Radiotherapy (RT) was used clinically for the first time in 1896, and, since then, has evolved impressively, in particular, more recently. Initially, RT was referred to as ‘Röntgen therapy,’ after the discovery of the X-rays by Wilhelm Röntgen in 1895.1 In those early days of RT, external beam RT (EBRT) with superficial kilovolt (kV) X-rays, in addition to treating some malignant diseases, was mainly used to treat various skin diseases through its anti-inflammatory capacities and infectious diseases, such as tuberculosis, due to the supposed antibacterial activity of X-rays.2 As such, RT was widely used in this era before the introduction of antibiotics, chemotherapeutic agents, and steroids. However, for the treatment of cancer, these early EBRT treatments with rather unreliable treatment units often resulted in severe side effects and/or poor local control.
The development of reliable therapeutic X-rays equipment would ultimately take 40 years, until the mid-1930s, however, still using EBRT treatment with low energy (and thus less penetration) X-rays.3 Nevertheless, it was the introduction of the prolonged fractionated scheme by Coutard in those days that allowed such EBRT to provide cancer cure with acceptable toxicity.4 This approach continued until the 1950s, when units with cobalt-60, a synthetic radioactive isotope of cobalt, were able to treat patients with gamma-rays of 1.2 MV (high energy and thus high penetration). The first million volt (super voltage) units, the linear accelerators (linacs), were produced in the US in the 1940s, but it would take until 1953 before the first patient was treated with a linac at the London Hammersmith Hospital.5 In order to avoid losing time with treatment planning in the actual treatment room, ‘simulator’ rooms devoted to treatment planning were built. On a treatment-like machine, treatments could be simulated with the aid of fluoroscopy and 2D radiographs.
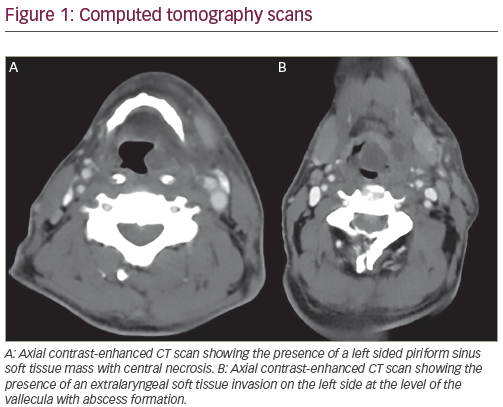
The recent history of EBRT techniques in head and neck cancer (HNC) (see Figure 1) is characterized by the search for the best possible equilibrium between treatment intensification in order to further improve loco-regional control and toxicity reduction (see Figure 2). This is not only true for locally advanced disease but also, or perhaps even in particular, for early stages treated with RT.
The recent history of RT in general and of RT in HNC in particular, starts with the introduction of the computed tomography (CT) scan (Godfrey Houndsfield, 1971) in RT planning in the 1980s. Conventional fluoroscopy-based 2D RT makes room for 3D conformal RT (3D-CRT) (see Figure 3). No longer are the fields determined based on bone anatomy, 3D-CRT makes it possible to contour the target volume (TV) and the organs at risk (OARs) slice by slice and to shape the beams precisely around the contoured TV. All imaginable beam angles can now be used to keep the OARs out of the beam path whenever possible. At the same time, the relatively cheap and reliable cobalt-60 units had been gradually replaced by electricity-driven linacs without a physical radiation source. The acceleration of electrons by high-frequency electromagnetic waves makes it possible to produce photons at higher dose rates and higher energies than the cobalt-60 units. Therefore, these linacs can treat deepseated tumors faster than the cobalt-60 units with a relative smaller penumbra (i.e. the peripheral zone of the beam receiving between 80% and 20% of the prescribed dose) while better sparing the skin.
This more precise administration requested for more precise repositioning. Sandbags, sponge, and tape immobilization was replaced by immobilization devices with head supports and customized thermoplastic masks (see Figure 4), allowing for more precise and faster daily repositioning. In the 1980s and 1990s, the patients were simulated at the RT department but then afterwards they were referred to the radiology department for a CT scan in treatment position. The contouring and the dose calculations were carried out at the RT department.
In the 21st century, however, more and more RT centers have their own CT-simulator. After the CT scan in treatment position is acquired, and the TVs and OARs are contoured, an ‘inverse’ simulation can be performed in the treatment-planning system. In doing so, treatment parameters, such as beam direction and isocenter, for example, are decided upon guided by 3D imaging and by the resulting dose distributions, instead of by simple human judgment.
At the same time, the quality/accuracy of contouring has been improved by delineation atlases (e.g. the Gregoire Lymph node atlases, atlases on the pharyngeal constrictor muscles, etc.) and by the possibility of adding supplementary imaging information to the planning CT.6–9 This supplementary imaging information may be derived from magnetic resonance imaging (MRI) and/or positron emission tomography (PET) scan, for example, preferentially in treatment position. This was made possible by the development of precise fusion software programs. This more precise contouring reduces toxicity as it lowers the volume of unnecessary irradiated healthy tissue and it increases tumor control by reducing the risk for geographical misses.
Intensity-modulated Radiotherapy
In the early 1990s, powerful informatics allowed the development of intensity-modulated RT (IMRT ) in different forms. The inverse planning techniques no longer place fields around the TVs: they ‘shape’ the dose around them.
Another important point for this evolution was the replacement of the custom-made cerrobend alloy shielding blocks (placed between the patient and the head of the machine) by multileaf collimators (MLCs) (see Figure 3). The build-in MLC makes a rapid change in field configuration possible, allowing a subdivision of each beam in multiple smaller fields (beamlets), each of them administering a different part of the total dose to a different volume of the TV (see Figure 3).
As such, IMRT builds up the total prescribed dose stone by stone, beamlet by beamlet, to end up with a more conformal and homogeneous dose distribution to the TVs than with the classic techniques. In the same way, the OARs can be better spared out of the high-dose zone of the TVs whenever possible, reducing acute and late side effects.10–18
Treatment intensification by IMRT can easily be performed by ‘dose painting,’ i.e. the administration of different doses to different adjacent risk zones at the same time (see Figure 5).13 This dose painting permits localized treatment acceleration (or ‘simultaneous integrated boost’) and/or dose-escalation (e.g. dose painting by numbers on the more resistant/aggressive regions visualized on the PET scan).19–21 This might lead to higher tumor control. However, dose painting by numbers is still considered experimental as major problems on volume definition and reposition (in)accuracy still have to be solved. To take into account these geometric uncertainties, new planning techniques, such as probabilistic treatment planning, may be required. This approach does not use a fixed margin for geometric uncertainties (i.e. the planning TV) anymore, but a mathematical model based on expected uncertainties during the course of treatment. The probabilistic planning system builds its own ‘margins’ into the dose distribution, governed by probabilistic planning criteria.22
Despite the widespread use of IMRT in the treatment of HNC, only one randomized trial recently showed superior antitumor efficacy over conventional RT in terms of loco-regional control in nasopharyngeal cancer patients.18,21,23 However, randomized trials do show level I evidence in reducing late xerostomia resulting in an important improvement in the quality of life compared with conventional RT .14–18 Therefore, IMRT is considered standard of care in HNC.
Rotational Intensity-modulated Radiotherapy Techniques
The last few years, static beam IMRT has gradually been replaced by rotational IMRT based on Brahme’s theory of more degrees of freedom resulting in more conformal dose distributions and thus better dose painting.24 There are basically two major ways to perform rotational RT : cone beam and fan beam. The first was introduced in the late 1990s and this rotational technique can be delivered on a conventional linear accelerator with conventional MLC.25
The latter, also referred to as tomotherapy, is specifically designed for IMRT . Serial tomotherapy, the pioneer in IMRT , was introduced somewhat earlier by the NOMOS Corporation (Swickley, Pennsylvania, US) as the PEACOCK system.26 Helical tomotherapy (HT), on the other hand, was introduced much later by TomoTherapy (Accuray, Sunnyvale, US) in 2003 and is delivered by a CT look-alike machine with an accelerator tube instead of the X-ray source.27 With its integrated CT scan it combines helical administered IMRT with high-precision image-guided RT (IGRT ).
All these rotational IMRT techniques are clearly faster than classic static beam IMRT , and planning studies show better dose homogeneity and OAR sparing.28–32 However, there is no hard evidence of their clinical superiority over classic IMRT .33–35
Parallel to IMRT , there has been also the clinical implementation of stereotactic radiation (CyberKnife and linac-based stereotactic RT ) and particle therapy (protons and carbon ions).
Stereotactic Radiotherapy or ‘Radiosurgery’
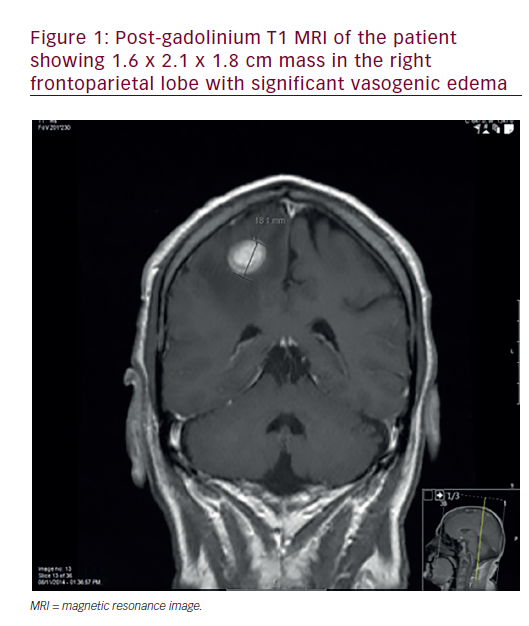
Stereotactic radiotherapy (SRT ) is a nonsurgical procedure that delivers precisely targeted radiation at much higher doses than conventional RT , while sparing the nearby OARs. Indications for fractionated SRT are generally limited to a few (four or fewer) small (3 cm or less) lesions. As such, in HNC SRT is used as a boost after conventional RT or for reirradiation after relapse or second primary in previous irradiated tissue.36
SRT in HNC can be performed by the classic linac (e.g. Novalis, Xknife, etc.) or by the dedicated CyberKnife system. The most spectacular SRT technique is without any doubt the frameless 4D image-guided CyberKnife. The X-ray source is mounted on a robotic arm so that it can move around the central point, irradiating with an enormous degree of freedom. Its accuracy is below 1 mm for static targets and ±2 mm for mobile targets. This accuracy together with its dose gradient, which is even steeper than with IMRT , makes it possible to better spare the surrounding OARs.
In HNC, stereotactic fractionated RT has mostly been reported in smallsized studies in the recurrent disease setting, with variable results due to the heterogeneity of the study populations. Studies about its use as a boost after IMRT are ongoing.36
Particle Therapy or Hadron Therapy
As it is felt by some that photon-based RT may have reached the limits of its possibilities, other particles (re-)gained interest. Most popular are protons and carbon ions, which were first clinically used in 1954 and 1994, respectively.
Both have dose distributions that are superior to any photon technique. In the ‘Bragg peak,’ the typical dose deposit zone of these particles, all the dose is deposed leaving no exit dose. This may be particularly interesting in the treatment of HNC with a lot of radiosensitive OARs nearby (spinal cord, brainstem, parotid, and submandibular glands). Moreover, the absence of exit dose makes dose escalation easier than for IMRT and decreases the risk for secondary cancers, which makes it ideal for the treatment of children. Finally, particle therapy can be optimized to intensity-modulated particle therapy (IMPT) allowing for dose painting and even ‘repainting,’ i.e. online adaptive RT based on the measured delivered dose.36–39
Besides this ballistic advantage, heavy particles or heavy ions (best known are carbon ions) have the supplementary benefit of a higher biologic effect for a given physical dose.38–40 Compared with photons and protons, their energy loss per tissue path length is two to three times higher. This increases the biologic effect, also in radio-resistant cancers (e.g. melanoma, adenoid cystic carcinoma, certain sarcoma subtypes, etc.), which makes these tumors good candidates for carbon ion treatment.41
However, the ballistic characteristics of particle therapy and the added higher biologic effect of carbon ions are counterbalanced by the high investment cost that limits the number of centers worldwide. Miniaturization of particle beam equipment is ongoing and will hopefully resolve this restriction problem.
Also for particle therapy there is no definitive proof of superiority.36,42–45 Several planning studies showed a significantly lower dose to the OARs and some small clinical studies reported early promising results. Nevertheless, with particle therapy some undesirable toxicities have also been encountered.36,45–47 Therefore, further research and assessment of its use is warranted.
Image-guided Radiotherapy
Parallel with the evolution of RT machines and planning systems imaging developed further and was also further integrated into the whole process.
From blurry 2D gammagraphies, image-guided radiotherapy (IGRT ) evolved into orthogonal X-rays and electronic portal imaging IGRT , and developed further into 3D CT scan-based imaging (see Figure 3), and even 4D imaging-based RT . CT-based (‘volumetric’) IGRT mostly gives a much better idea of the soft tissues and the tumor within the patient. In addition, 4D imaging also takes into account the organ motion during treatment e.g. due to breathing.
This evolution not only improves the accuracy of the daily repositioning, reducing the risk for geographical miss, but it also allows for a reduction of the safety margins used to encompass uncertainties in patient’s repositioning and organ motion. Reduction of these margins has a direct impact on the global toxicity of RT .48 Daily IGRT is preferable as it corrects not only for the systematic fault but also for the random fault.49,50 Specific situations, such as high-dose zones near critical organs (e.g. optic nerve/ chiasm, brainstem), re-irradiation, hypofractionation, and tumors of the lower neck, may benefit from specific/more precise imaging protocols. The first two because of the higher impact of a shift; the last two because of the higher risk for movement during the treatment.
Adaptive Radiotherapy
The patient and his/her tumor are liable to change over the 6 to 7 weeks of RT treatment. The patient may lose weight; the tumor might shrink during this period; the OARs might change by radiation. As such, it is hardly to be expected that the reference CT scan/planning at baseline will still reflect the situation after a few weeks of treatment. And yet, many still accept this as the plan for the whole treatment period for practical reasons. With the introduction of the 3D IGRT , the observed changes can no longer be disregarded. Maintaining the patient’s bodyweight with diets and feeding tubes is one way, but even then one can see shrinkage of the tumor and/or the parotids with the latter sometimes moving toward the high-dose zone.51
In addition to changes in OARs, the question is how tumor shrinkage should be interpreted? A concentric shrinkage without tumor cells remaining in the outer ends seems unlikely. Therefore, TV reduction, as such, may be unsafe. However, when an (experimental) dose escalation in the high-risk section of the TV is required, in an attempt to improve loco-regional control, adaptation during the 6- to 7-week course of RT of volume and/or the dose in this dose-escalation zone might be something to consider in order to optimize treatment.52 This adaptation has to be guided by changing information from imaging (CT scan, MRI, and/or PET scan). Nevertheless, the standard minimal prescription dose to the initial high-risk TV should be respected.
Today’s software does not have the capacity to quickly re-contour and re-plan the treatment. Whenever we see an important anatomical change the only solution that often remains is to start the whole process of contouring and planning from the start. A negative aspect of this approach is surely that this might influence the definition of the cut-off value of an ‘important’ change. Therefore, efforts are made for quick (re-)contouring with the help of atlases integrated in the planning systems. A promising new development is the use of deformable image registration software that deforms the initial CT scan and contours to the newly acquired CTscan. Moreover, planning systems themselves become more powerful and faster and get better/more precise calculation algorithms.
Geometric adaptation, i.e. adaptation in function of changed anatomy, is practically feasible but very labor intensive. Dosimetric adaptation, i.e. replanning, based on reconstruction of delivered dose on the daily IGRT CT scan, is still under investigation.
Ultimately, all this should lead to daily adaptation based on the CT scan of the day. Or even better, based on the MRI or the PET scan of the day or on a combination of them all.
Quality Assurance
As RT becomes more and more complicated, quality assurance (QA) is more important than ever. This QA should encompass a clear program of systematic control of the different parts of the treatment but also regular end-to-end tests and external audits. In 2001, the Radiological Physics Center (MD Anderson Cancer Center) found in a phantom study of IMRT in HNC, comparing planned and delivered dose, a 43% failure in obtaining the 5%/3 mm criteria (i.e. the measured dose at a certain point being within 5% or 3 mm of the planned dose).53 In function of the shape/ steepness of the dose-response curves, this may translate into rather large differences in tumor control and/or toxicity.
Peters and colleagues found an impact of QA on the outcome of HNC patients treated with chemo-RT .54 In a large international phase III trial (TROG 02.02) patients with major protocol violations (in total 12%) had markedly inferior freedom from loco-regional failure (54% versus 78%; p<0.001) and survival (50% versus 70%; p<0.001) at 2 years compared with those who were fully compliant from the start. Interestingly, the major protocol violations were highly correlated with the number of patients enrolled at the treatment center (fewer than five patients: 29.8%; >20 patients: 5.4%; p<0.001). This illustrates the importance of experience with this high-tech RT for HNC and is another argument in favor of centralizing HNC in specialized (RT ) centers.55
However, the huge technologic evolution does not (yet) solve the major QA problem of target delineation, the most important factor in today’s RT . Continuous education, educational sessions, intercolleague judgment, and multidisciplinary contouring (e.g. with radiologist and/or head and neck surgeon) are more important than ever in order to avoid geographical miss.45,55
Conclusion
RT techniques have evolved rapidly in the last 2 decades with the introduction of IMRT in different forms in routine practice despite the lack of hard level 1 evidence of a better outcome. However, today IMRT is standard of care in patients with HNC as randomized studies have shown a significant advantage (level 1 evidence) of IMRT over 3D CRT in terms of toxicity. Rotational IMRT is most promising as it is also clearly faster than static beam IMRT .
Fractionated stereotactic RT is an option that can be considered in HNC patients in case of small lesions using it as a boost or in case of re-irradiation. The use of particle therapy with its interesting ballistic capacities is limited due to the cost of equipment. Therefore, large-scale experience is lacking. As such, proton therapy is reserved for tumors near radiosensitive OARs and for children. Carbon ions will be mainly used for radio-resistant cancer types because of the supplementary higher biologic effect. Finally, adaptive RT is promising but needs much more technologic evolution before it can be optimally used.
All these new techniques in RT require a high level of image guidance in order to reach their maximal capacities and to avoid overdose to the nearby OARs and/or underdose of the TVs. A rigorous QA of all the different steps in the irradiation process is essential to make sure that the right dose is administered exactly at the right place. The radiation oncologist of today is strongly assisted by technology but cannot be replaced by it. On the contrary, the recent technical evolution has made human judgment and experience more crucial than ever before.