For the past 10 years, many cytotoxic and targeted agents have been pitted against or combined with gemcitabine in randomized phase III trials and no drug has been shown to be superior to single-agent gemcitabine. Luckily, in the past year, for the first time, two large, randomized phase III studies in APC—capecitabine plus gemcitabine versus gemcitabine, and erlotinib plus gemcitabine versus gemcitabine—have demonstrated the superiority of a gemcitabine-containing combination over single-agent gemcitabine. In this paper we will review the current advancement in PC treatment.
Resectable Pancreatic Cancer
Ten percent of patients have resectable disease at the time of PC diagnosis. Prognosis of patients after complete resection of node-negative cancer is poor, with three-year disease-specific survival rate at 27% (95% confidence interval (CI): 23–32%) and MS of 15–19 months.3 The treatment plan in the adjuvant setting is currently dependent on which side of the Atlantic you are located: chemotherapy alone is mostly used in Europe—European Study Group for Pancreatic Cancer-1 (ESPAC-1), Charité Onkologie Clinical-001 (CONKO-001)—while chemoradiation therapy (CRT) is the current standard in the US—Gastrointestinal Study Group (GITSG), Radiation Therapy Oncology Group 9704 (RTOG 9704). Adjuvant Therapy with Chemotherapy and External Beam Radiotherapy
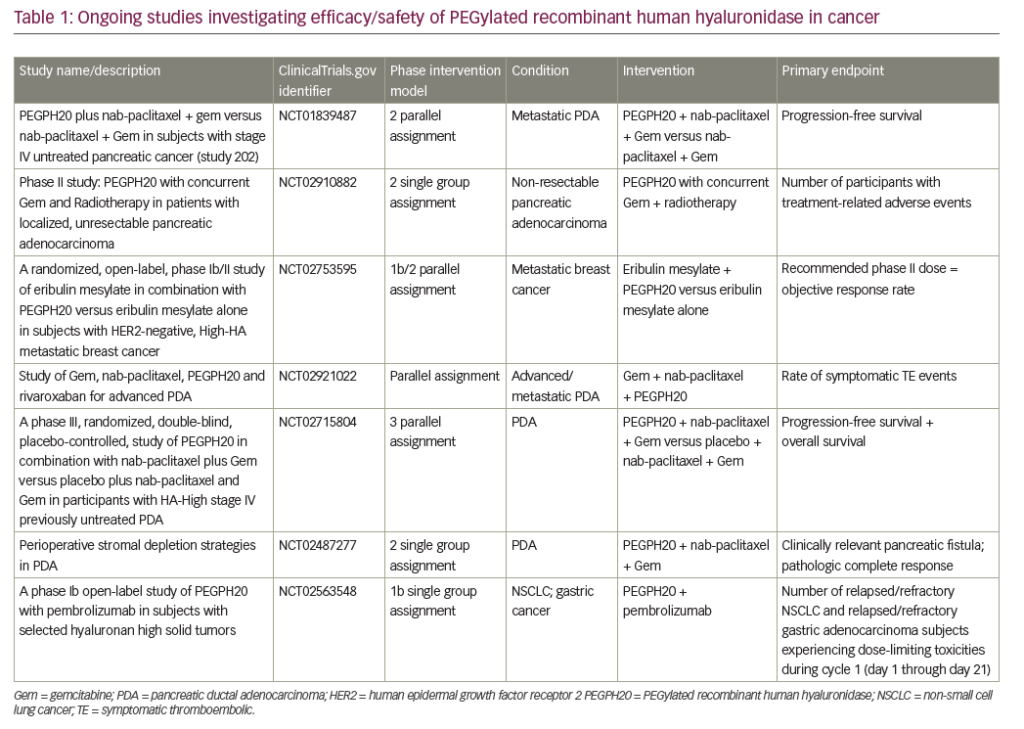
One rationale for adjuvant CRT comes from the high risk of local and systemic disease recurrence and overall poor prognosis. One of the first studies to support adjuvant CRT in patients with resected PC was conducted by GITSG. This small study (n=43) showed survival benefit (MS: 20 versus 11 months; fiveyear survival: 18 versus 8%) in patients who received bolus 5-FU with radiation therapy (XRT) for one year compared with patients who did not.4 However, this study was criticized for small sample size due to early closure of the trial. The European Organization of Research and Treatment of Cancer (EORTC) compared post-operative combined 5-FU (25mg/kg/day continuous infusion for five days every four weeks) and external beam radiotherapy (EBRT) (split course 40Gy) with observation only in patients with resected pancreatic and periampullary cancer. Klinkenbiji et al. were able to show a trend toward benefit in terms of MS (24.5 versus 19 months; p=0.208). The subgroup analysis looking only at PC patients showed a trend toward benefit in MS (17.1 versus 12.6 months; p=0.099).5 This study was also criticized for suboptimal XRT—lower doses and split courses—that may have allowed cancer repopulation between courses, thereby underestimating the benefit of CRT. The trial ESPAC-1 was a two-by-two factorial designed study comparing adjuvant concurrent CRT (bolus 5-FU/split-course radiation), chemotherapy alone (5-FU/Leucovorin (LV)), CRT followed by chemotherapy, and observation. The chemotherapy-only arm had statistically significant benefit over the observation arm in MS (20.1 versus 15.5 months; p=0.009). However, the CRT arm showed worse MS (15.9 versus 17.9 months; p=0.05).6 The RTOG 9704 study randomized 538 resected PC patients to evaluate the benefit of adding gemcitabine to infusional 5-FU combined with XRT (5- FU+XRT). One arm received 5-FU+XRT and the other arm was treated with gemcitabine before and after 5-FU+XRT. Although there was no significant difference when pancreatic body and tail cancers were all included, patients with pancreatic head tumors (n=380) showed benefit in MS (18.8 versus 16.7 months; p=0.047).7 While the benefit of XRT was inconclusive in randomized trials (see Table 1), two recent large, uncontrolled studies support the benefits of adding radiation. Greco et al. analyzed 2,636 patients with resected PC of whom 42.6% received radiation and 57.4% did not. After a mean follow-up of 19 months, patients who underwent adjuvant radiation had improved median overall survival (OS) (18 versus 11 months; p<0.01).8 Corsini et al. performed a retrospective review of 472 patients who underwent complete resection with negative margins for invasive adenocarcinoma of the pancreas from 1975 to 2005 at the Mayo Clinic. The authors concluded that the addition of adjuvant concurrent CRT improves OS after complete resection of PC. Patients who received adjuvant CRT had longer median OS over patients who did not receive radiotherapy (2.1 versus 1.6 years; p=0.001).9
5-FU = 5-fluorouracil; XRT = radiation therapy; CXRT = combined chemoradiation therapy; MS = median survival; HR = hazard radio; OS = overall survival; DFS = disease-free survival.
XRT = radiation therapy.
Chemotherapy Alone
In the CONKO-001 study, Oettle et al. randomized 368 patients with resected PC to gemcitabine or observation for six months. Tumor prognostic characteristics were similar in both arms. This trial showed a statistically significant disease-free survival (DFS) benefit (13.4 versus 6.9 months; p<0.001) of gemcitabine over observation (see Table 1). Treatment with gemcitabine caused a trend toward OS benefit (22.1 versus 20.2 months; p=0.06).10 This benefit of chemotherapy was consistent with the result from the ESPAC-1 trial, which showed the benefit of 5-FU/LV over no adjuvant therapy in PC patients (MS 19.7 versus 14 months) who had complete resection.6 The role of gemcitabine as a single agent will further be defined by the ongoing ESPAC-3 study, which is a randomized phase III study comparing observation versus 5-FU versus gemcitabine in the adjuvant setting of PC.Locally Advanced Pancreatic Cancer
Approximately 30% of patients have locally advanced disease at the time of diagnosis with MS of six to 10 months.11 PCs are deemed unresectable when the following features are present:
• involvement of superior mesenteric artery or celiac axis;
• absence of vascular flow through the superior mesenteric vein–portal vein (SMV–PV) confluence;
• complete encasement of SMV–PV confluence leading to vascular thrombosis and cessation of blood flow in the SMV–PV;
• celiac axis involvement/encasement with tumor or direct involvement of inferior vena cava or aorta;
• extrapancreatic involvement; or
• distant metastases.
Combined Modality with Chemoradiation Therapy
5-FU-based Chemoradiation Therapy
5-FU-based CRT has been the mainstay approach since the Mayo Clinic published randomized trial data showing prolonged MS by addition of 5-FU to XRT in 1969.12 This result was supported by GITSG when they reported a significant survival benefit (one-year survival rate 40 versus 10%) of 5-FU-based CRT over radiation only.13 In the US, commonly accepted practice is to use infusional 5-FU rather than bolus 5-FU as a radiosensitizer based on experience with other gastrointestinal cancers. A few small studies have demonstrated that capecitabine has the potential to be a substitute for infusional 5-FU in the treatment of locally advanced pancreatic cancer (LAPC).14,15
Gemcitabine-based Chemoradiation Therapy
Gemcitabine-based CRT has been investigated since the benefit of gemcitabine over 5-FU in APC was reported. Optimal administration strategies for this regimen are still being investigated in clinical-trial settings. Due to high toxicity with this regimen in early trials, the Cancer and Leukemia Group B (CALGB) conducted a phase II trial of concurrent XRT (50.4Gy) and low-dose weekly gemcitabine (40mg/m2 twice weekly) in patients with LAPC. This regimen rendered a disappointing median OS rate of 8.2 months.16 However, in patients with an Eastern Co-operative Oncology Group (ECOG) performance status score of zero, MS was 13.7 months. The Hoosier Oncology Group (HOG) treated patients with LAPC with weekly gemcitabine (600mg/m2) with concurrent XRT (50.4Gy) followed by gemcitabine monotherapy. This regimen showed more favorable side-effect profiles along with a promising one-year survival rate of 31.1%.17
Paclitaxel-based Chemoradiation Therapy
Paclitaxel has shown activity against LAPC in combination with XRT. The Brown University Oncology Group reported a 26% response rate in 42 patients with LAPC.18 A phase II trial with the combination weekly paclitaxel plus XRT has been conducted (RTOG 9812) and data are maturing.19 Newer technologies in XRT, including three-dimensional conformal RT, which allows reduction of radiation fields and optimization of radiation-sensitizing chemotherapy, will improve treatment of LAPC in the future.
Is the Therapeutic Index Better with Gemcitabine Radiation Therapy than with 5-FU Radiation Therapy?
A review of the literature suggests significantly higher severe toxicity rates with gemcitabine than with 5-FU when used as a radiosensitizer in LAPC. Median and one-year survivals were not significantly different with the use of concurrent gemcitabine versus 5-FU in an exploration published by MD Anderson Cancer Center. A small number of patients with (minimal arterial involvement) unresectable disease had margin-negative resections after treatment with gemcitabine-XRT. These possible benefits and the high rate of severe toxicity define a very narrow therapeutic index for concurrent gemcitabine-based chemo-XRT given by this schedule of administration. Despite the absence of any randomized studies in LAPC comparing capecitabine with 5-FU, capecitabine offers a more convenient and relatively less toxic radiosensitizer than intravenous 5-FU.
Chemotherapy Alone
A randomized phase III trial by Chauffert et al. evaluated whether 5-FU-based CRT can improve benefits of gemcitabine monotherapy. Patients with LAPC were randomized 1:1 between the CRT arm (60Gy in six weeks, 2Gy/fraction, concomitant with 5-FU, 300mg/m2/24h as a continuous infusion, days one to five every week and cisplatin, 20mg/m2/d, days one to five at week one and week five) or gemcitabine (1000mg/m2 weekly on a schedule of seven weeks on and one week off) as induction therapy. Both arms received gemcitabine 1000mg/m2 weekly on a schedule of three weeks on and one week off as maintenance therapy. This study was closed early due to the lower survival rate in the induction CRT arm compared with the gemcitabine-alone arm (MS: 8.4 versus 14.3 months).20 One potential reason for this difference is that the toxicity from CRT resulted in decreased used of maintenance gemcitabine. Patients with LAPC have been included in clinical trials for metastatic pancreatic cancer (MPC), and chemotherapy alone has been the accepted treatment of LAPC. Recent trials with various chemotherapy regimes in PC—including LAPC—patients have suggested that the palliative and survival benefits from chemotherapy alone may be equivalent to CRT. Various chemotherapy regimen tested in this setting will be discussed in the following section.
Advanced Pancreatic Cancer
Up to 60% of patients have metastatic disease at the time of diagnosis. The MS rates of these patients are dismal at between three and six months.2 After the approval of gemcitabine in 1997 (see Table 3), many cytotoxic and targeted agents have been pitted against, or combined with gemcitabine in randomized phase III trials (see Tables 4 and 5). No drug was shown to be superior to single-agent gemcitabine. This bleak landscape finally changed after two large, randomized, phase III studies in APC demonstrated the superiority of a gemcitabine-containing combination over single-agent gemcitabine: capecitabine plus gemcitabine (GEMCAP) and erlotinib plus gemcitabine, as detailed below.
Cytotoxic Agents
Gemcitabine
Gemcitabine has been compared with 5-FU in APC patients and showed its superiority in clinical response rates (24 versus 5%) and one-year survival rates (18 versus 2%) in a randomized study by Burris HA et al.21 (see Table 3). In addition to the survival benefit, gemcitabine was also superior to 5-FU in producing clinical benefit response (see Figure 1). This study led to the approval of gemcitabine as a first-line chemotherapy agent.21
Fixed Dose Rate versus Conventional 30-minute Infusion of Gemcitabine
The benefit of fixed dose rate (FDR) gemcitabine versus the standard 30-minute infusion schedule, which was proposed in a phase II trial, was contradicted by a US intergroup randomized phase III trial (ECOG-6201), which showed no difference between the two schedules.22 Increased myelosuppression is associated with FDR gemcitabine infusion (neutropenia, thrombocytopenia). Gemcitabine versus Gemcitabine/Platinum
Gemcitabine/oxaliplatin (GEMOX) showed encouraging results in a phase II trial and led to randomized trials comparing GEMOX with gemcitabine monotherapy. The Groupe d’Etude et de Recherche Clinique en Oncologie et Radiothérapie/Italian Group for the Study of Gastrointestinal Tract Carcinomas (GERCOR/GISCAD) intergroup study compared standard gemcitabine monotherapy versus FDR GEMOX in patients with LAPC and MPC. GEMOX showed longer progression-free survival (PFS) (5.8 versus 3.7 months; p=0.04) than that of gemcitabine. GEMOX also rendered better response rates (27 versus 17%; p=0.04). There was a trend toward MS benefit (9 versus 7.1 months; p=0.13). Toxicities from both arms were acceptable, while GEMOX was more myelosuppressive and caused more peripheral neuropathies.23 The major criticism for this study was that it compared a 30-minute infusion with an FDR infusion in GEMOX regimen. The US intergroup trial ECOG 6201 compared standard 30-minute gemcitabine versus FDR gemcitabine versus GEMOX. Preliminary data from this study presented at the American Society of Clinical Oncology (ASCO) 2006 failed to show significant advantages of GEMOX to gemcitabine monotherapy.22 Other gemcitabine/platinum combinations gave rise to benefits. A gemcitabine and cisplatin combination showed significant improvement against disease progression and in response rates. Heinemann et al. also showed 2.2 months’ prolongation of PFS (p=0.53) by the addition of cisplatin to gemcitabine.24
Gemcitabine versus Gemcitabine + Fluoropyrimidines
While phase III randomized trials did not show any benefit of adding 5-FU (infusional or bolus) to gemcitabine, the addition of oral fluoropyrimidine— capecitabine—to gemcitabine (GEMCAP) showed promising results. A multinational randomized trial by Herrmann et al. reported no advantage of adding capecitabine; however, subgroup analysis showed the benefit of GEMCAP to patients with good performance status (hazard ratio (HR): 0.76; p<0.03).25 Another phase III randomized trial by Cunningham compared single-agent gemcitabine with gemcitabine three times weekly plus capecitabine 1660mg/m2 daily for 21 days in every 28-day cycle. The addition of capecitabine doubled the response rate (14 versus 7%; p=0.008) and improved OS (HR: 0.80; p=0.026). The incidence of myelosuppression was higher in the combination arm, and hand–foot syndrome was noted only in the combination arm.26 The final results of the study are anxiously awaited. Addition of S-1, a novel oral fluoropyrimidine derivative, to gemcitabine in patients with MPC showed promising activity in a phase II study of 54 patients. Response rates were 44% and MS was 10.1 months with an acceptable toxicity profile. A randomized phase III trial is being undertaken.27
Targeted Agents
Based upon the biology of PC, the following classes of targeted agents are being investigated actively: epidermal growth factor receptor (EGFR) inhibitors, vascular endothelial growth factor receptor (VEGFR) inhibitors, farnesyltransferase inhibitors, matrix metalloproteinase inhibitors, and cyclooxygenase-2 (COX-2) inhibitors.
Epidermal Growth Factor Receptor Inhibitors
The National Cancer Institute of Canada randomized patients with LAPC and MPC to gemcitabine/erlotinib and gemcitabine/placebo. The addition of erlotinib resulted in a statistically significant benefit in survival rate (HR: 0.81; 95% CI: 0.67–0.97; p=0.025). Improvement of MS was from 5.9 to 6.4 months, and one-year survival rate improved from 17 to 24%.28 This study led to the approval of erlotinib by FDA—the first biologic plus gemcitabine combination that showed benefit after the efforts of a decade. A rash was the most common toxicity associated with erlotinib and correlated with the expected outcome.Cetuximab, an anti-EGFR chimeric monoclonal antibody, in combination with gemcitabine showed promising activity in a phase II trial by Xiong et al.29 Forty-one patients with LAPC and MPC were treated with this regimen and showed 12.2% relative risk (RR), median OS of 7.1 months, and oneyear OS of 31.7%. Cetuximab was dosed with 400mg/m2 loading followed by a 250mg/m2 weekly dose. Gemcitabine was given at 1000mg/m2 on a schedule of seven weeks on and one week off. This regimen was well tolerated with the most common side effects being neutropenia (39%) and asthenia (22%).29 In an effort to confirm this result, a phase III randomized trial is being conducted by the Southwest Oncology Group (SWOG).30 The primary study end-point of this trial is OS. Unfortunately, in April 2007 ImClone Systems and Bristol-Myers Squibb (BMS) announced that this phase III study of cetuximab plus gemcitabine in patients with locally advanced unresectable pancreatic cancer or MPC did not meet its primary end-point of improving OS. The open-label, randomized study compared cetuximab plus gemcitabine with gemcitabine alone in more than 700 patients with PC in the first-line treatment setting. The study was conducted in centers throughout the US and Canada. Seven hundred and sixty-six patients (735 eligible) with a median age of 64 (30–91) years were enrolled by SWOG and the Cancer Trials Support Unit (CTSU) between January 2004 and April 2006. Of those, 51% were male, 21.5% had locally advanced disease, and 13% had PS of 2. The study closed with full accrual. The median survival was six months in the gemcitabine arm and 6.5 months in the gemcitabine plus cetuximab arm for an overall HR of 1.09 (95% CI: 0.93–1.27; p=0.14). The corresponding PFS was three months and 3.5 months for gemcitabine and gemcitabine plus cetuximab arms, respectively (HR: 1.13; 95%CI: 97–1.3; p=0.58). This study failed to demonstrate a clinically significant advantage of the addition of cetuximab to gemcitabine for overall survival, PFS, and response in advanced PC. Kullmann et al. recently presented an abstract—at the 2007 Gastrointestinal Cancers Symposium—of a phase II trial testing first-line GEMOX plus cetuximab (GEMOXCET) in MPC patients. The addition of cetuximab to GEMOX was well tolerated and exhibited a high response rate (38%). Myelosuppresion and rashes were commonly noted toxicities with this regimen.31
Vascular Endothelial Growth Factor Receptor Inhibitors
Based on the encouraging results of a phase II study, gemcitabine plus bevacizumab, a recombinant humanized monoclonal antibody to VEGFR, was tested in a phase III randomized trial by CALGB. A total of 602 patients with unresectable PC were randomized to gemcitabine (1000mg/m2 D1, 8, 15) plus bevacizumab (10mg/kg D1 and 15) and gemcitabine plus placebo (with a dosing schedule identical to the bevacizumab arm). The CALGB Data Safety Monitoring Board released study data in June 2006 because a futility boundary had been crossed. The study was unblinded on June 26, 2006. Preliminary results were presented at the Gastrointestinal Symposium in January 2007. The conclusion of this study was that the addition of bevacizumab to gemcitabine did not improve survival in MPC.32 Of note is that more patients with ECOG performance status of zero were enrolled in the phase II study than in the phase III study, all patients had APC in the phase III study versus APC and LAPC in the phase II study, and 23% had received prior radiotherapy among phase II patients versus 11% in the phase III study. A GEMOX plus bevacizumab combination in a phase II trial including 82 patients with MPC showed six-month survival of 68% (95% CI: 57.1–81.0) and MS of 9.4 months (95% CI: 7.2–11.0).33 The combination of gemcitabine with sorafenib, a small-molecule multikinase inhibitor, was tested in a small phase II trial of patients with MPC.33 Sorafenib was dosed at 400mg twice daily for 28 days along with gemcitabine 1000mg/m2 on days one, eight, and 15 in a 28-day cycle. In this small study of 17 patients, the combination regimen was well tolerated but was inactive. Sorafenib, in addition to inhibiting VEGF, inhibits the raf-1 kinase and platelet-derived growth factor receptor (PDGFR) tyrosine kinase, and may have enhanced activities compared with bevacizumab, which only inhibits VEGF. A larger study has been proposed to investigate its activity. Ras-farnesyltransferase Inhibitors and Matrix Metalloproteinase Inhibitors Ras-farnesyltransferase inhibitors and matrix metalloproteinase inhibitors were shown to be ineffective against MPC as single agents or in combination in various phase III trials. Studies combining targeted agents are being pursued in Europe and the US.34
Conclusions
Although we have made incremental progress in the treatment of PC, the prognosis of patients with this disease remains extremely poor. Gemcitabine plus erlotinib or capecitabine is considered the standard of care for APC patients in North America. In pilot studies of modern combination chemotherapy, responses may exceed those of single-agent gemcitabine, but with added toxicities. However, patients with LAPC seem to derive more benefit from combination chemotherapy than those with APC, and should be studied separately in future studies. The role of XRT in the adjuvant therapy remains split between the US and Europe. We definitely need to identify surrogates for survival. In addition, oncologists need to change their attitude toward clinical trials. The development of novel agents and approaches is urgently needed in conjunction with improvement in access to clinical trials for patients.