3 months (95% CI, 8.0–11.3 months; HR versus control, 0.61 [95% CI, 0.48–0.77]). Confirmed ORR was 26.8% (95% CI, 21.1–33.1%) for the triplet group, 19.5% (95% CI, 14.5–25.4%) for the doublet group and 1.8% (95% CI, 0.5–4.6%) for the control group. The adverse-event profile was favourable, with grade 3 or higher adverse events in 65.8%, 57.4% and 64.2% of patients in the triplet, doublet and control groups, respectively, and a discontinuation rate due to an adverse event of 9%, 9% and 11%, respectively. One fatal event in the triplet arm and two in the control arm were possibly treatment related.12
In summary, the combination of encorafenib and cetuximab improved survival and tumour response with a safety profile not significantly different from standard treatment; however, the addition of binimetinib did not show any benefits in terms of OS and was associated with added toxicity. Patients with high C-reactive protein levels, an Eastern Cooperative Oncology Group performance status of 1, an incomplete primary tumour resection, and metastatic involvement of three or more organs may be candidates for greater benefit from the triplet combination.12
Interestingly, an additional analysis demonstrated that patients treated with the double combination showed similar OS regardless of prior therapies (including bevacizumab) or the duration of prior therapy used.40
The BEACON CRC trial thus provided the first evidence of improvement in survival from a chemotherapy-free targeted therapy in a prospectively biomarker-defined population of patients with metastatic CRC. This led to regulatory approval by the European Medicines Agency (EMA) for the combination of encorafenib + cetuximab in pre-treated, BRAF V600E -mutated metastatic CRC in June 2020.12
Preliminary results from the phase II ANCHOR CRC trial were recently presented as an abstract at the 2021 European Society for Medical Oncology World Congress on Gastrointestinal Cancer.13 The aim of the trial was to translate the encouraging data from BEACON CRC into the first-line setting, evaluating the combination of encorafenib + binimetinib + cetuximab in a treatment-naive population of 95 patients with BRAF V600E-mutated CRC. Preliminary results showed an ORR of 47.8% and a median OS of 17.2 months, with grade 3 or higher adverse events in 69.5% of patients, thus confirming the activity of the combination in the absence of new safety signals.13
The BREAKWATER phase III study is a further step towards first-line use of targeted drugs in this setting.14 The trial has a safety lead-in phase, enrolling patients with BRAF V600E-mutated metastatic CRC who have received no more than one line of treatment; this is followed by a phase III trial evaluating three separate arms in a fully treatment-naive population. Arm A will receive therapy with encorafenib + cetuximab; arm B will receive the doublet plus standard chemotherapy with FOLFOX (folinic acid, fluorouracil, and oxaliplatin) or FOLFIRI; and the control arm will receive standard chemotherapy alone according to the physician’s choice, with or without an anti-VEGF antibody. The primary endpoint is PFS in arm A and arm B versus the control arm, respectively; OS will also be evaluated as a key secondary endpoint.14
The phase II MODUL trial evaluated novel agents as biomarker-driven maintenance therapy in patients with metastatic CRC treated with FOLFOX + bevacizumab in the first line.15 It comprised four experimental treatment cohorts and a control cohort employing fluoropyrimidine + bevacizumab. The BRAF-mutated cohort received treatment with vemurafenib + cetuximab + 5-fluorouracyl and leucovorin; the primary endpoint was PFS. At a median follow-up of 16.4 months, median PFS was 11.6 months in the control arm and 10.0 months in the experimental arm; ORR was 25% versus 50%, respectively.41 The trial was closed prematurely due to events unrelated to the BRAF-mutated cohort, so the results are therefore purely descriptive; however, an exploratory genomic analysis carried out on sequential liquid biopsies identified mutations in the MAPK pathway as possible drivers of acquired resistance to the experimental treatment.15
Future directions
The treatment landscape of BRAF-mutant CRC is rapidly changing towards treatments that have demonstrated improved outcomes in this prognostically unfavourable population.12,13 Moreover, on-going trials will also enhance comprehension and data on the efficacy of the new target therapy combinations in the first-line setting. Therapeutic intervention on multiple blockades along the MAPK pathway is efficient in different experiences; however, pharmacological options for targeting the specific proteins along the signalling cascade are evolving, and selecting the best targets and agents to optimize efficacy and minimize toxicity will be an important issue to be considered for future research.12,29,32–39
Molecular profiling is making a difference: a growing knowledge of the molecular landscape of these tumours, which were traditionally handled according to a ‘one size fits all’ approach, is making a personalized approach more feasible. Additionally, unravelling the interplay of clinical, immunological and molecular features will become fundamental for both stratification of patients and treatment choices. In this perspective, MSI and BRAF V600E-mutant CRC is particularly relevant: on one hand, the exact prognostic outlook of this entity is yet to be clarified, on the other hand, BRAF mutations do not seem to hinder response to immunotherapy, which opens the way to a possible sequencing strategy.11
The landscape of clinical and molecular parameters and their evolution over the course of the disease´s history is fundamental, as it allows clinicians to monitor tumour progression and resistance through non-invasive approaches. Despite the inconclusive results of the MODUL trial, its strategy of longitudinal monitoring through liquid biopsy is likely to be a part of future investigation methods.15 The inclusion of patients in clinical trials and the incorporation of these techniques in prospective studies must be a priority to better understand and defeat this illness.