Early-stage Pancreatic Cancer
Surgery
For the few patients who present with potentially resectable disease, accurate diagnosis and staging are vital to avoid the unnecessary morbidity associated with aggressive surgical management. Initial radiological staging usually employs contrast-enhanced computed tomography. Endoscopic ultrasound (EUS) in experienced hands is emerging as an important pre-operative assessment tool. EUS allows more accurate characterisation of small lesions, T-staging and definition of vascular structures, and can also be utilised to obtain tissue diagnosis via fine-needle aspirate.5,6 Percutaneous biopsy of resectable lesions is generally not recommended due to the theoretical risk of intra-peritoneal seeding. Positron emission tomography, if available, may provide further information regarding the presence or absence of distant metastases. Staging laparoscopy and laparoscopic ultrasound are also important tools for detecting occult metastases in selected cases.7
A discussion of surgical techniques is beyond the scope of this article. The goals of surgery are removal of the primary tumour with microscopically clear margins, complete resection of the relevant peri-pancreatic lymph node groups and reconstruction of the gastrointestinal tract.8 The standard procedure is a Whipple’s procedure, or pancreatico-duodenectomy, which involves resection of the distal stomach, distal common bile duct, gall bladder, duodenum, pancreatic head, uncinate process, proximal jejunum and regional lymph nodes. A variation on this is the pylorus-preserving Whipple’s, which spares the distal stomach and proximal duodenum. Referral to high-volume surgical centres has improved peri-operative mortality rates to less than 5%.8 Despite this, median survival is still limited to 11–20 months, and the five-year survival rate from surgery alone is less than 25%, mainly due to high rates of local and distal recurrence.9 Both adjuvant chemoradiation (CRT) and chemotherapy have been evaluated as potential strategies to improve surgical outcome. Results of these trials are summarised in Tables 1 and 2. Adjuvant Chemoradiation
The first randomised controlled trial (RCT) to demonstrate a benefit for adjuvant therapy was the Gastrointestinal Tumour Study Group (GITSG) trial. Bolus 5-fluorouracil (5-FU) plus split-course radiation followed by two years of 5-FU was compared with observation alone.10 The study closed early due to poor accrual, after recruiting only 43 patients. Despite this, due to a statistically significant improvement in survival (21 versus 11 months; p=0.035), adjuvant CRT was adopted as standard therapy in the US. This approach has not been incorporated into routine practice in Europe for a number of reasons. First, in the GITSG trial patients received maintenance 5-FU in addition to CRT, and it is therefore impossible to determine which component of treatment was responsible for the observed effect. Second, two subsequent larger European studies, the European Organisation of Research and Treatment of Cancer (EORTC) and European Study Group for Pancreatic Cancer (ESPAC)-1 trials, failed to find a statistically significant advantage favouring adjuvant CRT. The first of the European trials, the EORTC trial, recruited over 200 patients and evaluated post-operative CRT with continuous-infusion 5-FU on days one to five every four weeks and split-course radiotherapy (RT) compared with surgery alone.11 A non-significant trend towards improved survival was seen (24.5 versus 19 months; p=0.208). ESPAC-1 had a two-by-two factorial design to compare CRT (bolus 5-FU with split-course RT) with no CRT and chemotherapy (bolus 5-FU/leucovorin) with no chemotherapy. In contrast to the GITSG trial, in the analysis of CRT versus observation ESPAC-1 found a trend towards worse survival with the addition of CRT (15.9 versus 17.9 months, hazard ratio [HR] for death 1.28, 95% confidence interval [CI] 0.99–1.66; p=0.05).12 A recent meta-analysis did not find a significant effect on risk of death with adjuvant CRT, and a subgroup analysis favoured adjuvant CRT in patients with positive resection margins, although the confidence intervals crossed unity.13
The definitive role of CRT as adjuvant treatment for pancreatic cancer remains uncertain. The ESPAC-1, GITSG and EORTC studies administered CRT that is probably inferior to modern regimens, which now utilise infused 5-FU and single-course radiation. Prospective RCTs comparing modern CRT regimens with non-radiation-containing regimens have not been conducted. Furthermore, whether gemcitabine and/or other systemic agents will succeed 5-FU in chemoradiation regimens also remains to be seen.
Adjuvant Chemotherapy
Several studies (see Table 2) have evaluated the roles of single-agent and combination adjuvant chemotherapy, the largest of which are ESPAC-1, Charité Onkologie (CONKO)-001 and the Radiation Therapy Oncology Group (RTOG)-9704 trial. ESPAC-1 reported a statistically significant overall survival (OS) advantage for adjuvant bolus 5-FU/ leucovorin (21.1 versus 15.5 months, HR death 0.71, 95% CI 0.55–0.92; p=0.009).12 This treatment regimen subsequently became the control arm in the ESPAC-3 trial, which evaluated the efficacy of adjuvant gemcitabine and completed accrual for pancreatic cancer in December 2006; results have not yet been presented. CONKO-001 randomised 368 patients to six months of adjuvant gemcitabine or surgery alone, with a primary end-point of disease-free survival (DFS). This end-point was met, with a median DFS of 13.3 months for patients receiving gemcitabine compared with 6.9 months for patients in the observation arm (p<0.001).14 AT ASCO 2008, final OS data were presented. Adjuvant gemcitabine resulted in a statistically significant benefit compared with observation (22.8 versus 20.2 months; p=0.005).15 A trial reported by Kosuge et al. at the European Society for Medical Oncology (ESMO) 2007 conference provides further support for the use of adjuvant gemcitabine. One hundred and eighteen patients were assigned to three months of adjuvant gemcitabine compared with observation. A significant improvement in DFS (11.44 versus 4.97 months; p=0.01) but not OS (22.3 versus 18.4 months; p=0.29) was seen.16
The standard approach in the US of incorporating CRT into postoperative management is reflected in the design of the RTOG 9704 trial. This study compared gemcitabine with infused 5-FU when given both pre- and post-CRT (infused 5-FU and single-course radiation).17 Four hundred and fifty-one eligible patients were recruited, 388 with pancreatic head tumours. There was no significant difference in OS or DFS for all patients. For patients with pancreatic head tumours, a nonsignificant trend towards improved survival from 16.9 to 20.5 months (p=0.09) was noted with the use of gemcitabine. A 2005 meta-analysis of adjuvant therapy for pancreatic cancer reported a 25% reduction in the risk of death with the addition of adjuvant chemotherapy (HR 0.75, 95% CI 0.64–0.90; p=0.001).13 This improvement was maintained with the inclusion of the CONKO-001 data (24% reduction in the risk of death).13,18 Adjuvant chemotherapy with 5-FU or gemcitabine confers significant improvements in DFS and/or OS. The results of ESPAC-3 are awaited to determine the best agent to use in this setting. Locally Advanced Pancreatic Cancer
Large phase III RCTs that specifically evaluate treatment in locally advanced disease are scarce. It follows that the optimal approach to the management of patients with locally advanced pancreatic cancer remains contentious. Therapeutic options include chemoradiation, chemotherapy and combined chemoradiation/chemotherapy with the goals of both local and distal disease control. Neoadjuvant therapy to downstage and convert initially unresectable locally advanced tumours to resectable remains an experimental approach. Early trials demonstrated that 5-FU-based CRT was superior to RT alone.19,20 The benefits of this approach were confirmed in a 2007 meta-analysis of combined radiation/combined modality therapy for locally advanced pancreatic cancer, which found a survival advantage for chemoradiation compared with radiation alone.21 Over time, CRT regimens have evolved, with infused 5-FU now replacing bolus 5-FU and subsequently, by extrapolating from other malignancies, the substitution of oral capecitabine for infused 5-FU. RCTs comparing infused 5-FU with capecitabine in this setting have not been conducted. Alongside refinement of radiation techniques, other CRT strategies under evaluation are gemcitabine- and paclitaxel-based regimens and combination chemotherapy–radiation regimens.22
An RCT conducted by Chauffert et al. compared gemcitabine chemotherapy with cisplatin–5-FU-based chemoradiation followed by maintenance gemcitabine chemotherapy. This trial was stopped prematurely after a significant OS advantage was found for upfront gemcitabine compared with combined modality therapy (13.8 versus 8.6 months; p=0.03).23 It has been postulated that the toxicity from the CRT led to decreased use of maintenance gemcitabine.
The 2007 meta-analysis mentioned previously did not find a survival advantage for chemoradiation followed by chemotherapy.21 This approach is therefore not recommended as standard therapy. A newer approach currently under evaluation is the administration of initial chemotherapy followed by CRT in the absence of disease progression. Retrospective studies suggest that initial chemotherapy followed by CRT may improve survival.24,25 The theoretical advantage of such an approach is the selection of patients with chemo-responsive disease and without occult micrometastases for CRT to improve local control rates. Ongoing phase III clinical trials are evaluating this approach. The majority of trials evaluating chemotherapy for advanced pancreatic cancer included patients with locally advanced disease. The benefits of chemotherapy have been confirmed in several trials and, for this reason, chemotherapy alone is an accepted treatment option for this group of patients.
Metastatic Pancreatic Cancer
The majority of patients with pancreatic cancer present with advanced (inoperable or metastatic) disease. The outcome for these patients is extremely poor: if untreated, median survival is in the order of three to four months. The aims of treatment are tumour control, symptom management and maintaining and improving quality of life (QOL). Although palliative stenting, bypass surgery, radiotherapy, nerve plexus blocks and intrathecal infusions are often utilised to provide symptomatic relief, chemotherapy is the backbone of treatment for patients with advanced disease of adequate performance status (PS). Several trials have confirmed the benefits of palliative chemotherapy in addition to best supportive care (BSC). In a 2007 meta-analysis, chemotherapy resulted in a 36% improvement in survival compared with BSC (HR 0.64, 95% CI 0.42–0.98).26
Single-agent Chemotherapy
A single RCT published in 1997 comparing gemcitabine (1,000mg/m2 over 30 minutes weekly x 7 followed by one week’s rest, and then weekly x 3 every 4 weeks) with 5-FU (600mg/m2 weekly) established gemcitabine monotherapy as the accepted standard of care for advanced pancreatic cancer. A modest but significant improvement in median survival was observed (5.65 versus 4.41 months; p=0.0025) alongside, and perhaps more importantly, a significant superior clinical benefit response (23.8 versus 4.8%; p=0.0022).27 No single chemotherapy agent has replaced gemcitabine in first-line treatment of advanced pancreatic cancer.
Fixed-dose regimens (FDRs) of gemcitabine have been investigated in an attempt to improve the efficacy of gemcitabine. FDRs capitalise on the pharmacokinetic properties of gemcitabine. Gemcitabine requires initial phosphorylation by deoxycytidine kinase to gemcitabine monophosphate, and subsequent phosphorylation to gemcitabine diphosphate and gemcitabine triphosphate, the active form of the drug.28 Deoxycytidine kinase has saturable kinetics, and it has been demonstrated that infusing gemcitabine at 10mg/m2/minute achieves steady-state plasma levels of 20μmol/l, thereby maximising the rate of formation of gemcitabine triphosphate. Despite initial promising results from phase II studies, the three-arm phase III E6201 study failed to reach its primary end-points of a 33% or more difference in survival using either FDR gemcitabine or FDR gemcitabine with oxaliplatin compared with standard gemcitabine therapy.29
Gemcitabine Combinations
Table 3 summarises the results of phase III studies combining gemcitabine with other chemotherapy agents including fluoropyrimidines (5-FU and capecitabine), platinum agents (oxaliplatin and cisplatin), docetaxel, topoisomerase inhibitors (irinotecan and exatecan) and pemetrexed. Results have been largely disappointing. Although many combinations appeared to improve response rate (RR), few regimens resulted in a significant improvement in OS. The most promising regimens are gemcitabine combined with capecitabine and gemcitabine/platinum combinations. Although gemcitabine combined with cisplatin, epirubicin and 5-FU resulted in statistically significant higher OS compared with gemcitabine alone (5.4 versus 3.3 months), the median OS for each arm was less than the expected median OS for gemcitabine alone.30 This regimen also resulted in significantly higher rates of haematological toxicity.
Two RCTs comparing gemcitabine alone or combined with capecitabine (GemCap) have been conducted in Europe. In the initial analysis of the UK National Cancer Research Institute (NCRI) study, GemCap resulted in statistically significant improvements in RR (14.2 versus 7.1%) and OS (7.4 versus 6.0 months), with a good toxicity profile.31 A subsequent analysis of the UK study, presented at the NCRI Upper Gastrointestinal Clinical Studies Group meeting in May 2008, reported maintenance of the superior RR (19.1 versus 12.4%; p=0.034) and a trend towards improved OS (7.1 versus 6.2 months; p=0.08). The second study evaluating gemcitabine combined with capecitabine did not find a significant difference in OS, RR or PFS between the two arms; however, a post hoc analysis did find a significant prolongation in OS (10.1 versus 7.4 months; p=0.014) for patients with Karnofsky performance status of 90–100.32 Explanations from the authors for the lack of significant difference for all patients were an excess of early disease-related deaths among poor PS patients in the GemCap arm, as well as a smaller sample size and lower capecitabine dose intensity compared with the UK trial. They therefore maintained that gemcitabine combined with capecitabine is an acceptable recommended treatment option for patients of adequate PS. A meta-analysis of these two studies and a third randomised study also evaluating GemCap versus gemcitabine33 (total 935 patients combined) indicated a significant OS advantage for combination chemotherapy (HR 0.86, 95% CI 0.76–0.99; p=0.03) with no significant heterogeneity. At least two meta-analyses have reported a survival benefit for gemcitabine combined with platinum agents.26,34 Gemcitabine combined with oxaliplatin (Gemox), arguably the best tolerated of these regimens, resulted in a statistically significant improvement in RR (26.8 versus 17.3%; p=0.04) and DFS (5.8 versus 3.8 months; p=0.04) compared with gemcitabine alone. In addition, a significant improvement in clinical benefit was reported (38.2 versus 26.9%; p=0.03). Although an OS advantage was not observed, the Gemox regimen represents an active and reasonable treatment option for advanced pancreatic cancer.
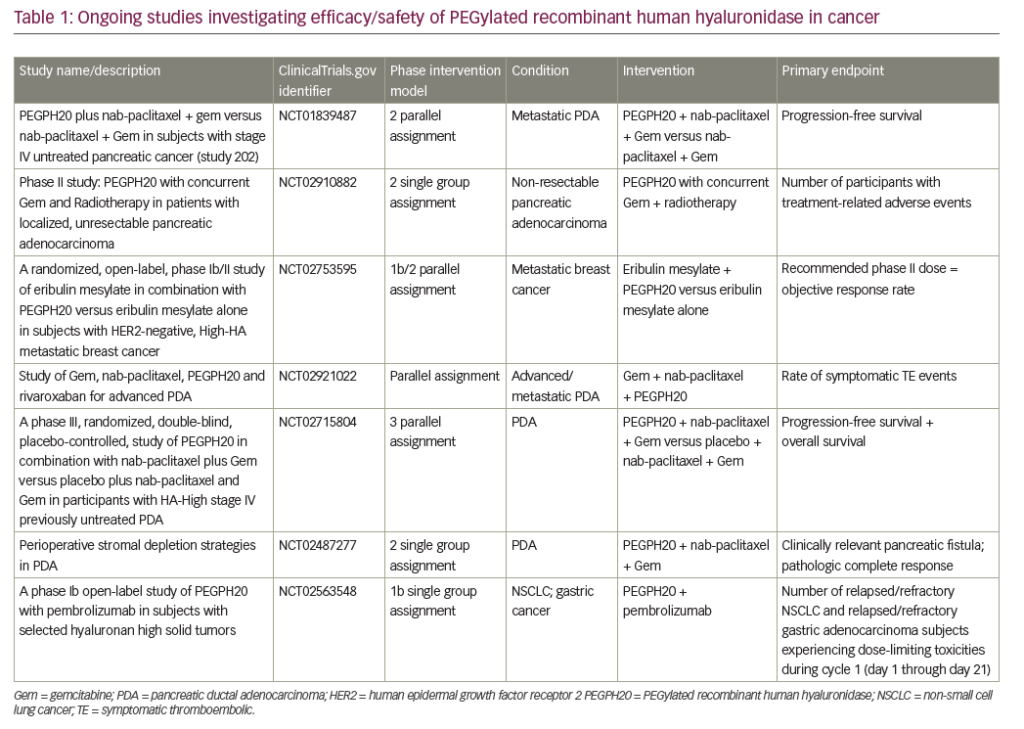
Gemcitabine in combination with molecular targeted agents has also been investigated (see Table 4). Matrix metalloproteinase inhibitors and farnesyl transferase inhibitors did not add to the efficacy of gemcitabine in RCTs.35,36 In the NCIC CTG PA.3 study, erlotinib combined with gemcitabine conferred a modest but significant OS benefit compared with gemcitabine alone (6.24 versus 5.91 months, HR 0.82; p=0.038).37 On the basis of this trial, erlotinib was approved for use in combination with gemcitabine for the treatment of advanced pancreatic cancer.
Preliminary results of two phase III studies presented at the American Society of Clinical Oncology (ASCO) in 2007 comparing gemcitabine with gemcitabine/bevacizumab and gemcitabine/cetuximab have not demonstrated a significant improvement in OS, PFS or RR.38,39 More recently, AVITA, a double-blind, placebo-controlled study of gemcitabine and erlotinib ± bevacizumab, failed to demonstrate an OS benefit (primary end-point) for the addition of bevacizumab (7.1 versus 6.0 months; p=0.21).40 The addition of bevacizumab to gemcitabine and erlotinib resulted in significantly improved PFS (4.6 versus 3.6 months; p=0.0002) and a trend towards improved RR (13.5 versus 8.6%; p=0.057). A current phase II trial in the UK, TARGET, is evaluating the addition of erlotinib and bevacizumab to gemcitabine/capecitabine, whereas a current German controlled trial is comparing the gemcitabine/ erlotinib doublet with capecitabine/erlotinib.
Second-line Therapy
There is no standard second-line treatment for advanced pancreatic cancer, and few randomised phase III studies have been completed. Several regimens have been evaluated including 5-FU/leucovorin, irinotecan, rubitecan, paclitaxel, gemcitabine plus oxaliplatin, oxaliplatin plus fluoropyrimidines, capecitabine plus erlotinib and raltitrexed plus oxaliplatin or irinotecan.
The CONKO-003 study initially compared BSC with oxaliplatin/5-FU/ leucovorin in patients who had failed first-line therapy with gemcitabine. Initial results after recruiting 46 patients reported a significant improvement in median OS for oxaliplatin/5-FU/leucovorin (4.8 versus 2.3 months; p=0.0077). The trial was subsequently amended to incorporate 5-FU/leucovorin as the control arm, as physicians and patients increasingly found BSC to be an unacceptable comparator arm.41 At ASCO 2008, the reported median OS for the oxaliplatin-containing arm was 26 weeks compared with 13 weeks for 5-FU/leucovorin alone.42 Median PFS was also improved (13 versus nine weeks; p=0.012). These data suggest that patients who progress during or after first-line gemcitabine-based chemotherapy may benefit from a second-line oxaliplatin-based regimen.
Conclusion
Although the approach to the adjuvant management of pancreatic cancer differs across the Atlantic, with chemoradiation favoured in the US and chemotherapy alone in Europe, the consensus is that surgery alone is inadequate treatment for early-stage pancreatic adenocarcinoma. A multidisciplinary approach is essential, as is accurate staging and careful selection of patients who are to proceed to resection. The results of ESPAC-3 will provide important information regarding whether gemcitabine surpasses 5-FU as the more efficacious adjuvant chemotherapy agent.
Current data support gemcitabine combined with capecitabine or erlotinib as the standard of care for patients with locally advanced or metastatic disease. Gemcitabine in combination with platinum agents is also an option for patients with good PS. Whether the addition of chemoradiation to initial chemotherapy will improve outcomes for patients with locally advanced pancreatic cancer remains to be seen.
An exciting first-line approach has been the addition of both erlotinib and bevacizumab to gemcitabine/capecitabine chemotherapy, which is currently under investigation in the phase II component of the UK TARGET study. Second-line treatment options remain limited, but recent data suggest a potential role for oxaliplatin-bsed regimens. Active recruitment to clinical trials is clearly vital to establish best treatment, but is difficult, namely due to the rapid decline in PS that usually accompanies this clinical scenario.