Gastric and gastro-oesophageal junction (GOJ) adenocarcinomas are highly aggressive tumours with an overall poor prognosis, which is primarily attributable to the late stage of diagnosis resulting from nonspecific symptoms.1,212 While curative surgical resection is recommended for early-stage cases,3Expand Reference advanced disease is treated with palliative intent, employing chemotherapy, immunotherapy and targeted therapies.4Expand Reference
The backbone of first-line treatment in gastric/GOJ cancer is a combination of platinum and fluoropyrimidine chemotherapeutic agents.4,545 The ToGA trial (ClinicalTrials.gov identifier: NCT01041404), published in 2010, found that the addition of trastuzumab adds a modest survival benefit for patients with human epidermal growth factor receptor 2 (HER2)-positive tumours.6Expand Reference However, despite this advance, nearly a decade passed before the next step forward in the treatment of these cancers.7Expand Reference These new approaches included immunotherapy and targeted agents such as immune checkpoint inhibitors, fibroblast growth factor receptor 2 (FGFR2b) blockers, and antibody–drug conjugates (fam-trastuzumab deruxtecan-nxki [Enhertu®]; Daiichi Sankyo, Inc, Basking Ridge, NJ, USA).8Expand Reference In addtion to these, agents that target Claudin 18.2 (CLDN18.2) are also under intense investigation for treating gastic/GOJ tumors.9Expand Reference
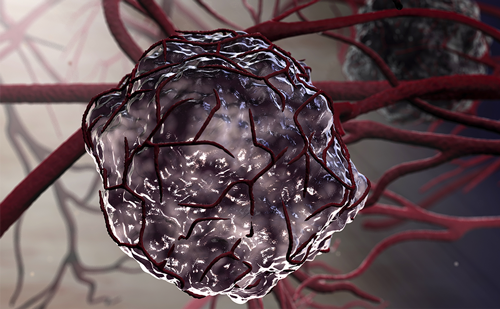
Claudin (CLDN) proteins were first described in 1998 as components of the tight cellular junctions that act as paracellular barriers.10Expand Reference Within the CLDN family, CLDN18 encompasses two isoforms: CLDN18.1, predominantly found in lung tissue, and CLDN18.2, exclusively expressed in gastric tissue.11Expand Reference CLDN18.2 epitopes are inaccessible in normal gastric tight junctions.12Expand Reference However, during malignant transformation, disruptions in cellular polarity expose CLDN18.2 epitopes on the surface of cancer cells, rendering them potentially accessible for targeted therapies.12Expand Reference CLDN18.2 expression is maintained in up to 80% of primary gastric cancers and their metastases and is also aberrantly expressed in other malignancies.13,141314 Sahin et al. detected CLDN18.2-expressing cells in 63% of pancreatic, 60% of oesophageal, 41% of non-small cell lung and 15.38% of ovarian cancers.13Expand Reference
Zolbetuximab (IMAB362; Astellas Pharma, Tokyo, Japan) is a first-in-class chimeric monoclonal antibody targeting CLDN18.2.15Expand Reference It exerts its effect by mediating antibody-dependent cellular cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC), thereby inducing apoptosis in gastric cancer cells expressing CLDN18.2.16Expand Reference It can also enhance T-cell infiltration and induce pro-inflammatory cytokines release when combined with chemotherapeutic agents.17Expand Reference
This review outlines the potential of zolbetuximab as a first-line treatment for CLDN18.2-positive, HER2-negative, locally advanced unresectable or metastatic gastric or GOJ adenocarcinomas. It provides a comprehensive analysis of the available clinical data from phase I, II and III trials on the efficacy and safety of zolbetuximab in the current treatment landscape.
Mechanism of action and preclinical evidence
Targeting Claudin 18.2: an overview of the biomarker
Sahin et al. identified CLDN18.2 in the differentiated cells of the gastric mucosa but not in undifferentiated gastric stem cells.13Expand Reference CLDN18.2 in the tight junctions of gastric mucosa maintains the paracellular barriers and prevents the leakage of H+ ions through paracellular pathways.18Expand Reference The structure of CLDN proteins consists of four transmembrane domains, including a N-terminus and C-terminus in the cytoplasm and two extracellular loops. Potential therapeutic antibodies interact with CLDN proteins in the extracellular loops. The C-terminus is the site of phosphorylation and interaction with signalling molecules.17Expand Reference Alterations in the function of CLDN proteins contribute to tumour development and proliferation.19Expand Reference Sanada et al. detected a reduction in CLDN18.2 expression in 56.5% of gastric cancer cells via quantitative RT-PCR, implying its possible role early in gastric carcinogenesis.20Expand Reference Hagen et al. demonstrated, via an in vivo genetic approach, that the loss of CLDN18.2 protein resulted in alterations of the gastric mucosal architecture in mice.21Expand Reference Consequently, this loss promoted evolving neoplasia in mice, highlighting the tumour-suppressive role of CLDN18.2 in gastric tissue.21Expand Reference Sahin et al. reported that the expression of CLDN18.2 in cancer cells is regulated by the cyclic-AMP response element binding protein binding to the CLDN18.2 promoter site.13Expand Reference Furthermore, genetic alterations involving CLDN18.2 were observed in subgroups of gastric cancer. Notably, CLDN18–ARHGAP26 gene fusion was detected predominantly in diffuse gastric cancer.22Expand Reference ARHGAP encodes for Rho GTPase-activating protein (RhoGAP), which contributes to the organization and stability of actin and microtubule cytoskeleton.23Expand Reference Therefore, CLDN18–ARHGAP26 gene fusion in gastric cancer cells led to the loss of their epithelial phenotype, increased invasiveness, compromised cellular barrier, and decreased cell–cell and cell–extracellular matrix adhesion.24Expand Reference
Understanding the precise mechanisms through which CLDN18.2 influences mucosal homeostasis and carcinogenesis could provide valuable insights for developing novel therapeutic strategies. Thus far, most zolbetuximab studies have used immunohistochemistry (CLAUDETECT™ 18.2VR kit; Ganymed Pharmaceuticals, Mainz, Germany) to evaluate CLDN18.2 expression in gastric cancer cells.25–27252627 Nonetheless, since 92% of the protein sequence of CLDN18.1 is highly consistent with CLDN18.2, looking for more precise antibodies targeting CLDN18.2 is an on-going challenge.28Expand Reference A novel approach to identifying CLDN18.2 involves using a CLDN18.2 molecular beacon with a stem-loop hairpin configuration. The molecular beacon recognized CLDN18.2 RNA rapidly in several cell models and was also successfully used in a circulating tumour cell assay.29Expand Reference
Zolbetuximab: binding and inhibiting Claudin 18.2
Zolbetuximab is a novel chimeric immunoglobulin G1 antibody produced from murine monoclonal antibodies and chimerized to resemble the human immunoglobulin G1 constant region for clinical application.17Expand Reference This monoclonal antibody exhibits high sensitivity and specificity for the CLDN18.2 protein expressed on the surface of malignant cells, particularly at the first extracellular loop of CLDN18.2. Upon binding to CLDN18.2, zolbetuximab triggers the cellular and humoral immune systems to activate ADCC and CDC.30Expand Reference Its safety and ability to eliminate cancer cells were reported in preclinical animal models.25Expand Reference Subsequent clinical trials have focused on evaluating the safety, optimal dosing and efficacy of zolbetuximab among patients with gastric and GOJ cancer.27,31–3327313233
Preclinical studies demonstrating the efficacy and mechanism of action of zolbetuximab
In preclinical studies, the binding characteristics and potential antitumour activity of zolbetuximab were assessed both in vitro using CLDN18.2-expressing gastric cancer cell lines and in vivo in mouse CLDN18.2-expressing xenograft models of human gastric cancer cell-derived tumours30Expand Reference and pancreatic cancer cell lines.16Expand Reference CLDN18.2 was found to be expressed robustly (60–90%) in pancreatic cancer and primary and metastatic gastric cancer tumours.16,301630 Zolbetuximab mediated ADCC and CDC against gastric cancer lines with endogenous CLDN18.2 expression but not in CLDN18.2-negative cancer cells.30Expand Reference Chemotherapeutic agents increased CLDN18.2 expression in tumour cell lines, thus further sensitizing them to zolbetuximab-induced toxicity.30,343034
Clinical trials and efficacy
Phase I trials: safety and dosing considerations
In a phase I trial (ClinicalTrials.gov identifier: NCT00909025), 15 patients each received a single infusion from one of five dose groups (33, 100, 300, 600 and 1,000 mg/m2) of zolbetuximab.14Expand Reference This demonstrated a linear pharmacokinetic profile with a half-life (t1/2) of 17 days. No life-threatening adverse events (AEs) were reported with single doses up to 1,000 mg/m2.15Expand Reference One patient who received 600 mg/m2 maintained stable disease at the 4-week follow-up.15Expand Reference Given the small sample size, no definitive conclusions could be drawn regarding the potential association between CLDN18.2 expression level and the activity of zolbetuximab. The enrolled patients had variable CLDN18.2 expression, and the anti-tumor activity of zolbetuximab was not the primary objective of this phase I trial.
Another phase I trial conducted in Japan evaluated patients with CLDN18.2-positive, previously treated locally advanced or metastatic gastric/GOJ cancer, with disease progression on previous lines of therapy (ClinicalTrials.gov identifier: NCT00909025).35Expand Reference Patients received 800 mg/m2 intravenous zolbetuximab on cycle 1, day 1, followed by 600 mg/m2 or 1,000 mg/m2 every 3 weeks. Similarly to the previous phase I study, this trial did not identify any dose-limiting toxicities. The best overall response was stable disease (SD) in 64.7% or progressive disease (PD) in 35.3%, yet, only two patients had SD lasting more than six months. The median progression-free survival (PFS) and overall survival (OS) were 2.6 and 4.4 months, respectively.
A third phase I trial assessed the safety of combining zolbetuximab with immunomodulating drugs such as zoledronic acid and interleukin-2 in patients with advanced or metastatic gastric cancer or GOJ cancer (ClinicalTrials.gov identifier: NCT01671774).36Expand Reference The rationale behind exploring this combination stemmed from the previous understanding of zolbetuximab-mediated ADCC30Expand Reference; namely, this mechanism involves interacting with immune effector cells such as natural killer cells and gamma/delta (γδ) T cells, which only constitute a small proportion of T cells. The bisphosphonate zoledronic acid is recognized for activating cytolytic γ9δ2 T cells and natural killer cells, potentially enhancing the ADCC effect.37Expand Reference Yet, although this combination therapy was generally well tolerated, it did not show additional improvements compared with zolbetuximab alone. The best response observed in this trial was stable disease, which was achieved in 58% of the patients.36Expand Reference
Phase II trials: assessing zolbetuximab’s efficacy and response rates
In a multicentre, phase IIa clinical trial named the MONO study (ClinicalTrials.gov identifier: NCT01197885),31Expand Reference the efficacy of zolbetuximab was evaluated as a single agent for patients with advanced gastric, GOJ, or oesophageal adenocarcinoma with moderate-to-strong CLDN18.2 expression in ≥50% of cancer cells. Patients received zolbetuximab every 2 weeks at two dose levels (300 mg/m2 as a safety run-in and 600 mg/m2 as the targeted dose). Clinical benefit was achieved in 23% (n=10) of patients, with four attaining partial response and six maintaining stable disease.
Another randomized, multicentre phase IIb clinical trial (ClinicalTrials.gov identifier: NCT01630083), named the FAST study, assessed the efficacy of zolbetuximab plus epirubicin, oxaliplatin, and capecitabine (EOX) versus EOX alone as first-line treatment for patients with advanced gastric/GOJ and oesophageal adenocarcinoma with moderate-to-strong CLDN18.2 expression in ≥40% tumour cells.27Expand Reference Compared with those receiving EOX alone, patients treated with zolbetuximab plus EOX had a longer median PFS (7.5 versus 5.3 months), a statistically significant reduction in the risk of death (hazard ratio [HR] 0.55; p<0.0005) and a prolonged median OS (13 versus 8.3 months). Of note, the improvement in PFS and OS with combination therapy was more pronounced in patients with ≥70% CLDN18.2-expressing tumours than in the overall population with a ≥40% CLDN18.2 expression. This finding is consistent with the MONO study,31Expand Reference where 9 of the 10 patients who achieved clinical benefit had moderate-to-strong CLDN18.2 expression in ≥70% of tumour cells, which could indicate a potential link between the expression of CLDN18.2 and zolbetuximab activity.
A further multicohort phase II trial (the ILUSTRO study; ClinicalTrials.gov identifier: NCT03505320) investigating zolbetuximab as monotherapy and combined with modified FOLFOX6 (mFOLFOX6), with or without nivolumab, or pembrolizumab, is ongoing.38,393839 However, results presented from ILUSTRO cohort 2, in which patients received zolbetuximab plus mFOLFOX6, revealed a median PFS of 13.7 months (95% Confidence Interval [CI]: 7.4–not estimable), a 12-month PFS rate of 58% and an objective response in 63.2% of patients (95% CI: 38.4–83.7).40Expand Reference
Phase III trials: comparative studies and outcomes
The phase III studies SPOTLIGHT (ClinicalTrials.gov identifier: NCT03504397)33Expand Reference and GLOW (ClinicalTrials.gov identifier: NCT03653507)32Expand Reference were conducted as potential registration trials to determine the benefit of adding zolbetuximab to chemotherapy (mFOLFOX6 or capecitabine and oxaliplatin [CAPOX]) in previously untreated patients with recurrent/metastatic HER-2-negative, CLDN18.2-positive (moderate-to-strong CLDN18.2 expression in ≥75% of tumour cells) gastric or GOJ adenocarcinomas. In the SPOTLIGHT trial, 565 patients from 215 centres were enrolled and randomly assigned (1:1) to either zolbetuximab plus mFOLFOX6 or placebo plus mFOLFOX6. Zolbetuximab 800 mg/m2 was administered on cycle 1, day 1, followed by 600 mg/m2 on cycle 1, day 22, and every 3 weeks in the following cycles.33Expand Reference Conversely, mFOLFOX6 was administered on days 1, 15 and 29 for four 42-day cycles. Zolbetuximab treatment resulted in a significant 25% reduction in the risk of disease progression (HR 0.75, 95% CI 0.60–0.94; p=0.0066) and a prolonged median PFS of 10.61 months (95% CI 8.90–12·48) compared with 8.67 months in the placebo group (95% CI 8.21–10.28). Additionally, the median OS was significantly longer in the zolbetuximab group than in the placebo group (median 18.23 versus 15.54 months; HR 0.75, 95% CI 0.60–0.94; p=0.0053). The objective response rate (ORR) was similar in both treatment arms (61% and 62%) among patients with a measurable disease.25,272527 Intriguingly, subgroup analysis revealed that patients with the diffuse and intestinal Lauren subtypes experienced significantly longer PFS and OS in the zolbetuximab group. Meanwhile, no additional survival benefits were observed amid patients with mixed and other Lauren subtypes.33Expand Reference Additionally, patients with GOJ cancer experienced lower benefits of zolbetuximab compared with gastric cancer patients. Yet, a cautious interpretation of these findings is warranted due to the small GOJ cancer subgroup, and future trials should recruit more patients with GOJ cancer to withdraw conclusions precisely.
The survival benefit is less pronounced in the SPOTLIGHT trial compared with the phase II FAST trial; this difference may be attributed to the variations in the median survival among patients in the control arm that deviate from the expected outcome.27,332733 In the FAST trial, the median survival in the EOX arm was lower than reported in the REAL-2 (Current Controlled Trials identifier: ISRCTN51678883)41Expand Reference and REAL-3 (ClinicalTrials.gov identifier: NCT00824785)42Expand Reference trials (median OS 8.3 versus 11.2 and 11.3 months, respectively).27Expand Reference The authors of the FAST trial attributed this difference to the higher proportion of patients with metastatic disease in the FAST trial compared with the REAL-2 trial (95.2% versus 75.2%). Conversely, in the SPOTLIGHT trial, the expected median PFS was longer than anticipated in the control arm, which might have contributed to the reduced difference in outcome and the delayed separation of the survival curves of both treatment arms.33Expand Reference
The phase III trial, GLOW, aimed to assess the efficacy and safety of zolbetuximab combined with CAPOX chemotherapy versus CAPOX with placebo.32Expand Reference Patients received an 800 mg/m2 loading dose of zolbetuximab on cycle 1, day 1, followed by 600 mg/m2 every 3 weeks. CAPOX consisted of oxaliplatin 130 mg/m2 administered intravenously on day 1 and oral capecitabine 1,000 mg/m2 administered twice daily on days 1–14 of each cycle for eight 21-day cycles. Zolbetuximab plus CAPOX showed a statistically significant improvement in PFS, achieving the primary endpoint of this trial.43Expand Reference Compared with the placebo group, patients in the zolbetuximab arm achieved a 31.3% risk reduction in disease progression or death (HR 0.687, 95% CI 0.544–0.866; p=0.0007).43Expand Reference Compared with the placebo group, the zolbetuximab group exhibited significant improvements in median PFS (8.21 versus 6.80 months; HR 0.687; p=0.0007) and OS (14.39 versus 12.16 months; HR 0.771, p=0.0118).43Expand Reference In patients with measurable disease, the ORR was 53.8% in the zolbetuximab versus 48.8% in the placebo arm.43Expand Reference
These two large phase III trials that evaluated zolbetuximab in combination with two widely accepted standard-of-care chemotherapy regimens for gastric and GOJ adenocarcinomas demonstrated an OS benefit and have been submitted to regulatory agencies. However, there are a few differences between them. In the SPOTLIGHT trial, zolbetuximab was administered every 3 weeks in combination with mFOLFOX6, which was given every 2 weeks. On the other hand, the GLOW trial used a 3-week treatment interval for both zolbetuximab and CAPOX. This difference in the frequency of clinic visits may be considered when evaluating the convenience and feasibility of treatment options. Notably, the GLOW trial exhibited an earlier separation of the survival curves than the SPOTLIGHT trial, indicating a potentially more favourable outcome for the CAPOX plus zolbetuximab treatment regimen. Further studies may be warranted to validate this finding and compare these chemotherapy regimens to determine the best combination with zolbetuximab.
Safety profile and adverse events
Common adverse events associated with zolbetuximab
Zolbetuximab was shown to have a manageable safety profile both alone and when combined with CAPOX and mFOLFOX6.33Expand Reference The most frequently reported AEs were gastrointestinal, namely nausea and vomiting, potentially due to specific CLDN18.2 expression in the gastric mucosa. In the phase I trials, zolbetuximab was well tolerated across the entire dose range (33–1,000 mg/m2), and treatment-related AEs mostly were of grades 1–3.15,35,36153536 A similar safety profile was observed in the phase II MONO and FAST trials.27,312731 In the MONO study, the most common AEs were nausea, vomiting and fatigue, and 20% of patients (n=11) discontinued treatment due to treatment-emergent AEs (TEAEs).31Expand Reference In the FAST study, nausea occurred in 76.2% and 81.8% of patients in the EOX and EOX plus zolbetuximab arms, respectively.27Expand Reference Vomiting was also more frequent in the EOX plus zolbetuximab arm than in the EOX arm (67.5% versus 54.8%). Notably, vomiting was less common among patients who had a prior gastrectomy than patients without gastrectomy in the EOX plus zolbetuximab arm but not in the EOX arm.27Expand Reference Anaemia and neutropenia were more common in the EOX plus zolbetuximab treatment arm than in the EOX arm.27Expand Reference Cytopenias are commonly associated with chemotherapy, and the increased AE monitoring time resulting from the significant improvement in survival could have contributed to this increase in frequency in the EOX plus zolbetuximab arm.
Consistent with the previous trials, nausea, vomiting and decreased appetite were the most frequent TEAEs in the SPOTLIGHT trial.33Expand Reference A higher incidence of grade 3 or more TEAEs was reported in the zolbetuximab arm, with 87% of the 279 patients experiencing such events, compared with 78% of the 278 patients in the placebo arm.33Expand Reference Furthermore, treatment was discontinued due to treatment-related AEs in 14% of patients in the zolbetuximab arm, compared with 2% of patients in the placebo arm.33Expand Reference
Strategies for managing adverse events
Given the high symptom burden and complexity often seen in patients with advanced gastric or GOJ adenocarcinoma, achieving a balance between the antitumour activity and quality of life poses a significant challenge.44Expand Reference In the FAST trial, the addition of zolbetuximab has shown promising results in improving patient-reported outcomes and significantly reducing the time to deterioration (p=0.008) compared with EOX alone.45Expand Reference Patient-reported outcomes were assessed via the EORTC QLQ-C30 and QLQ-STO22 tools. Patients who received zolbetuximab maintained a better quality of life and lower symptom burden for a longer duration, as the time to deterioration in the QLQ-C30 global health status/quality of life score was significantly delayed by 2.6 months in the EOX plus zolbetuximab arm compared with EOX alone.45Expand Reference In the MONO and SPOTLIGHT trials, nausea and vomiting occurred more frequently during the first infusion.31,333133 With repeated zolbetuximab infusions, the incidence tended to decrease. Various modalities were employed to reduce gastric toxicity, including infusion time lengthening, antiemetics administration and infusion interruptions.31,33,35313335 In the FAST trial, patients received proton pump inhibitors for gastric mucosal protection.27Expand Reference In addition, premedication with antiemetics was recommended for the first 3 days of each cycle. To avoid possibly compromising zolbetuximab’s effect, using steroids as antiemetics was contraindicated.27Expand Reference Future research might be needed to focus on the long-term outcomes and safety considerations associated with zolbetuximab.
Current treatment landscape and zolbetuximab’s positioning
CLDN18.2 expression and patient populations
These described trials selected patients with moderate-to-strong CLDN18.2 expression; however, expression thresholds differ between the trials. For instance, the phase III trials enrolled patients with moderate-to-severe CLDN18.2 expression in ≥75% of tumour cells,32,333233 while the phase II trials included patients with a CLDN18.2 expression in ≥40% and ≥50% of tumour cells, respectively.27,312731 Despite this difference, subgroup analyses in the phase II trials FAST and MONO revealed that patients with high CLDN18.2 expression achieved improved efficacy.27,312731 CLDN18.2-positive tumours were detected in 38% (n=922) of patients in the SPOTLIGHT trial,33Expand Reference 49% (n=334) in the FAST trial27Expand Reference and 45% (n=54) in the MONO trial.31Expand Reference Notably, the CLDN18.2 immunostaining assay was switched from a manual immunohistochemistry test (the CLAUDETECT 18.2VR kit) in phase II trials to the investigational VENTANA® CLDN18 (43-14A) RxDx Assay (Roche Diagnostic Solutions, Tucson, AZ, USA) in the SPOTLIGHT phase III trial.33Expand Reference Previous studies reported a higher CLDN18.2 expression among Japanese patients than among European populations (87% versus 77%).14,261426 Future research should focus on determining a standardized detection method with high specificity, determining the optimal cut-off point for expression levels and investigating whether different ethnicities may require different cut-off points to refine patient selection criteria and optimize zolbetuximab use in clinical practice.
Pellino et al. assessed the association of CLDN18.2 positivity with other biomarkers and the clinicopathological features of gastric/GOJ cancers.46Expand Reference Their investigation revealed no association between CLDN18.2 expression and p53, HER2, E-cadherin, programmed death-1 ligand 1 (PD-L1) or mismatch repair deficiency status.46Expand Reference Notably, high expression of CLDN18.2 was detected in Epstein-Barr Virus (EBV)-positive gastric cancers, considering the small Epstein-Barr Virus-positive sample. Moreover, CLDN18.2 expression exhibited a statistically significant association with specific clinical characteristics, including patients aged below 70 years, an advanced disease stage (III or IV) at diagnosis, peritoneal involvement and a lower frequency of liver metastasis.46Expand Reference These findings originated from a single institution, emphasizing the need for further investigation on a larger scale through prospective, multicentre studies to validate these associations comprehensively. In the SPOTLIGHT trial, 13% (n=41) of the patients with CLDN18.2-positive cancers had a PD-L1 combined positive score (CPS) of 5 or above.33Expand Reference This finding suggests a potential advantage for combining zolbetuximab and PD-L1 inhibitors in patients with PD-L1-positive, CLDN18.2-positive gastric/GOJ cancer , which is currently under evaluation in the on-going ILUSTRO phase II trial.38 FExpand Referenceurthermore, it represents a significant focus for future studies for ascertaining the most effective targeted therapy for individuals with CLDN18.2-positive cancers and a PD-L1 CPS of 5 or higher.
Zolbetuximab’s positioning and future perspectives
Based on these clinical trial results,9,32,3393233 the US Food and Drug Administration (FDA) has granted a Priority Review designation to the Biologics License Application for the approval of zolbetuximab and set a target action date of 12 January 2024.47Expand Reference If approved, zolbetuximab would become the first CLDN18.2-targeted therapy available in the United States for this patient population.
The promising results of zolbetuximab for patients with CLDN18.2-positive gastric/GOJ cancer have prompted exploring its potential as a targeted therapy for other CLDN18.2 expressing malignancies, such as pancreatic adenocarcinoma. An on-going phase II clinical trial aims to assess the efficacy and safety of zolbetuximab in combination with nab-paclitaxel and gemcitabine as first-line treatment in patients with CLDN18.2-positive, metastatic pancreatic adenocarcinoma.48Expand Reference This trial represents a pivotal step in assessing the broader therapeutic potential of zolbetuximab and its synergy with existing treatments for other malignancies with CLDN18.2 expression. In addition, exploring zolbetuximab in combination with other agents that have shown potential in enhancing ADCC, such as immune checkpoint inhibitors or immune-modulating therapies, could hold considerable promise.
In the context of CLDN18.2-targeted therapies, it is noteworthy that zolbetuximab does not stand alone as a potential treatment option. Several innovative CLDN18.2-targeting therapeutic agents are currently under investigation. For example, antibody–drug conjugates, such as CMG901 (ClinicalTrials.gov identifier: NCT04805307) and SYSA1801 (ClinicalTrials.gov identifier: NCT05009966),49,504950 and bispecific T-cell engagers, such as AMG 910 (ClinicalTrials.gov identifier: NCT04260191),51Expand Reference have emerged as promising strategies. Moreover, a single-arm, open-label phase I pilot study revealed that autologous CAR-CLDN18.2 T-cell therapy is both safe and exhibits promising therapeutic efficacy in patients with advanced gastric and pancreatic adenocarcinoma, with a total ORR of 33.3% and well-tolerated AEs, highlighting its potential as a treatment option (ClinicalTrials.gov identifier: NCT03159819).52Expand Reference These novel interventions aim to capitalize on the specificity of CLDN18.2 targeting, holding great promise for improved therapeutic outcomes in patients with CLDN18.2-positive malignancies.
With the aggressiveness and poor prognosis of gastric/GOJ cancer, we are excited about zolbetuximab being a potentially transformative drug in the treatment landscape of CLDN18.2-positive tumours, especially given the promising results observed in the SPOTLIGHT and GLOW phase III trials. We believe that if zolbetuximab is granted FDA approval, it will not only provide hope to patients facing gastric/GOJ cancer but also serve as a cornerstone for future research into targeted therapies for CLDN18.2-positive cancers. However, patients who exhibit both CLDN18.2 positivity and high PD-L1 CPS present a therapeutic challenge. The question arises about whether these patients should be treated with zolbetuximab alone, immune checkpoint inhibitors or a combination approach. This dilemma underscores the complexity of precision medicine in gastro-oesophageal cancer and offers scope for future trials to determine the optimal treatment for this subset of patients. We believe that a new era of precision medicine represents a bright future for patients with gastric/GOJ cancer.
Conclusion
Zolbetuximab has demonstrated promising efficacy and a manageable safety profile among patients with advanced CLDN18.2-positive gastric and GOJ adenocarcinoma. With the current Priority Review for FDA approval, zolbetuximab may soon become the first CLDN18.2-targeted therapy available in the United States, providing hope for better outcomes in this challenging disease.