Cavitary bone defects are created in the curettage or debridement of benign bone tumors, infections, or low-grade malignancies. In order for new bone to fill these defects, the material that resides within must be osteoconductive, or an appropriate scaffolding that prevents non-osseous (fibrous) tissue infiltration, supports the attachment of new osteoblasts and osteoprogenitor cells, and sustains an interconnected structure through which new cells can migrate and new vessels can form.1 The subsequent substance that develops through this osteoconductive step must also be osteoinductive (facilitate the travel of factors and materials for cellular differentiation) and osteogenic (cause the cellular production of new bone) for new bone to form.1 Current US consensus dictates that in order for this cascade to develop in a bone defect, a graft must be used. In fact, over 500,000 bone graft procedures are performed annually in the US.2 In order to meet the first and crucial step of osteoconductivity, the graft must fill the void and provide a scaffolding on which stem cells can attach; in order to facilitate the next two critical steps, the graft must be non-inflammatory and non-toxic and resorb at a rate roughly equal to that of bone formation.1,3
Grafts that have been used to meet the aforementioned steps include autograft, allograft, and synthetic substitutes. Bone grafts constitute a large economic market, with over $1.5 billion in sales in 2007 in the US alone.2 Autograft has long been the gold standard of bone grafts and is the only graft option that has osteoconductive, osteoinductive, and osteogenic properties.2,4 Autologous bone grafting carries the disadvantages of pain at the donor site, variable quality, limited quantity, increased hospital stay, and a 15.8–29.2% complication rate. Complications include, but are not limited to, lateral femoral cutaneous or cluneal nerve injury, superior gluteal artery injury, wound problems, infection, need for further surgery, pelvic fracture, hematoma, and gait disturbances.4–8 Allogenic bone graft is the most commonly used bone graft material. It has osteoconductive and osteoinductive properties and no donor site morbidity, and is relatively low-cost. Allografts have the disadvantages of limited supply, potential antigenic response, lack of uniformity, and potential disease transmission—the most concerning being the documented instances of HIV and hepatitis C virus (HCV) transmission with fresh-frozen tendon and bone allografts.4,5,9–12 No consensus on the actual rate of disease transmission with bone allograft exists, though one study estimates the ‘viral transmission risk’ associated with bone allografting to be one in 1.6 million;13 there have, however, been no documented instances of HIV or HCV transmission through irradiated bone.14In response to the disadvantages of autograft and allograft, synthetic bone graft substitutes have evolved. Four classes of synthetic bone graft substitute exist:
- allograft-based—allograft bone used in combination with other bone substances: demineralized bone matrix (DBM);
- factor-based—natural/recombinant growth factors of bones: transforming growth factor beta (TGF-β), platelet-derived growth factor (PDGF), fibroblast growth factor, and bone morphogenetic protein (BMP);
- polymer-based—degradable and non-degradable polymers of bone: polylactic acid and polyglycolic acid; and
- ceramic-based: calcium sulfate, calcium phosphate, and bioglass.
The ceramic-based class accounts for over 60% of the synthetic market, a vast majority of which consists of mineral-based ceramics, which are the focus of this article. The purpose of this article is to review the published literature on the use of mineral bone graft substitutes in the grafting of bone defects created in the treatment of benign bone tumors in order to describe their risks, benefits, differences, and outcomes individually and in comparison with each other.
Materials and Methods
A complete Medline search was conducted for all articles describing mineral bone graft substitutes in the treatment of surgically created cavitary bone defects, specifically looking for recent high-level comparative studies but also including review and instructional articles. All of these studies were subsequently further cross-referenced among their citations to retrieve all relevant literature. Relevant pre-clinical studies on the use of mineral bone graft substitutes were also included. Studies involving bone grafting of spinal fusion, trauma, sports, and joint reconstruction procedures were generally excluded, with the exception of high-level or comparative studies that may apply to the treatment of surgically created cavitary bone defects.
General Review of Mineral-based Ceramics
Ceramic bone graft substitutes have been shown to be osteoconductive, virtually unlimited in supply, uniform in quality, without donor site morbidity, and without risk of disease transmission.15–18 The downsides of ceramics include their brittleness, low tensile strength, potential antigenic reactions, lack of osteoinductive and osteogenic properties, high cost (up to $400/cc, resulting in $150million in costs each year in the US), variable resorption rates, and potential for interference with wound healing.2,4,5,15,16
Indications for the use of a mineral bone graft substitute include a surgically or traumatically created bone defect that requires grafting for optimal consolidation. Relative contraindications include active infection, high infection risk, open fracture, lack of soft-tissue coverage, and bovine sensitivity (when collagen composite products are used). Numerous in vitro and in vivo studies have demonstrated the osteoconductivity of mineral bone graft substitutes.4,5,15,16 The pore size of the synthetic bone graft that allows for optimal scaffolding provision, osteoconductivity, and subsequent bone ingrowth and resorption is 150–500μ, which falls into the range of most synthetic mineral grafts available.4 The most notable clinical difference between different mineral bone graft substitute compounds is their varying rates of resorption: smaller particulate grafts are resorbed by osteoclasts and more expediently, while larger particulate grafts are resorbed by foreign body giant cells in a much slower manner.17 The different mineral bone graft compounds have very different biochemical characteristics; therefore, the detailed biology and clinical results of each class are described individually.Calcium Sulfates
The original mineral bone graft substitute, calcium sulfate (CaSO4), dates back to 1892 in its use as a bone graft for cavitary defects.19 The compound is derived by adding water to calcium sulfate hemihydrate. This creates gypsum, which is subsequently heated, leading to its crystallization as calcium sulfate.5,20 In literature from the distant past, Peltier and others state that calcium sulfate is biocompatible, bioabsorbable, radio-opaque, safe, non-immunogenic, non-osteoinhibitive, and regular in its resorption, and there is no infection from sequestration. These early studies also indicate, however, that calcium sulfate needs bone or periosteum for new bone to be incorporated.3
Calcium sulfate creates an acidic environment in vivo (calcium phosphate and sulfuric acid) that may be toxic to bacteria. For this reason, it has long been used as a treatment for osteomyelitis, with or without an associated antibiotic.21,22 In the earliest series involving humans, Peltier and Jones reviewed 26 unicameral bone cysts (UBCs) treated with curettage followed by packing with calcium sulfate pellets (plaster of Paris). They noted uneventful healing in all except for two patients (7.7%), who developed serous drainage that required revision surgery.21 In more recent years, significant data regarding calcium sulfate has come from animal studies. Calcium sulfate has been shown to adhere to osteoblasts and osteoclasts in vitro and to be resorbed by osteoclasts in rats.23 At 12 weeks, a study of sheep femur defects found BMP-2, BMP-7, TGF-β, and PDGF staining to be highest in the femurs grafted with calcium sulfate plus autograft, followed by calcium sulfate alone, followed by autograft, followed by nothing at all.24 In a canine model, the paper’s authors demonstrated that calcium sulfate appeared to be completely resorbed and replaced by bone at 13 weeks, with no adverse inflammatory response.25 The same authors also described a series of four different canine models in a single article.26 In their canine spine-fusion model, calcium sulfate had a significantly smaller area of bone fusion mass compared with autograft alone and was similar to no graft at all. After implantation of 10% tobramycin-impregnated calcium sulfate, local concentrations of antibiotic dropped to undetectable levels by 28 days, systemic concentrations were undetectable within 24 hours in a dose-dependant manner, and there was no local or systemic toxicity. Calcium sulfate resorbed completely and was shown to be osteoconductive in the canine humerus. Calcium sulfate with DBM had significantly more new bone formation at six weeks compared with calcium sulfate alone.26,27 Another canine bilateral defect model was used to compare a stronger calcium sulfate (MIIG X-3) versus conventional calcium sulfate pellets (Osteoset), and found a three-fold increase in initial compressive strength in MIIG group.28
Many of the clinical studies using calcium sulfate in the treatment of bone defects are retrospective in nature and many come from the trauma literature (see Table 1). In a review of 26 patients with a non-union (19) or osseous defect (nine) after open fracture treated with calcium sulfate and iliac crest bone grafting, seven out of nine (77%) bone defects had healed at five months.29 Re-visiting the application of calcium sulfate as an antibiotic carrier, another group retrospectively studied 25 long bone infections (nine defects and 16 non-unions), in which a calcium sulfate bone graft was used as an antibiotic vehicle, with or without adjuvant autograft. It was noted that 23 (92%) of the cases eradicated the infection and eight (32%) patients developed a sterile draining sinus that resolved when the graft was resorbed.30 The average time to resorption was 2.7 months, all nine bone defects obtained more than 60% new bone ingrowth (on X-ray), and five out of seven (71%) non-unions treated with calcium sulfate alone healed. A study reviewing 17 open fractures sustained from high-energy mechanisms in a combat situation found at an average of 8.5 months that 12 of 17 fractures were consolidated at radiographic follow-up. Six required further surgery for infection, four ultimately needed amputation, and there were three cases of heterotopic ossification (HO) at the graft site that all required resection.31
A number of studies regarding calcium sulfate in the grafting of cavitary bone defects created during the surgical treatment of benign bone tumors have been performed. A review of 13 non-structural bone defects in the treatment of benign bone tumors looked at radiographic time to resorption and complications. It found that all lesions healed and all pellets were resorbed at an average of 13.4 weeks (range five to 24 weeks). The resorption was proportional to the size of the lesion and occurred from the periphery inward.32 Another study retrospectively looked at patients with various benign bone lesions grafted with Osteoset, with or without DBM. At 12 months it found that 76–100% had healed, mean Musculoskeletal Tumor Society (MSTS) scores were 98% of normal, and one out of 24 patients (4.2%) sustained a post-operative pathologic fracture.33 The same authors in an improved version of the same study with greater numbers (98) and longer follow-up (mean 32 months) noted 100% resorption with bone formation by six months in all cases and a 3.1% post-operative pathologic fracture rate.34 In another study, the authors looked specifically at benign bone tumors curettaged and then grafted with an injectable form of calcium sulfate (MIIG 115) in a liquid vehicle. Fourteen out of 15 (93.3%) of the grafted defects showed complete radiographic incorporation of the graft material at an average of eight weeks. There was one (0.7%) deep infection and one (0.7%) pathologic femoral neck fracture.35 A retrospective review of 28 children with UBCs in different sites treated with a percutaneous aspiration, curettage, and Osteoset pellet injection grafting technique resulted in two (7.1%) persistent cysts, one of which required further surgery.36 In a continuation of this study, the authors retrospectively reviewed 27 more (55 total) pediatric UBCs. They found that 11 required at least one more surgery for recurrence, with two of 55 (3.6%) developing superficial drainage that was successfully treated with oral antibiotics alone and three of 55 (5.5%) sustaining post-operative fracture.37 Other studies have noted some downsides to calcium sulfate as a bone graft. One series of 15 cases of Osteoset pellet grafting following benign bone tumor resection revealed three cases of severe inflammatory reaction, one of which resolved two months post-operatively. One reaction resulted in wound dehiscence and one required surgical graft debridement. These results caused the authors to conclude that “due to rapid graft resorption, the resulting calcium-rich fluid incites inflammation.”38 One review of 58 Osteoset-grafting cases in the treatment of benign bone tumors noted a 13.8–19.0% rate of ‘adverse reaction’ to the graft, which consisted of erythema, edema, and serous drainage.39 In a subsequent article, the same journal published a series of 22 children with UBCs treated with aspiration and injection of liquid calcium sulfate (MIIG 115) or liquid calcium sulfate plus calcium phosphate hybrid (Prodense).40 They noted three cases of laryngospasm immediately after injection (all treated with MIIG), two of which required intubation and all of which resolved without further complication. They also noted one case of temporary systemic venous thrombosis (SVT) immediately after injection with Prodense, which resolved without complications.
Of all studies regarding the use of calcium sulfate in benign bone defects, only two high-level clinical studies (level I/II) have been performed.41 Kelly et al. conducted a level II prospective, multicenter cohort study of Osteoset pellets in 109 patients requiring a morcelized bone graft for a non-structural bone defect from multiple conditions in multiple locations (including a 46-patient subgroup of benign bone tumors). Of these, 65% had adjuvant graft (DBM, bone marrow aspirate, cancellous allograft, or cancellous autograft).42 Looking at calcium sulfate alone, there was 99% resorption and 98% new bone formation at 12 months. In the bone tumor subset treated with Osteoset alone (10 patients), there was 100% graft resorption and 97% new bone formation at 12 months. There was a 12% complication rate, including three infections (2.8%), two pathologic fractures (1.8%), and four cases of serous drainage that resolved once the pellets were absorbed (3.6%). An elegant level 1 prospective randomized, double-blind, controlled study compared calcium sulfate versus no grafting at all in tibial bone defects created after bone–patellar-tendon–bone harvest for knee ligament surgery. The authors studied the amount of new bone formation with serial computed tomography (CT) scans at 0, 6, 12, and 24 weeks.43 Significantly increased new bone was found in both groups from zero to six weeks and significantly increased bone was observed in the control group alone from six to 12 weeks compared with Osteoset (p=0.01). However, no statistical difference was found between the two groups at any time interval.
Calcium Phosphates
Hydroxyapatite
In response to the rapid absorption and inflammation associated with calcium sulfate, calcium phosphate compounds with potentially improved biological and mechanical properties gained popularity. In the calcium phosphate family, hydroxyapatite (HA: Ca10(PO4)6(OH)2) is derived from the sea corals Porites and Goniopora. It is created by a hydrothermal exchange that converts calcium carbonate in the coral exoskeleton to crystalline HA.4,20 Its 200–500μ pore size is similar to human trabecular bone and it is available in blocks, granules, or cement formulations. HA has compressive strength but remains brittle, with low tensile strength.15,44
Several pre-clinical studies have evaluated the initial safety and efficacy of HA as a bone void filler. In their implantation of 52 canine bone defects from various sites with HA, the authors of one study found the construct to be weak initially, but to be almost as strong as native bone upon incorporation.45 Another canine model found the HA graft site to consist of 52% soft tissue, 13% new bone, and 35% HA at 12 months, with 67% of the HA surface being covered with new bone.46 In a canine humeral defect model, at 16 weeks 50–60% of pores were filled with new bone and compressive strength was two to three times that of the surrounding cancellous bone; however, the grafted area only reached cortical bone strength, and the bending strength of the associated cortical bone returned to only 10% of its normal value.47 Shors and Holmes looked at 37 biopsy specimens of HA implants taken a mean 14 months post-grafting through light microscopy and electron scanning microscopy. They found 30% soft tissue, 31% HA, and 38% new bone, with 56% of the implant surfaces being covered by bone.48All of the clinical studies using HA grafting in the treatment of bone tumors are retrospective in nature (see Table 2). One study looked at 23 patients in whom simple bone cysts were treated by curettage followed by HA cube packing. It found complete healing without cyst recurrence in 78% of cases at two years, with new bone surrounding the HA at an average of 2.3 months.49 Two Indian studies of bovine HA studied grafting after benign bone tumor treatment in a small number of cases (12 and 23) and followed them clinically and radiographically for up to six years. The authors found the graft material to be biocompatible, safe, and slow to remodel, with no adverse effects or graft-related complications.50,51 Uchida et al. reported on 60 cases in which HA bone graft was used to fill resected benign bone tumors. Patients were followed up for a mean of 36 months.52 The authors biopsied seven specimens (cases requiring surgery for other reasons) and found new bone ingrowth onto the graft in all cases. They did, however, experience three (5%) pathologic fractures and saw minimal radiographic resorption in all cases, even at five years. Another study looked retrospectively at 51 patients with benign bone tumors excised and filled with pure HA. At a mean follow-up of 11.4 years the HA was resorbed statistically more rapidly in males and young patients (<30 years of age), but was not fully resorbed in any patient at the last follow up. Patients had no graft-related or neoplastic complications, but two (3.9%) had post-operative fractures within two months of surgery.53 In order to improve delayed resorption, alterations in the production of traditional HA were made by preventing the complete conversion of calcium carbonate to HA. A retrospective review of 71 consecutive patients managed with advanced coralline HA (Pro Osteon 500R) in the treatment of bone tumors and followed up for an average of 2.4 years revealed lack of resorption of the graft material and a 16.9% complication rate.54
As with calcium sulfate, the highest-level studies involving the use of HA in bone defects come from the trauma literature (see Table 3). In 1989, Bucholz et al. in a prospective, randomized study compared operative tibial plateau fractures treated with HA (Pro Osteon) grafting against those treated with iliac crest cancellous autograft.55 They followed autograft patients for 15.4 months and HA patients for 34.5 months and were unable to find any statistical differences in maintenance of reduction, union rates, or complications. In seven HA cases requiring further surgery, biopsy was performed and revealed 25–47% new bone ingrowth and 25–39% residual HA. They also found a lack of radiographic HA resorption in all cases at follow-up. Another prospective, randomized, multicenter study looked at HA cement (BoneSource) compared with iliac crest bone graft in the treatment of traumatic metaphyseal defects throughout the skeleton. The authors found that maintenance of reduction and ‘success’ increased in the HA group compared with the iliac crest bone graft group at six (69 versus 57%) and 12 months (79 versus 70%), as did maintenance of reduction (83 versus 67%), but these differences did not achieve statistical significance.56
Tricalcium Phosphates
In response to the delayed resorption profiles of HA, the tricalcium phosphate (TCP: Ca3(PO4)2) group evolved. This group is also in the calcium phosphate family, which includes alpha, beta, and gamma subtypes. Alpha-TCP (α-TCP) is polygonal in structure while β-TCP is spherical, more porous, and more trabeculated, and resorbs faster than α-TCP.57 β-TCP is the most commonly used of the three forms, has increased porosity (50% [250–400μ diameter]) and resorbs 10–20 times faster than HA.58–61 Granules and blocks of β-TCP have similar compressive strength to cancellous bone, but like HA are brittle and have low tensile strength.58 TCP resorbs in six to 18 months via osteoclasts without inflammatory reaction. 62
In 1984, Uchida et al. conducted a histologic study of three different porous ceramic mineral bone graft substitutes (calcium aluminate, calcium phosphate, and HA). They found all three to have tissue ingrowth, but there was a considerably lower density of ingrowth in the calcium aluminate group.63 In a canine study of 1cm tibial defect treated with grafting and external fixation, a combination TCP (36% alpha and 64% beta; Cellplex) showed statistically increased torsional strength and stiffness compared with autograft, allograft, and no graft at six weeks but not at eight weeks. There was complete histologic bone ingrowth, with 38% residual implant, at eight weeks.64In a study of 40 patients with bone defects (including eight benign bone tumors), the authors found excellent results with the use of β-TCP; however, this may last a variable number of years without being resorbed.65 Another study of 18 pediatric bone cysts treated with TCP also found two recurrences, with the remaining 16 patients having well-incorporated grafts with no adverse reaction. They did, however, find residual TCP up to seven years post-operatively.66 A further group of authors studied 24 patients treated with HA (20) or β-TCP (four) in a non-randomized fashion for the grafting of cavitary defects from different benign bone tumors. They did not compare the two substances head to head, but concluded that both grafts were safe and efficacious in the treatment of benign bone tumors.67 A retrospective review of 20 defects (20cc average size) treated with β-TCP found that 16 went on to full resorption and remodeling (four at 12 months, eight at 24 months, and four at 48 months), with three grafts in larger defects (41.2cc average size) never fully resorbing. The only complication was a rash.68 A review of 53 patients with cavitary bone defects created during the curettage of benign bone tumors followed for a mean of 21 months found no complications. Forty-three percent of cases were fully resorbed at the latest follow-up. The rates of resorption in these cases were statistically proportional to the size of the defect.69 Other investigators have found that the size and volume of the defect and graft, as well as the patient’s age and bone quality, are important factors affecting the integration of β-TCP into host bone.70 In a level III retrospective study comparing HA (Bonfil) with β-TCP (OSferion) in 53 patients with benign bone tumors, both groups had two pathologic fractures (7.6% overall). The authors found β-TCP to be a more attractive bone graft substitute since it showed evidence of graft resorption and new bone formation in all cases. One patient with subchondral giant cell tumor treated with HA graft sustained varus deformity requiring surgical revision.71
While most TCP ceramics are made through a high-pressure sintering technique with compaction, new proprietary formation techniques have been developed that may make these implants more biochemically favorable.4 One such proprietary technique of β-TCP machining creates an ultraporous β-TCP (Vitoss) that has been the subject of several studies. Vitoss consists of 75% 100–1,000μ pores for bone ingrowth and 25% smaller (<100μ) pores, theoretically aiding in diffusion.4,44 In a review of six cases where Vitoss was used in human fractures, no adverse reactions were seen. One case of biopsy nine months post-operatively showed new bone formation, no inflammatory reaction, and ‘significant quantities of the graft remaining.72 In a retrospective radiographic case series, 60 patients with cavitary bone defects were treated with Vitoss.
Bone marrow aspirate and resorption were determined on X-ray.73 The authors noted that resorption and trabeculation increased steadily with time. One out of 60 cases (1.7%) had a pathologic fracture. There was no difference in graft incorporation rate based on age, size of defect, or use of local adjuvant treatment. Another retrospective review of 24 patients with cavitary lesions created after curettage of a benign bone tumor filled with Vitoss found faster resorption and statistically faster trabeculation for smaller lesions (<43cc) at all time intervals of three, six, nine, and 12 months, with trabeculation lagging behind resorption.74 None of the lesions was fully resorbed at 18-month follow-up. The graft in soft tissues was seen in most patients at six weeks, all of which eventually resorbed. Two patients (8.3%) had extrusion of the graft from the incision that resolved. Another two patients (8.3%) sustained post-operative fracture. Hak describes another proprietary process of β-TCP (x-link, TrueForm, FormPutty) formation that has been developed in which the β-TCP is laid down one layer at a time, creating 3D geometry that also allows for increased scaffolding, implantation of cells and factors, and bone ingrowth.5 In an interesting canine humerus defect model, FormPutty, Vitoss, autograft, and no graft at all were compared head to head histopathologically and mechanically.75 Both FormPutty and Vitoss had statistically increased tissue reaction scores at 12 weeks compared with autograft and no-graft sites. There was also a statistically increased reaction at 12 weeks with FormPutty and Vitoss compared with their six-week marks. Both TCPs had a statistically decreased residual graft at 12 weeks compared with six weeks. There were no significant differences found between any of the groups in terms of new bone formation, residual implant, yield force, stiffness, or failure force at 12 and 24 weeks. In a level II prospective study of 18 ankle fusions treated with x-link granules, the authors noted an 85% fusion rate at a mean of four months, with no graft complications.76Calcium Phosphate Cements
Neither HA nor TCP has greater compressive strength than cancellous bone and cannot be used in situations where greater strength is required. Studies using high-level investigations have analyzed the use of calcium phosphate cement in the treatment of fractures that require structural support. Although these studies involve traumatic and not true cavitary bone defects, their high level and potential applicability to tumor surgery warrants their mention. A modification of traditional TCPs, these injectable compounds consist of combinations of calcium phosphate, TCP, and calcium carbonate, which upon mixture and exothermic or isothermic crystallization reaction change from a temporary liquid into solid dahilite or carbonated apatite. This is similar to the mineral phase of bone, with greater compressive strength than cancellous bone.4,5 These substances set in less than 10 minutes and achieve maximal compressive strength at 24 hours. One study showed that its calcium phosphate cement had an initial set time of 2.75 minutes, a final set time of 7.5 minutes at 37ºC, and a final compressive strength of 48MPa at 24 hours (the maximum compression strength of cancellous bone is 30MPa).77 A study of the calcium phosphate cement Norian SRS showed a final compressive strength of 55MPa at 24 hours.78 This graft and surrounding bone remodels over time. It is absorbed by osteoclasts, results in new lamellar bone formation, and resorbs slowly, with 30–60% resorbed at one year.79 Most of the calcium phosphate cements cure in an isothermic manner; however, some may be slightly exothermic (e.g. Mimix), albeit not enough to cause the thermal tissue damage seen with polymethylmethacrylate.79 A human cadaveric lateral tibial plateau fracture model comparing cancellous grafting with α-BSM calcium phosphate bone cement found statistically increased stiffness and resistance to displacement (p<0.0001) in the α-BSM group.80
Progressing from these pre-clinical studies, numerous level I studies have prospectively looked at calcium phosphate cement (Norian and α-BSM) in the supportive treatment of metaphyseal fractures (see Table 3). These studies have found statistically improved early motion in distal radius fractures,81,82 earlier weight-bearing and mobilization in lower extremity fractures,83–86 improved maintenance of reduction,87–92 and improved early fracture stability in hip fractures.87,88 Interestingly, after publishing a level I study in favor of Norian SRS in femoral neck fractures, Mattsson et al. in a subsequent study of femoral neck fractures found a statistically increased revision rate in the calcium phosphate cement group and did not recommend its use.85 This being said, the majority of the data highly support the use of calcium phosphate cements for metaphyseal support in peri-articular fractures. No high-level human studies evaluating the use of calcium phosphate cements in the treatment of bone defects from tumor have been performed.
Mineral Bone Graft Composites
In the quest to improve the delivery vehicle of bone graft substitutes in order to avoid problems—including difficult handling, inability to fully fill the void, extravasation into soft tissues, and the desire to obtain further biological advantage—collagen- and silicon-based composites were developed. Modifications of the TCP include the formulation packing, strip, or moldable putty vehicles that usually involve the addition of a matrix substance such as type I bovine collagen (i.e. Vitoss Scaffold Foam). The addition of type I collagen decreases compressive strength and the collagen portions are quickly absorbed.5 These composites cannot be used in patients with allergies to bovine collagen. In a level I prospective, randomized, multicenter study, 297 long-bone fractures from various sites that required surgical stabilization were grafted with 65% HA/35% TCP plus type I bovine collagen (Collagraft) or iliac crest autograft. The authors were unable to find differences in union (88% power) or function between the groups. Twelve patients developed bovine collagen antibodies, but no related problems occurred.93 With regard to silicated mineral compounds, no studies have been performed to evaluate their safety and efficacy in human bone defects. In vitro biochemical studies have produced mixed results, with some claiming improved biological activity with silication by increasing the solubility of the material, creating a more electronegative surface, and developing a finer microstructure.94 A conflicting bench study states that “there is no experimental evidence that Si ions are released from Si-substituted calcium phosphates at therapeutic concentrations, and there is no study linking the improved biological performance of Si-substituted calcium phosphates to Si release.”95 In an elegant animal histological study, the authors compared calcium sulfate (Osteoset), ultraporous β-TCP (Vitoss), and silicated calcium phosphate (Actifuse) in the grafting of osteochondral defects in the subchondral bone of the femoral condyle of rabbits. The authors compared the response according to histologic parameters from one to 12 weeks.96 They noted rapid resorption of calcium sulfate, which elicited an inflammatory response and left the defect site empty before significant quantities of new bone were formed. Both β-TCP and Si-CaP scaffolds supported early bone apposition. They found, however, that β-TCP degradation products provoked an inflammatory response that impaired and reversed bone apposition. They stated that the rapid graft resorption of β-TCP impaired new bone growth through dissolution of the scaffolding and through inflammation-related retardation. They concluded that Si-CaP appeared to provide a more stable osteoconductive scaffold and supported faster angiogenesis and bone apposition compared with calcium sulfate and β-TCP.
In addition to silicon or bovine collagen, celluloid polymers may act as plasticizers and potential biological inducers for mineral bone grafts. No studies of such compounds have been performed on human bone defects. Biphasic calcium phosphate ceramic particles were plasticized with the polymer hydroxypropylmethylcellulose (HPMC) and then implanted into rabbit femoral defects.97 At eight weeks, the yield strength for the grafted group was significantly higher than for the host trabecular bone tissue. Histology revealed that osteoconduction had occurred. In a canine humerus model comparing calcium sulfate paste (MIIG 115) mixed with HPMC versus MIIG 115 alone, the added HPMC enabled better handling. There was similar progressive resorption and new bone formation on X-ray, and the area of new bone, residual implant, and strength were similar between the two groups.98
In order to obtain the optimal chemical and biological characteristics of the available mineral compounds (i.e. resorption profiles), mixtures of the mineral compounds themselves were developed. In a canine study of diaphyseal fracture defects filled with a granular HA/TCP ceramic, the authors concluded the graft was biocompatible and osteoconductive but not osteoinductive or osteogenic, being unable to promote healing in large fracture defects.99 A combination of 75% calcium sulfate plus 25% calcium phosphate (brushite plus β-TCP) injectable cement called Prodense is now available. In a canine humeral defect model, calcium sulfate pellets (Osteoset) were compared with Prodense. The authors found statistically increased ultimate compressive strength in the Prodense group compared with both Osteoset and normal trabelcular bone at all time intervals.100 The Prodense group also had an elastic modulus statistically closer to bone than Osteoset. They noted that Prodense was resorbed at a statistically slower rate than Osteoset and that there was residual Prodense in all samples at 26 weeks. A review of 13 patients who underwent treatment of aggressive benign bone tumors (aneurysmal bone cysts and giant cell tumors) with grafting with composite 65% HA/35% calcium sulfate found a mean time to consolidation of 18 weeks (range 12–28 weeks). There were two (15.4%) local recurrences, one post-operative fracture (7.7%), and no graft-related complications.101 A retrospective review of 75 patients who underwent bone grafting with 70% HA/30% TCP granules after excision of a benign bone tumor revealed two pathologic fractures (2.7%) and the graft was not fully resorbed at the last follow-up in any patients.102 A prospective study was performed on 34 patients to evaluate 65% HA/ 35% TCP (Ceraform) in the treatment of cavitary bone defects related to benign bone lesions.103 Of the lesions, 70.6% were completely healed, 26.5% were partially healed, and one patient had local recurrence (2.9%). The average time to healing was 19.9 weeks and there were no graft-related complications.Discussion
Only one level III study,71 two level II studies,42,103 and no level I studies have been performed on the use of synthetic mineral bone graft substitutes in the grafting of bone defects created in the treatment of benign bone tumors. The level I data regarding mineral bone graft substitutes comes primarily from the trauma literature. The oncological studies that have been performed indicate that calcium sulfate resorbs too quickly to facilitate appropriate new bone formation and that this quick resorption is associated with an inflammatory response and potential serous drainage that resolves when the graft is resorbed. At the other end of the spectrum, the delayed resorption profile of HA prevents bone ingrowth, which makes this graft a less attractive option.
Many articles describe the grafting of bone defects as the ‘standard of care,’ but no data in the literature describe the true indications for grafting of bone defects. With regard to the size or location of the bone defect, the underlying condition, adjuvant treatment, or host factors, no parameters have been concretely delineated to indicate the need for grafting. Surgeons and scientists base all treatment on the assumption that a surgically created bone defect of almost any size must be filled. A critical interpretation of the literature must focus on the real benefits achieved from a graft, especially in comparison with no graft at all.
The primary goal for bone grafting of non-structural defects is biological healing. The data have proved that mineral bone graft substitutes are osteoconductive and facilitate the body’s own subsequent osteoinductive and osteogenic capabilities. The question arises of whether this osteoconductivity is any greater clinically than the osteoconductivity of no graft at all (where healing is due to marrow blood and hematoma). A number of studies have shown no benefit of grafts. In their level I study, Petruskevicius et al. compared the grafting of tibial bone defects with Osteoset versus no graft at all and found statistically increased bone formation from six to 12 weeks in the no graft versus the grafted group.43 Turner et al.’s study of the canine spine fusion model found statistically decreased bone fusion mass in the calcium sulfate group compared with no graft at all.26 Walsch et al. found increased growth factor staining in calcium sulfate grafts compared with no graft at all, but did not demonstrate any correlation of this staining to new bone formation.24 One canine study of a diaphyseal tibial defect found increased strength and stiffness in the β-TCP grafted group compared with no graft at six weeks, but no differences were found at eight weeks.64 Another canine study comparing two commercially available β-TCP products was unable to find statistical differences in either graft compared with no graft at all in terms of new bone formation, yield force, stiffness, or failure force at any time interval.75 Even the benefits of grafting revealed in the trauma literature are only with regard to maintenance of reduction and stability. No benefits have been found in terms of union or healing rates. Although one must be careful not to commit a type II statistical error and assume that no differences found in low-powered studies equals equivalence, the data have not yet clearly demonstrated results to the contrary.
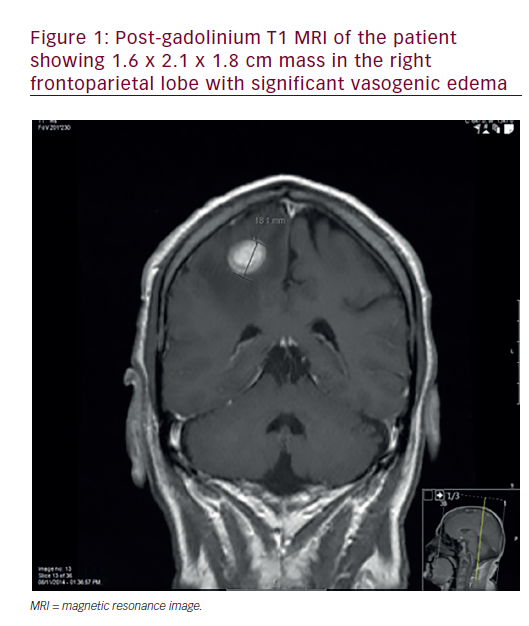
A second issue that arises from a review of the literature is the accuracy of traditional X-ray in evaluating both graft resorption and new bone formation. Differences in penetration or angle can skew image results, so what may appear to be new bone formation may simply be an artifact. Some studies have commented on this phenomenon in their discussion.73,104 CT scanning offers the most accurate and standardized way to measure graft resorption and new bone formation. Petruskevicius et al. picked up on this fact, using CT as the measure in their well-designed study.43 CT evaluation for graft resorption results in the patient being exposed to unnecessary radiation, however, and the minerals in the graft—which are often very similar to the mineral composition of bone—may still mimic the appearance of new bone itself. The third issue that arises from a literature review is whether mineral bone grafts may actually retard the formation of new bone. All agree that the grafts are osteoconductive, but if they interfere with the body’s natural osteoinduction and osteogenesis, they may be causing more harm than good. Numerous aforementioned studies have noted the significant lack of HA resorption, which effectively blocks the formation of new bone. Hing et al.’s histological study suggests that the inflammatory response caused by the rapid resorption of calcium sulfate and possibly β-TCP biologically interferes with new bone formation.96 Again, well-designed studies comparing mineral grafts versus no graft would help elicit the clinical significance of this theoretical effect. The TCP formations of mineral grafts have proved themselves to be the most biologically compatible through their osteoconductivity and more appropriate resorption profiles. Save for the calcium phosphate cements in the case of metaphyseal fractures, however, no TCP graft formulation has proved itself superior in the literature. The informed surgeon is therefore free to make the decision of graft selection based on a number of variables. The costs of these implants can be quite high (up to $385/cc in the case of one graft in the center where the authors of the current paper work) and result in exorbitant fees in the grafting of large (>30cc) defects.
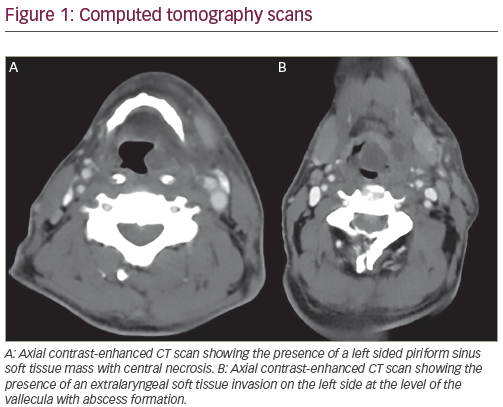
Ease of use is an important variable, since mixing steps (as with calcium phosphate cements) may delay operative times or require inservicing of operating room staff. Ease of administration is very important, since the graft is unable to act as an osteoconductive scaffolding if it does not fill the entire defect. The packing and putty formulations address this need. More recently, injectable vehicles have facilitated the minimally invasive percutaneous grafting of bone defects that may once have required more morbid open surgeries (see Figure 1). The purely mineral liquid injectables (cements) have a working phase that is difficult to handle without a matrix (such as type I bovine collagen, silicon, or HPMC). This can result in graft loss from the defect and messy extravasation into the surrounding tissues.
In addition to biology, the other potential benefit of bone grafting may come from increased mechanical strength. None of the older blocks or granules can achieve compressive strength any greater than that of cancellous bone, but calcium phosphate cements have been able to exceed it. The strength of these calcium phosphate cements is only in compression, however, and this compressive strength is still nowhere near that of cortical bone. The cements still remain weak in shear, tension, torsion, and bending. Most pathologic fractures from bone defects occur during torsional or bending moments over cortical bone defects.1 In this regard, grafting with blocks, granules, or cements does little to prevent pathologic fracture, as evidenced by a post-operative pathologic fracture incidence of up to 7.7% seen in a number of series.33,34,53,74,101
Conclusions
Synthetic bone graft substitutes have evolved in response to the downsides of autograft and allograft. No level I studies regarding their use in the treatment of bone tumors have been performed. The clinical studies that have been performed indicate that calcium sulfate resorbs too quickly and incites an inflammatory reaction, HA resorbs too slowly and blocks new bone ingrowth, and β-TCP and mineral bone graft composites have the biochemical profile that is most compatible with new bone formation. These studies also indicate that all of the mineral grafts are safe and may be as effective as other graft options. Radiographic interpretation of graft resorption and new bone formation may, however, be inaccurate, and no evidence exists to suggest that mineral bone graft substitutes are biologically or mechanically superior to no graft at all. The trauma literature has yielded numerous level I studies indicating that calcium phosphate cements result in increased metaphyseal fracture stability. These studies have not yet detected any improvement in bone healing rates with use. Prospective randomized clinical trials in the treatment of bone tumors comparing bone graft substitutes versus other grafts (autograft and allograft), versus each other, and versus no grafting at all are necessary to properly delineate the real indications for bone grafting and to demonstrate the graft’s efficacy in this regard.