The treatment of advanced or recurrent endometrial cancer has advanced significantly in recent years. This is particularly important, given the rising mortality rates of endometrial cancer, particularly among high-risk subtypes.1Expand Reference Platinum-based chemotherapy had long been the standard of care in patients with advanced or recurrent endometrial cancer. New approaches to the classification of endometrial cancer based on the molecular profile have allowed for a more targeted approach to treatment. The new molecular classification identifies ultramutated (harbouring a DNA polymerase epsilon or POLE mutation) and hypermutated (mismatch repair–deficient [dMMR]) tumours, which tend to have an improved prognosis and better response to immunotherapy than other endometrial cancers. Microsatellite-stable (copy-number low) tumours tend to be of low grade with intermediate prognosis, while P53-mutated (copy-number high) tumours have a poorer prognosis and higher rates of recurrence.2,323
The use of immune checkpoint inhibitors, such as dostarlimab, pembrolizumab, durvalumab and atezolizumab, has been studied in patients with endometrial cancer across the molecular classification spectrum and has shown significant promise in dMMR tumours and limited efficacy in microsatellite-stable tumours. These new therapies are leading to the approval by the US Food and Drug Administration (FDA) and National Comprehensive Cancer Network-listed treatments for patients with endometrial cancer. For example, dostarlimab is now approved by the FDA for dMMR endometrial cancer as both a single agent for the second line or greater and in conjunction with platinum-based chemotherapy as the first line in newly diagnosed advanced-stage or recurrent chemotherapy-naive settings.4Expand Reference
Mechanism of action
Dostarlimab is an immunoglobulin G4 (IgG4) monoclonal antibody that acts on the T-cell programmed cell death protein 1 (PD-1) pathway. The PD-1 pathway includes the PD-1 T-cell receptor and the programmed death ligands 1 and 2 (PD-L1 and PD-L2), which bind to it. The upregulation of the PD-1 pathway leads to T-cell immunosuppression and is a mechanism of action used by multiple cancers. Dostarlimab binds to PD-1, inactivating this pathway.5Expand Reference Thus, the tumour is unable to hide from the immune system. Similar to other PD-1 inhibitors, such as nivolumab and pembrolizumab, dostarlimab binds primarily to the flexible loop regions of the PD-1 receptor. The bulk of the resulting structure is what limits the binding of the ligands PD-L1 and PD-L2 to the receptor, as the flexible loop regions are not directly involved in the binding of the PD-1 receptor to its ligands. Dostarlimab also binds to PD-1 with a high affinity, greater than that of PD-L1.6Expand Reference The proof-of-concept for the action of immune checkpoint inhibitors, such as PD-1 inhibitors, against endometrial cancer was related to the fact that microsatellite instability-high (MSI-H) tumours, such as around 40% of endometrial cancers, have a high mutational burden. Tumours that exhibit significant inhibition of DNA repair mechanisms are particularly susceptible to the immune checkpoint inhibitors because excessive mutations make the tumours more visible to the immune system.7,878 Pharmacokinetic and pharmacodynamic data from the GARNET (A Phase 1 Dose Escalation and Cohort Expansion Study of TSR-042, an Anti-PD-1 Monoclonal Antibody, in Patients With Advanced Solid Tumors; ClincalTrials.gov identifier: NCT02715284) phase I clinical trial results support the use of fixed dosing instead of weight-adjusted dosing, which is in line with the prior approved PD-1 inhibitors.9,10910
Clinical efficacy
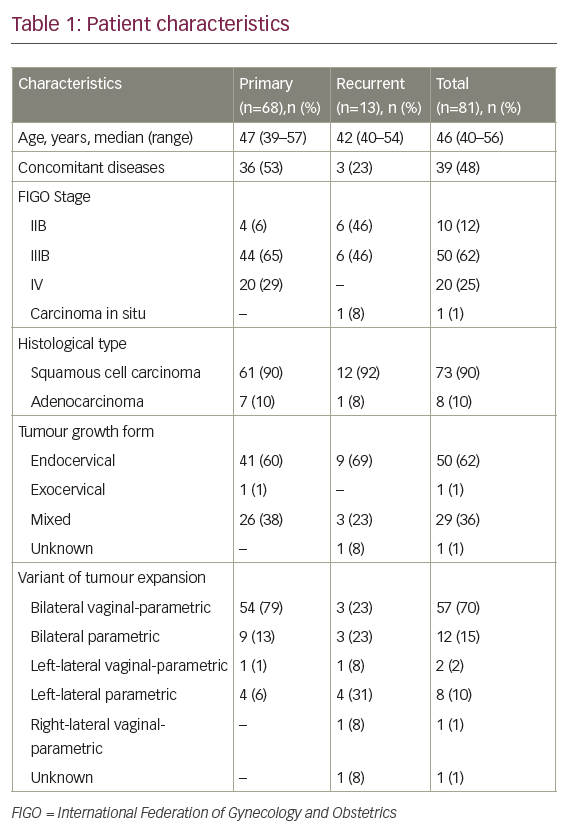
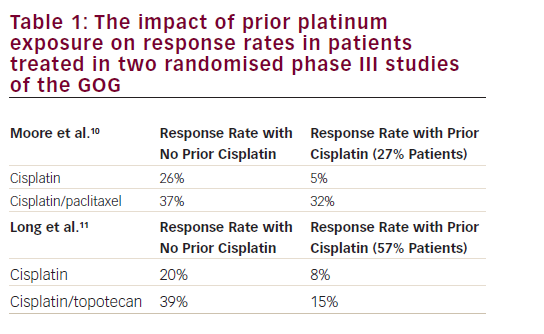
After Le et al. described in their 2017 article titled “Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade,” that PD-1 blockade had a 53% objective response rate in tumours exhibiting mismatch repair deficiency, further trials were published demonstrating the specific efficacy of dostarlimab in endometrial cancer.8Expand Reference The GARNET trial, whose results were published by Oaknin et al., was a phase I clinical trial evaluating dostarlimab activity in patients with dMMR and mismatch repair–proficient (pMMR) recurrent or advanced endometrial cancer, which has progressed after platinum chemotherapy. Parts 1 and 2A of the trial were mainly focused on dosing strategies and safety profiles, but part 2B split patients into different cohorts, including A1 (those with dMMR endometrial cancer) and A2 (those with pMMR endometrial cancer). These patients received fixed-dose dostarlimab intravenously 500 mg every 3 weeks for four cycles, followed by 1,000 mg every 6 weeks until progression, discontinuation secondary to toxicity or withdrawal from the clinical trial. Interim results from 104 patients with dMMR demonstrated an objective response rate of 42.3%.11Expand Reference In a post-hoc analysis, although not powered for statistical significance, this benefit was preserved across different histologic subtypes of endometrial cancer, stages and lines of prior therapy.9Expand Reference Based on these interim results, in April 2021, the FDA granted approval for dostarlimab as a single agent for advanced or recurrent dMMR endometrial cancer, which has progressed after standard-of-care platinum-based chemotherapy.7Expand Reference As of the latest publication, this single-group trial has enrolled 129 patients with dMMR and 161 patients with pMMR endometrial cancer. The most recent interim endometrial cancer results demonstrated a 43.5% objective response rate for patients with dMMR and a 14.1% objective response rate for patients with pMMR.12Expand Reference In March 2022, a different PD-1 inhibitor, pembrolizumab, was approved by the FDA for the same indication as dostarlimab after the results of the phase II trial KEYNOTE-158 (A Clinical Trial of Pembrolizumab [MK-3475] Evaluating Predictive Biomarkers in Subjects With Advanced Solid Tumors; ClinicalTrials.gov identifier: NCT02628067) demonstrated an overall response rate of 46% for dMMR/MSI-H recurrent endometrial cancer.13Expand Reference
Subsequently, a phase III double-blind randomized controlled trial (A Study to Evaluate Dostarlimab Plus Carboplatin-paclitaxel Versus Placebo Plus Carboplatin-paclitaxel in Participants With Recurrent or Primary Advanced Endometrial Cancer [RUBY]; ClinicalTrials.gov identifier: NCT03981796) was conducted to evaluate dostarlimab in conjunction with standard chemotherapy (carboplatin [area under the curve -6] and paclitaxel [175 mg/m2]) for advanced-stage or recurrent endometrial cancer.14Expand Reference Eligible patients had biopsy-proven stage III or IV or first-recurrence endometrial cancer. Multiple histologic cell types were accepted, including carcinosarcoma, clear cell, serous and mixed. Patients could only have received systemic therapy in the adjuvant or neoadjuvant setting greater than 6 months prior to recurrence. Patients did not have to have measurable disease if they were stage III patients with periaortic node metastasis or any stage IV patients. Patients were randomized to receive carboplatin, paclitaxel and dostarlimab (500 mg) every 3 weeks for six cycles followed by dostarlimab (1,000 mg) every 6 weeks for up to 3 years or to receive the same regimen with a placebo instead of dostarlimab. The primary endpoints were progression-free survival (PFS) and overall survival (OS), and the data were analysed among the dMMR/MSI-H population and the overall population. The trial randomized 494 patients, with 24% being dMMR. The results published by Mirza et al. were remarkable. Overall, patients who received dostarlimab had a 2-year PFS of 36.1% and OS of 71.3%. Patients who received the placebo had a 2-year PFS of 18.1% and OS of 56%. Patients with dMMR who received dostarlimab had a 2-year PFS of 61.4% and OS of 83.3%. Patients with dMMR who received the placebo had a 2-year PFS of 15.7% and OS of 58.7%.14Expand Reference After the results of the RUBY trial were released, the FDA granted approval in July 2023 to the RUBY trial regimen for dMMR or MSI-H endometrial cancer.2Expand Reference
Safety and tolerability
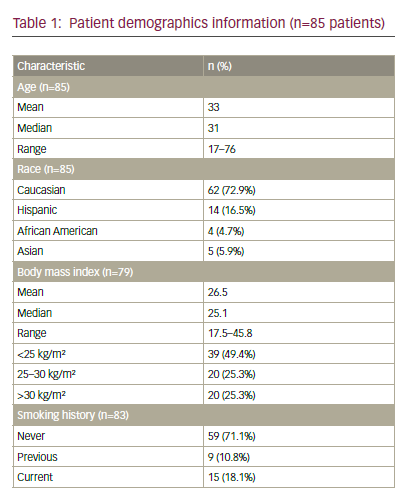
Both the GARNET trial and the RUBY trial demonstrated that dostarlimab has a similar safety profile to other approved immune checkpoint inhibitors. The GARNET trial reported that most treatment-related adverse events (TRAEs) were grade 1 or 2 and were commonly fatigue, diarrhoea and nausea. Among TRAEs that were grade 3 or greater, individual incidence was <3%, with anaemia being most common followed by diarrhoea, fatigue and some laboratory abnormalities in liver enzymes. Overall, 5.5% of enrolled patients had to discontinue trial participation secondary to grade 3 or greater TRAEs, most commonly because of laboratory abnormalities. Of note, all participants of the GARNET trial were on single-agent dostarlimab.12Expand Reference Adverse events reported in the RUBY trial must be interpreted differently than the GARNET trial, as all participants were receiving chemotherapy (carboplatin and paclitaxel) and some participants were receiving dostarlimab, while others received a placebo. Overall, adverse events and serious adverse events were more common in the dostarlimab treatment group than in the placebo group (70.5 and 37.8% versus 59.8 and 27.6%, respectively). The most common adverse events were nausea, alopecia and fatigue with similar incidence between the treatment group and the placebo group, although nausea and alopecia were higher in the dostarlimab group. The greatest difference in incidence between the two groups occurred for rashes, which occurred in 22.8% of patients on dostarlimab and 13.8% of patients on placebo. Immune-associated adverse events were more common in the dostarlimab group, including hypothyroidism, rash and arthralgia. There were two deaths in the dostarlimab group judged to be related to treatment: one due to myelosuppression and one due to hypovolaemic shock. There were no deaths associated with adverse events in the placebo group.14Expand Reference Patient-reported outcomes were evaluated in 88 of the GARNET trial participants, and the results were published by Kristeleit et al. The assessment was performed using the European Organization for Research and Treatment of Cancer Quality of Life Questionnaires C30 with favourable results through cycle 7 of treatment. Overall quality of life improved for participants over their baseline prior to starting treatment with dostarlimab. While physical functioning reportedly dropped below baseline after the first few cycles, it ultimately returned to baseline prior to cycle 7. There was no change in cognitive functioning with treatment. Regarding symptoms, pain, nausea and vomiting improved after a few cycles of treatment.15Expand Reference
Clinical implications
The results of the RUBY trial were first presented at the Society of Gynecologic Oncology Annual Meeting in March 2023, with the publication by Mirza et al. released shortly after online ahead of print.14Expand Reference While dostarlimab had already been approved for use in dMMR endometrial cancer as a single agent in the second or greater line of treatment, the RUBY trial led to the approval of dostarlimab for the treatment of dMMR endometrial cancer in conjunction with standard-of-care chemotherapy in the first-line setting. This approval occurred less than 6 months after the RUBY trial results were released. Currently, dostarlimab is the only immune checkpoint inhibitor approved by the FDA for this use. A similarly positive trial, NRG-GY018 (ClinicalTrials.gov identifier: NCT03914612) evaluating the PD-1 inhibitor pembrolizumab in conjunction with standard-of-care chemotherapy for advanced or recurrent endometrial cancer, was published simultaneously with the RUBY trial.16Expand Reference However, there remains a gap in treatment approval for pMMR endometrial cancer. While the most significant benefit was seen for patients with dMMR in the RUBY trial, there was an improvement in PFS and OS for all-comers, of which 76% did not have dMMR endometrial cancer.14Expand Reference However, dostarlimab for the treatment of pMMR endometrial cancer has yet to be approved by the FDA.