Q. What are phosphopeptide tumor targets and why are they good candidates for vaccine and cell therapy development?
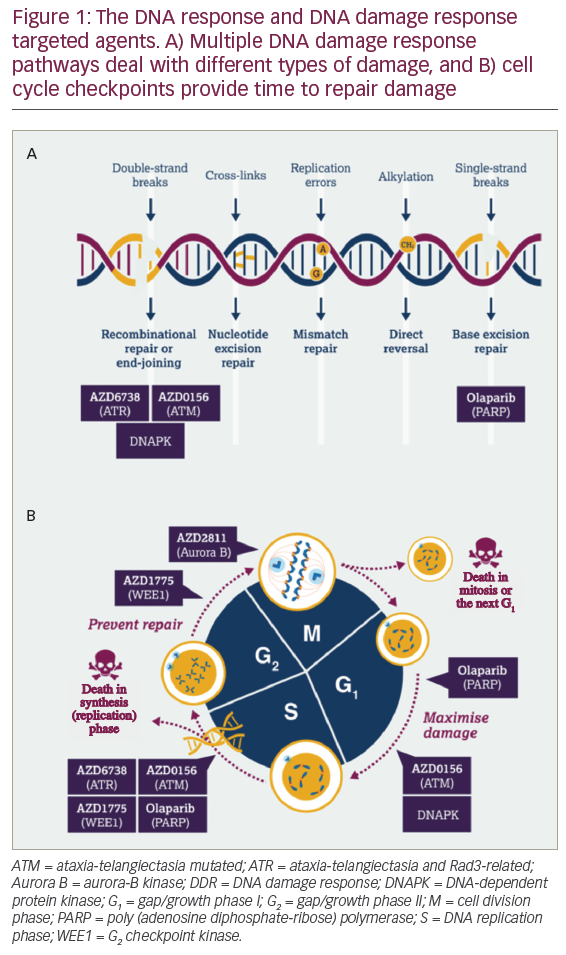
PTTs are a novel class of neoantigen. They are portions of aberrantly phosphorylated proteins that are presented at the cell surface to the immune system in the context of human leukocyte antigen (HLA) class I molecules. These PTTs arise within a cell as a result of dysregulated cellular signaling which is a hallmark of cancerous cells. Protein phosphorylation plays a key role in cellular signaling, and in normal cells this process is tightly regulated by enzymes which add or remove a phosphate group, leading to control of processes such as cell growth, division, survival etc. In the case of cancer cells, this process becomes dysregulated, leading to aberrant and uncontrolled phosphorylation, uncontrolled cellular signaling, and ultimately, cancer development. These abnormally phosphorylated proteins are degraded, resulting in a subset of abnormally phosphorylated peptides presented at the cell surface. These are the targets that we are investigating for novel cancer immunotherapies.3
PTTs are attractive candidates for immunotherapeutic development because they are specifically found in cancer cells, allowing the immune system to distinguish a cancer cell from a healthy cell. Additionally, they are thought to be widely applicable to a large patient population; many are present in at least 50% of patients with a single type of cancer, making them ideal for use in off-the-shelf therapies. Finally, they are believed to be immunogenic, i.e., capable of stimulating an immune response. T cells can recognize these PTTs as a sign that the cells presenting them are abnormal, leading to the specific killing of those cells.
Q. How many phosphopeptide tumor targets have been identified and how many are being used for vaccine development?
We have analyzed many patient tissues, representing different cancer types and different disease states, as well as various normal tissues. Through this analysis and prior work at the University of Virginia and elsewhere, nearly 3,000 unique phosphorylated peptides that are presented to the immune system have been identified. In order to determine which of these epitopes might make the best targets for development, we have implemented a filtering step in which we evaluate each one based on a set of selection criteria. We analyze which HLA type presents the epitope; HLAs that are more common in the population will be ideal. We also look at prevalence of an epitope among patients with a single cancer as well as across tumor types. We evaluate if the epitope is tumor specific or a tumor associated epitope that is also expressed in normal tissues. We also look at the relation of the proteins to cancer development and progression; we find that many of the PTTs we have identified are from source proteins that are involved in signaling pathways that go awry during the development of cancer. Finally, we evaluate the immunogenicity of the specific epitope. Through this process, we have identified approximately 50 PTTs that represent ideal candidates for further development.
Q. What is the latest status of your research on PSV-acute myeloid leukemia?
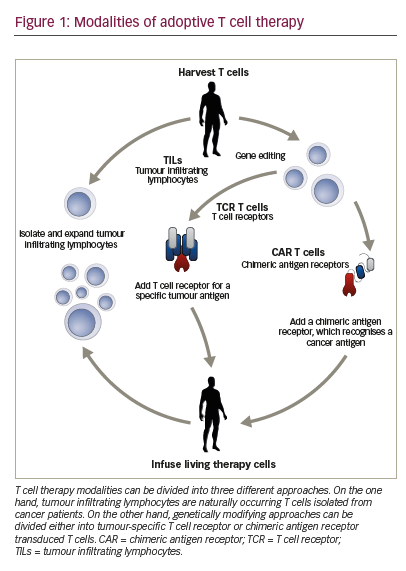
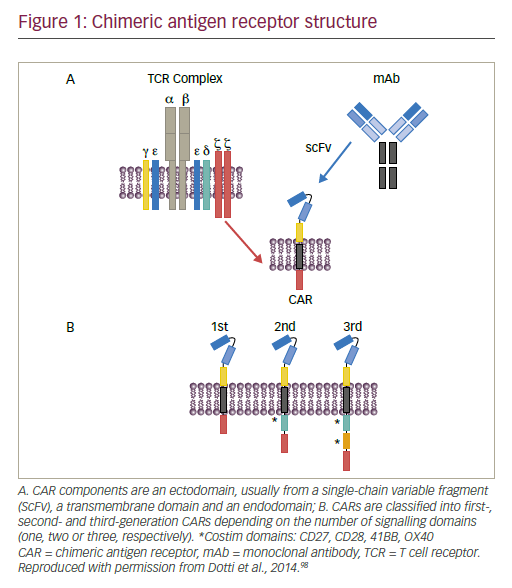
The goal with PSV is to use PTTs to make a tumor more visible to the immune system, training an individual’s own immune system to recognize whether a cell is healthy or not based on the presence of specific PTTs at the cell surface. This is intended to allow killing of the cancerous cells while leaving normal cells unaffected.
Our first candidate is a vaccine containing phosphorylated antigens prevalent in most patients with acute myeloid leukemia (AML). This vaccine has been developed by analyzing the repertoire of abnormally phosphorylated peptides presented on the surface of cancer cells from over two dozen patients with AML. Through this analysis, we identified hundreds of phosphorylated peptides that are presented to the immune system. Next, using the selection criteria described above, we were able to select a subset of PTTs for inclusion in the vaccine. This vaccine is an off the shelf therapeutic that is designed to be widely applicable. Based on the HLA type that we have focused on, about 70% of the US population is expected to be eligible for vaccination. Because of the shared nature of this target class, 95% of eligible patients are expected to express several of the epitopes that are included in the vaccine. By using this multi-epitope approach, we expect to stimulate a broad and robust anti-tumor immune response, minimizing the risk of residual disease and relapse.
Based on our current plans, our first planned product is a first-of-its-kind PTT-targeting vaccine designed to create an immune response in patients with AML and is designed to include antigens represented in 95% of patients with the disease. We are planning to advance our vaccine into the clinic to evaluate safety, immunogenicity and clinical efficacy in combination with other I-O agents.
We have an adjuvant called QS-21 Stimulon™ (Agenus, Lexington, MA, US) that will be co-administered with this vaccine. It is incorporated in the adjuvant system of GlaxoSmithKline’s Shingrix herpes zoster vaccine, which is up to 97% effective.4 We believe that the vaccine efficacy is attributable at least in part to the adjuvant. We don’t see this efficacy with other vaccines; ZOSTAVAX® (Merck, Kenilworth, NJ, USA) that preceded it was around 50% effective.5 This adjuvant helps to boost immune recognition and is intended to combat the tumor with other molecules in our own portfolio.
Q. Which malignancies are most likely to respond to this approach?
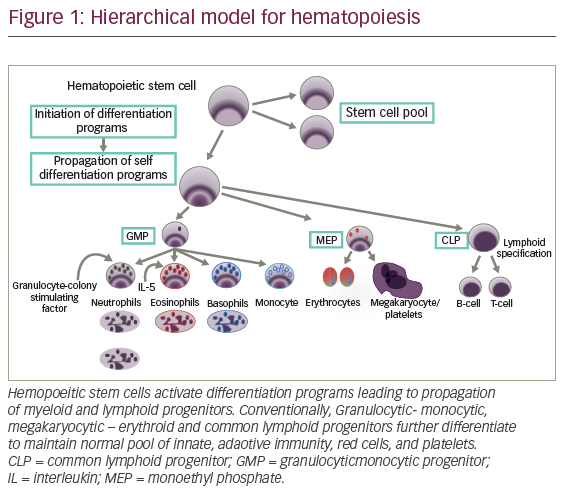
We are focusing on tumors that are good at avoiding immune recognition and therefore are unresponsive or have suboptimal responses. These include colorectal cancer, ovarian cancer, sarcomas, and brain cancers. These are fatal with a poor prognosis and in areas of the body that are difficult to expose them. We aim to adapt them to the innate and the adaptive immune system. We believe that PTTs represent extremely potent targets for vaccines as well as cell therapies and, given that we see the same targets that are prevalent in patients with various types of cancer, we expect that the modalities that we use to target them will be broadly applicable across many different tumor types.
Q. What other vaccines are planned in the future?
PTTs have the potential to treat many cancers. Therefore, we can continue to develop indication-specific vaccines focusing on tumors unresponsive to currently available therapies, such as colorectal cancer, ovarian cancer, sarcomas, and brain cancers. We can also develop this vaccine with representative PTTs that are highly prevalent among patients spanning multiple tumor types. This may allow us to treat a large portion of patients affected by multiple types of cancer. We are actively exploring both of these options.